ADD-ONS / ANATOMY
Anatomy of cerebral arteries
Updated on 06/05/2024, published on 10/11/2022
This chapter provides a summary of the fundamental aspects of cerebral vascular anatomy that are essential for stroke physicians and neurosonologists in their clinical practice. Anatomical variants of extracranial and intracranial arteries are discussed in a separate chapter. For more in-depth information on anatomy, refer to resources such as KENHUB
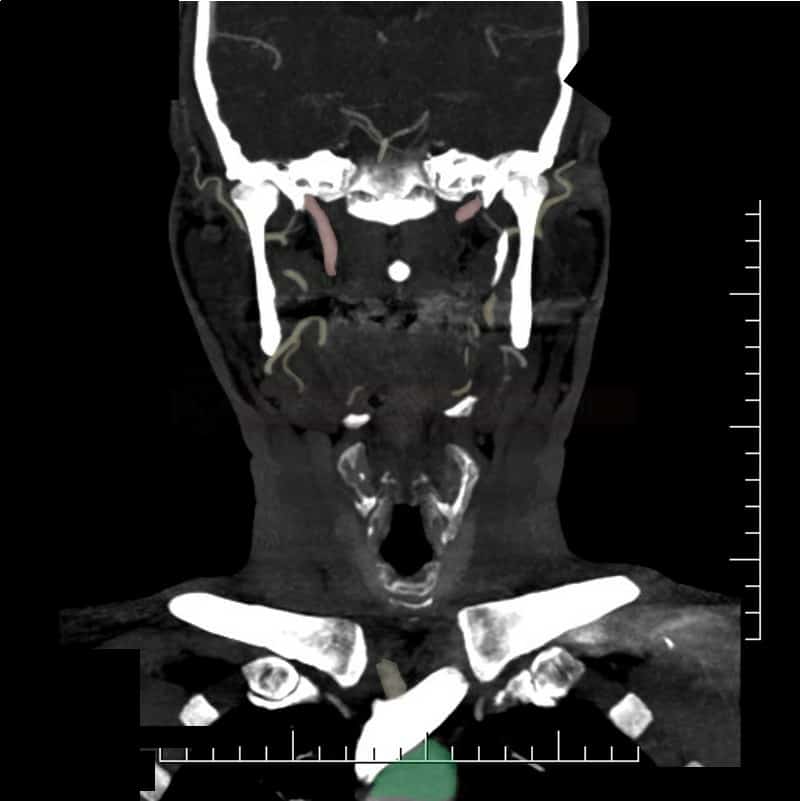
Extracranial cerebral arteries
Extracranial cerebral arteries include:
- brachiocephalic trunk (BCT) or innominate artery
- proximal segments of the subclavian arteries (SA) up to the origin of the vertebral artery
- common carotid arteries (CCA)
- internal carotid arteries (ICA)
- external carotid arteries (ECA)
- vertebral arteries (VA) – from the origin to the atlas (including the atlas loop)
| common carotid artery | 6-7 mm |
| internal carotid artery | 4-5.2 mm |
| vertebral artery | 3-4 mm |
| ophthalmic artery | 1 mm |
Anterior circulation
- the common carotid arteries (CCA) have distinct origins but follow symmetrical courses
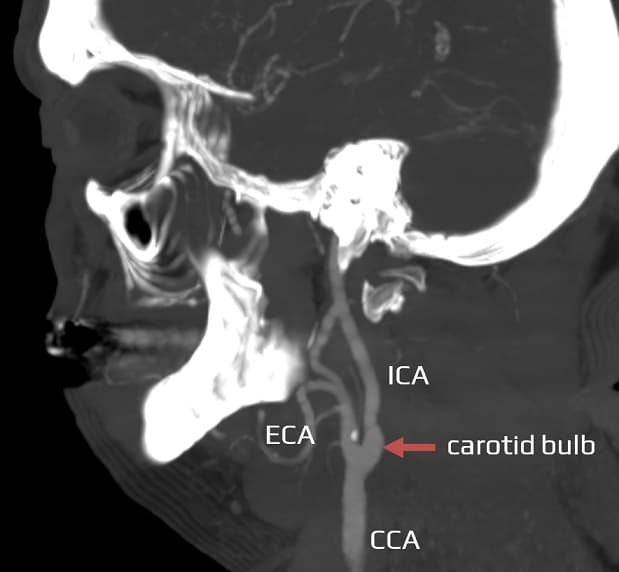
- the CCA typically bifurcates at the C4 level (within the C3-C5 range, at the upper border of the thyroid cartilage) into:
- internal carotid artery (ICA)
- usually situated dorsolateral to the ECA; its origin is enlarged, forming the carotid bulb or sinus with the carotid body
- has no branches in the neck
- enters the skull via the carotid canal, situated anteromedially to the jugular foramen
- external carotid artery (ECA)
- internal carotid artery (ICA)
- the level of bifurcation may be found higher (at the C2-3 level) or lower (at the C6-7 level), and it may be asymmetrical
- the ECA typically has 8 branches:
- ventral
