ISCHEMIC STROKE / PREVENTION
Smoking
Updated on 07/05/2024, published on 20/02/2023
Smoking and risk of stroke
- smoking is classified as a disease (dg. F17 – drug addiction)
- cigarette smoking and passive smoking are both significant independent risk factors for ischemic stroke (1.5-2 fold risk) [Peters, 2013]
- the excess risk of stroke is sex-independent
- the risk depends on the number of cigarettes smoked and the presence of hypertension (Shah, 2010)
- the risk of stroke is twice as high in heavy smokers compared with moderate smokers (< 20 cigarettes/day)
- smoking is also an independent risk factor for silent brain infarcts
- smoking combined with oral contraceptive use triples the risk compared to non-smoking OC users
- smoking also increases the risk of intracerebral hemorrhage (ICH) and subarachnoid hemorrhage (SAH)
- cardiovascular risk is reversible with abstinence
- quitting smoking significantly reduces stroke risk, returning to baseline approximately 5 years after cessation
- significant and early risk reduction occurs in light smokers (<20 cigarettes/day)
- it is essential, however, to avoid all forms of smoking (e.g., including pipe and passive smoking)
⇓
- in patients with stroke or TIA who smoke tobacco, counseling with or without pharmacotherapy (nicotine replacement, bupropion, or varenicline) is recommended to assist with smoking cessation (AHA/ASA 2021 1B-NR)
- patients with stroke/TIA who continue to smoke tobacco should be advised to stop smoking (and, if they are unable to quit, to reduce their daily cigarette consumption)
- patients with stroke or TIA should be advised to avoid environmental (passive) tobacco smoke
- accelerated atherosclerosis and arterial damage explain predisposition to large- and small-vessel strokes
- important contributing factors are:
- carboxyhemoglobinemia
- increased platelet aggregability
- increased fibrinogen levels and impaired endogenous fibrinolysis
- reduced HDL-cholesterol
- direct toxic effects of compounds such as 1,3-butadiene (accelerates atherosclerosis in animal models)
- smoking-induced vasoconstriction
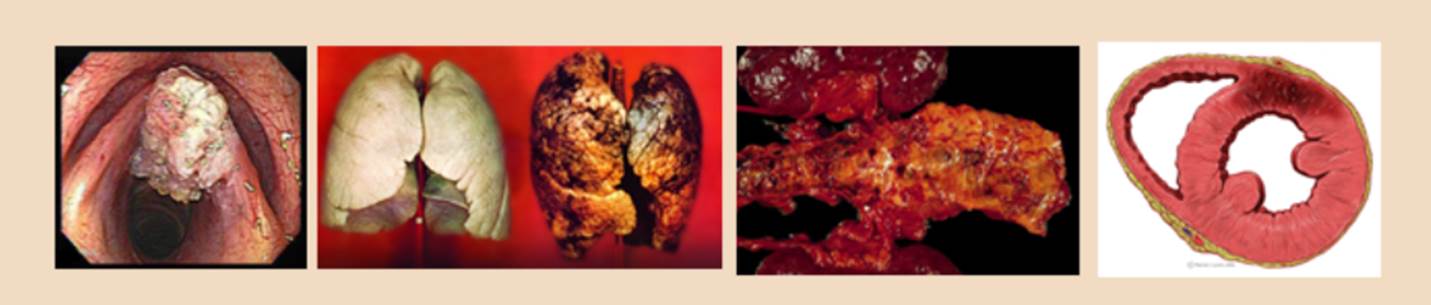
- cancer – tumors of the lung, oral cavity, pancreas, cervix, kidney and bladder, colon and rectum
- skin – affects the tiny arteries of the skin, thereby significantly accelerating the skin aging
- pregnancy – negative effect on the developing fetus (increased risk of miscarriage and congenital developmental defects, lower birth weight)
- risks to children – smoke increases the risk of sudden infant death syndrome, pneumonia, otitis media, and asthma
- other diseases – other diseases and disorders commonly associated with smoking (stomach and duodenal ulcers, earlier development of cataracts, impaired potency and fertility in men, menstrual disorders or infertility in women, psychosomatic disorders, exacerbation/aggravation of chronic diseases)
- after quitting, the following has been demonstrated: (Shah, 2010)
- within 20 minutes, blood pressure drops to the level it was before the last cigarette
- within 8 hours, carbon monoxide levels in the blood return to normal
- within 24 hours, the chance of a heart attack decreases
- within 2 weeks to 3 months, circulation improves, and lung function increases
- within 1–2 months, smoking-related stroke risk due to hypercoagulability normalizes to that of nonsmokers
- within 1–9 months, lungs regain normal ciliary function, reducing infection risk
- in 1 year, the risk of heart disease is cut in half
- in 5 years, stroke risk is reduced to that of a nonsmoker in most cases
- by 10 years, the risk of lung cancer is approximately half that of a smoker. The risks for cancers of the mouth, throat, esophagus, bladder, kidney and pancreas also decrease
- by 15 years, the risk of heart disease is that of a nonsmoker
Smoking and risk of stroke
- stroke patients are advised to quit smoking
- during the period of smoking, the number of nicotine receptors in the brain increases permanently ⇒ people who have been addicted to nicotine cannot be occasional smokers in the future

Regimen arrangements
- evaluate past experiences and learn from them (What helped? What failed?)
- set a D-day; from that day on, total abstinence is required
- identify triggers – negative emotions, company of smokers, alcohol, time stress, craving for tobacco – prepare alternative solutions to overcome them without cigarettes
- do not drink alcohol or coffee, remove tobacco products, ashtrays, lighters, and avoid smoky environments
- get support from friends and family
- consider pharmacotherapy (adequate type and dose)
- suitable for those who smoke > 10 cigarettes per day and/or light their first cigarette within an hour of waking up
Behavioral therapy
- pharmacotherapy should be used as part of a comprehensive smoking cessation program that includes behavioral therapy and support groups to address the psychological aspects of nicotine addiction
Pharmacotherapy
| Smoke cessation methods and their success rates | |
|