- superior thyroid artery (a.thyreoidea superior) – arises from its anterior aspect; the first branch visible on ultrasound
- lingual artery (a.lingualis)
- facial artery (a.facialis)
- dorsal
- occipital artery (a. occipitalis) – common feeding artery in dural AV fistula (DAVF)
- posterior auricular artery (a.auricularis posterior)
- medial
- ascending pharyngeal artery (a.pharyngea ascendens)
- the ECA terminates as two branches
- maxillary artery (a.maxillaris)
- superficial temporal artery (STA) (a.temp. superficialis)
- ventral
- ACE branches help to differentiate the ICA from the ECA on the ultrasound
- anastomoses:
- superior thyroid artery → inferior thyroid artery (originating from the thyrocervical trunk of the subclavian artery)
- terminal branch of the facial artery → ophthalmic artery (from the ICA)
- posterior auricular artery → occipital artery
- branches of the superficial temporal artery → lacrimal and palpebral branches of the ophthalmic artery
Posterior circulation
- the subclavian artery (SA) originates from the brachiocephalic trunk on the right side and directly from the aorta on the left side
- the vertebral artery (VA) usually originates from the SA
- in ~ 5% of cases, the left VA may originate directly from the aortic arch
- dominance of the left VA with right-sided hypoplasia is common
- extracranial segments (V0-3):
- V0 – origin
- V1 (preforaminal segment) – segment preceding entry into the transverse foramen (this most commonly happens at the C6 level)
- V2 – intraforaminal segment
- V3 – atlas loop (C2-dura)
Intracranial cerebral arteries
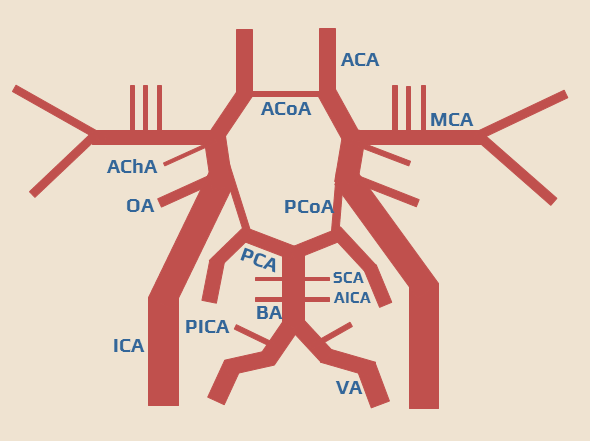
Anterior circulation
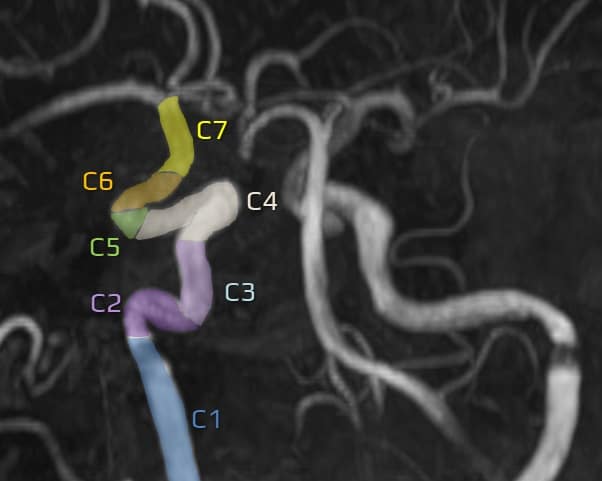
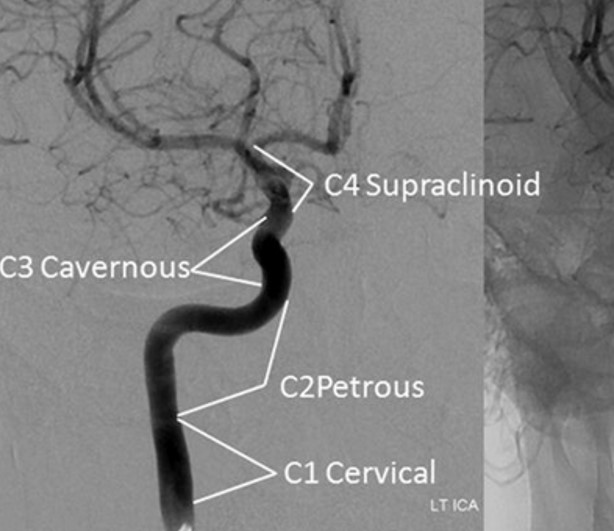
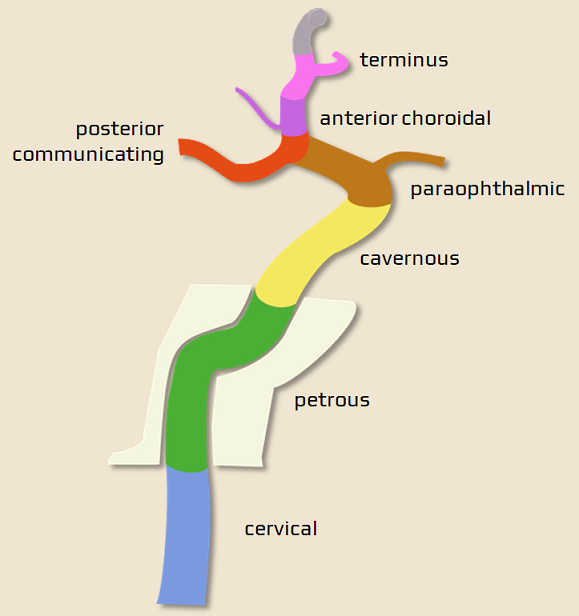
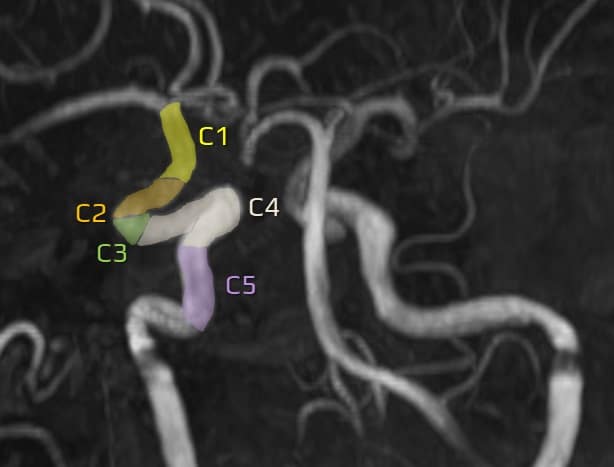
Internal carotid artery (ICA)
- the internal carotid artery (ICA) typically runs posteriorly, laterally, or posterolaterally to the ECA
- the ICA enters the skull via the carotid canal (C1, extracranial segment)
- subsequently, it turns anteromedially to form the C2 (petrous) segment and traverses the petrous portion of the temporal bone
- within the petrous segment of the temporal bone, the artery runs medially
- it gives off small branches to the middle ear cavity (caroticotympanic arteries)
- caroticotympanic arteries anastomose with the anterior tympanic branch of the internal maxillary artery and the posterior tympanic branch of the stylomastoid artery
- ICA exits the carotid canal superiorly (C3, lacerum segment)
- subsequently, it turns anteriorly and enters the medial part of the cavernous sinus (C4, cavernous segment)
- the artery then turns superiorly (C5, clinoid segment)
- ultimately, it turns posteriorly along the anterior clinoid process, continuing as the C6 (ophthalmic) segment
- the ophthalmic artery arises from this segment and enters the orbit along the optic nerve via the optic canal
- the terminal ICA (C7 segment) begins proximal to the origin of the PComA
- distal from the ophthalmic artery, the posterior communicating artery (PComA), and the anterior choroidal artery arise (AChA may originate from MCA)
- the terminal segment bifurcates into the anterior cerebral artery (ACA) and the middle cerebral artery (MCA)
- there are several classifications of ICA segments (see tab); it is advisable to use descriptive terms rather than simple labels (C1-7)
Middle cerebral artery (MCA)
- the middle cerebral artery (MCA) is (along with the ACA) a terminal branch of the internal carotid artery (ICA)
- the MCA supplies numerous deep brain structures, a significant portion of the lateral surface of the cerebral hemispheres, and the temporal pole of the brain
- MCA travels from the base of the brain through the lateral sulcus (of Sylvius), terminating on the lateral surface of the brain; surgical classification divides the MCA into four segments (M1-M4)
- M1 (sphenoidal/horizontal/Sylvian) segment – originates at the terminal bifurcation of the ICA, travels along the posterior margin of the lesser wing of the sphenoid bone, and typically has 2 terminal branches
- MCA gives off small arteries penetrating the anterior perforated substance (lateral lenticulostriate arteries), which supply the anterior part of the thalamus, internal capsule, and basal ganglia
- MCA communicates with the posterior cerebral artery (PCA) via the posterior communicating artery (PComA)
- originally, the genu of the MCA was considered to be the end of the M1 segment (the bifurcation usually starts here but can be placed more distally) = it is more practical to use the bifurcation as a distal border of the M1 segment
- M2 (insular) segment begins at the point of MCA bifurcation (or genu) and includes the superior branch (supplying the frontal lobe) and the inferior branch (supplying the temporal lobe). It gives off insular and temporal branches and terminates at the level of the circular sulcus of the insula
- in addition to 2 symmetrical branches, there are variants with dominance of the upper or lower branch, or 3-4 branches can be detected (< 10%)
- M3 (opercular) segment – ascends toward the surface of the brain, traversing the inner surfaces of the parietal and temporal portions of the insular operculum and reaching the surface of the Sylvian fissure
- M4 (terminal, cortical) segment – starts at the external surface of the Sylvian fissure and extends over the convexity of the hemisphere
- precentral, central, postcentral, and other cortical branches
- precentral, central, postcentral, and other cortical branches
- M1 (sphenoidal/horizontal/Sylvian) segment – originates at the terminal bifurcation of the ICA, travels along the posterior margin of the lesser wing of the sphenoid bone, and typically has 2 terminal branches
- anterior commissure
- internal capsule
- caudate nucleus, putamen, globus pallidus
- temporal pole, insula, lateral aspect of the orbital surface of the frontal lobe, opercular surfaces of frontal, parietal, and temporal lobes, inferior and middle frontal gyri, precentral and postcentral gyri, superior and inferior parietal lobules, superior, lateral surface of the temporal lobe, superior part of the lateral surface of the occipital lobe
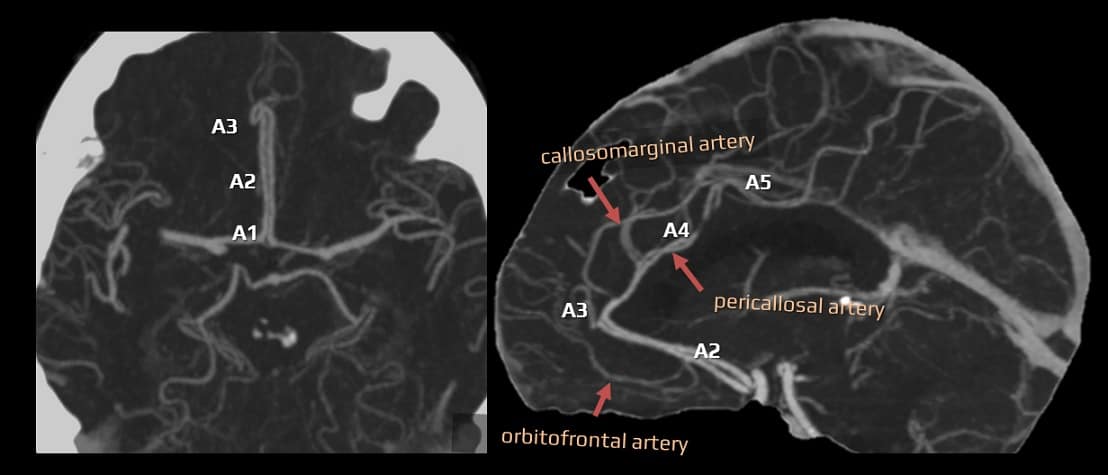
Anterior cerebral artery (ACA)
- the anterior cerebral artery (ACA) is a terminal branch of the ICA
- it supplies the medial aspect of the cerebral hemispheres up to the parietal lobe
- the left and right anterior cerebral arteries are connected by the anterior communicating artery (AComA), forming the anterior portion of the circle of Willis
- the ACA is divided into 5 segments:
- A1 segment (horizontal/precommunicating) originates from the ICA and extends to the AComA
- medial lenticulostriate arteries – arise from the A1 segment and supply the globus pallidus and the medial portion of the putamen
- medial LSAa are shorter, thinner, and fewer in number than the lateral lenticulostriate arteries, which arise from the M1 segment of the MCA
- should not be confused with the perforating branches from the A1/A2 junction (including the recurrent artery of Heubner)
- medial LSAa are shorter, thinner, and fewer in number than the lateral lenticulostriate arteries, which arise from the M1 segment of the MCA
- the recurrent artery of Heubner (RAH; AKA the medial striate artery) – the largest perforating branch routinely seen on angiography
- may arise distal to the AComA, at the level of the AComA, or less frequently proximal to the AComA
- 0.8 mm in diameter
- it supplies the head of the caudate nucleus, the medial portion of the globus pallidus, the anterior crus of the internal capsule, the anterior hypothalamus, and the basal nucleus of Meynert
- its occlusion may occur during clipping of the AComA aneurysm
- variants: absent or duplicated/triplicated/quadruplicated
- medial lenticulostriate arteries – arise from the A1 segment and supply the globus pallidus and the medial portion of the putamen
- A2 (infracallosal) segment – extends from the AComA along the rostrum of the corpus callosum to its genu
- orbitofrontal artery arises near AComA
- frontopolar artery
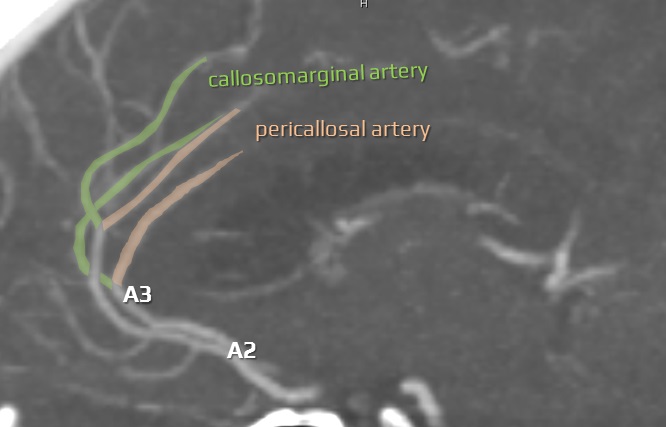
- A3 (precallosal) segment – circumvents the genu of the corpus callosum and bifurcates into callosomarginal and pericallosal arteries (continuation of ACA)
- callosomarginal artery can arise anywhere along the A1-A4 segments; it further branches into the medial frontal arteries (anterior, intermediate, posterior) and the paracentral artery
- occasionally, the A2 segment is very short, and the pericallosal and callosomarginal trunks arise just distal to the AComA; this may look like an ACA “quadrifurcation”
- callosomarginal artery can arise anywhere along the A1-A4 segments; it further branches into the medial frontal arteries (anterior, intermediate, posterior) and the paracentral artery
- 4/5 segment (pericallosal artery) – continues above the body of the corpus callosum
- A1 segment (horizontal/precommunicating) originates from the ICA and extends to the AComA
Ophthalmic artery (OA)
| Content available only for logged-in subscribers (registration will be available soon) |
Posterior circulation
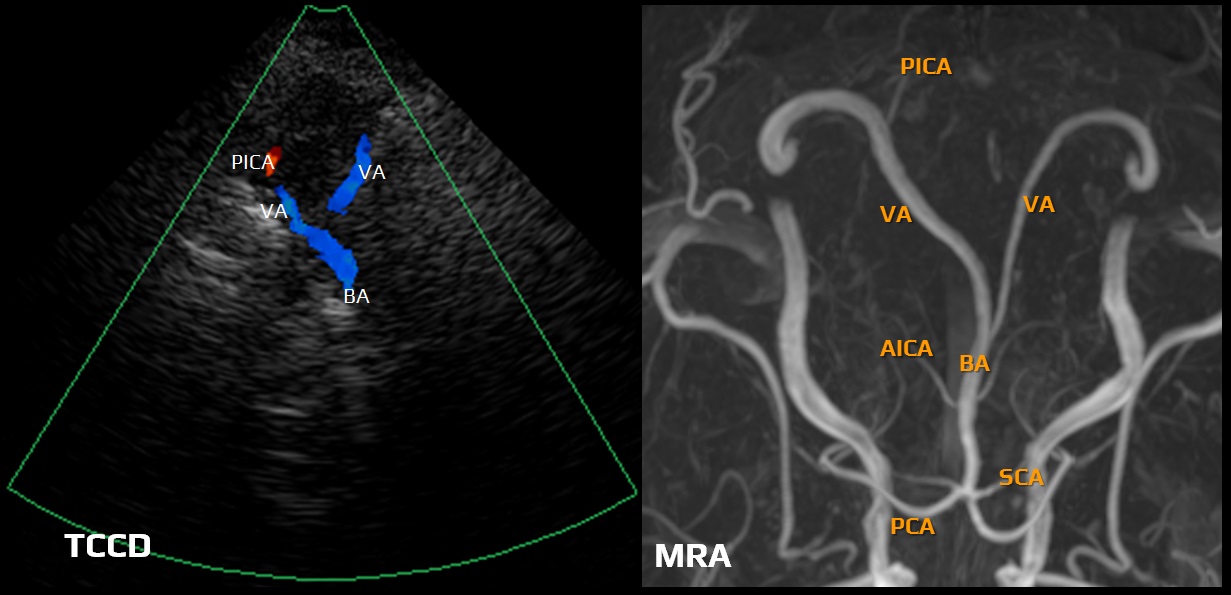
- the posterior (vertebrobasilar) circulation supplies the medulla oblongata, pons, mesencephalon (midbrain), cerebellum, and partially the thalamus
- the posterior (VA-BA) and anterior (ICA) circulations are interconnected via the posterior communicating arteries (PComA)
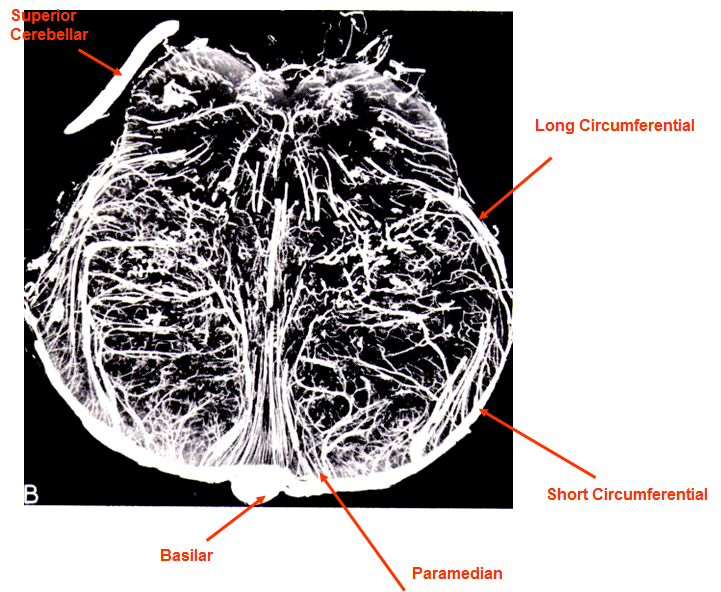
- arteries supplying the brainstem can be divided into anterior (paramedian), lateral (short circumflex), and posterior (long circumflex) perforating branches
- these branches arise from the vertebral arteries, basilar artery (BA), posterior inferior cerebellar artery (PICA), anterior inferior cerebellar artery (AICA), superior cerebellar artery (SCA), and the P1 and P2 segments of the posterior cerebral artery (PCA)
→ clinical presentation of various brainstem syndromes see here
Basilar artery
- an unpaired artery formed by the confluence of the vertebral arteries (V4 segments) located in the pontine basilar sulcus
- branches:
- anterior inferior cerebellar artery (AICA)
- labyrinthine artery (originating from the BA in ~ 15% of cases) – accompanies CN VIII through the internal acoustic meatus to the inner ear; most commonly, it originates from AICA
- superior cerebellar artery (SCA) – arises from the rostral portion of the basilar artery, just below the PCA
- perforating arteries supplying the brainstem
- BA terminates by branching into posterior cerebral arteries (PCAs)
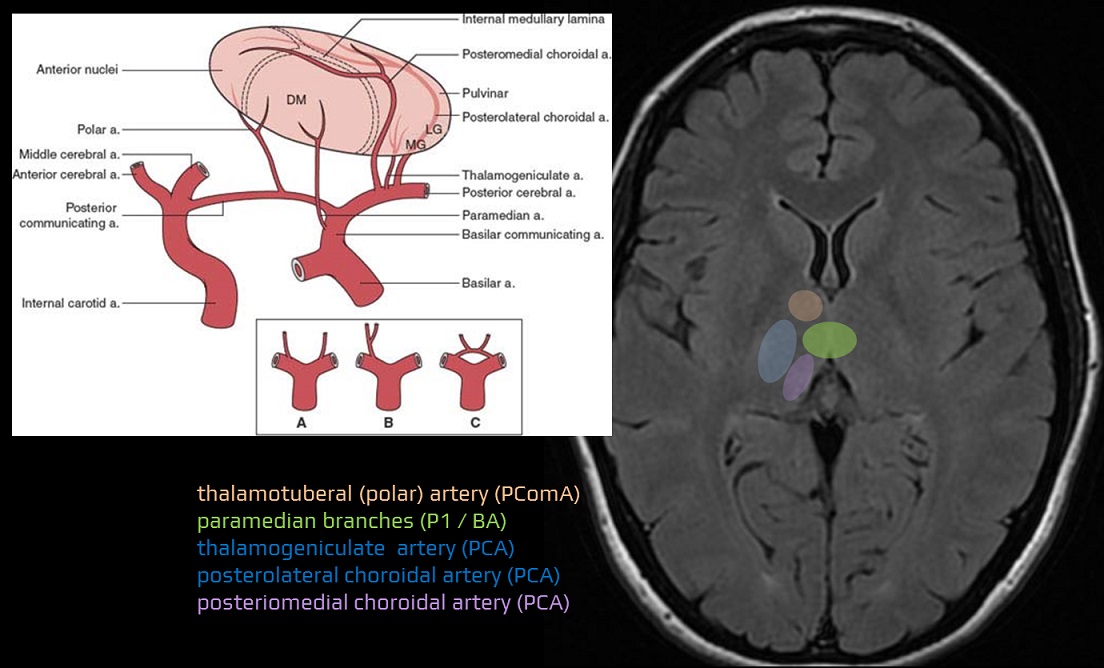
Posterior cerebral artery (ACP)
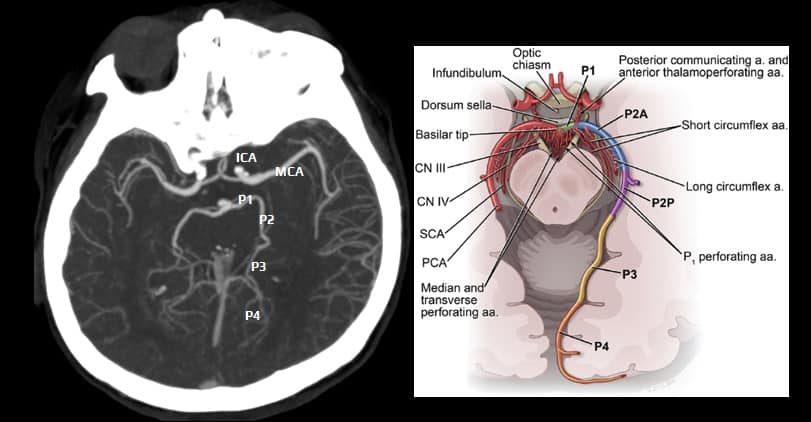
- posterior cerebral artery (PCA) is a terminal branch of the basilar artery
- the PCA crosses the oculomotor nerve, curves around the cerebral peduncle, and ascends above the tentorium to supply the inferomedial temporal lobe and the occipital lobe (including the visual cortex)
- P1 segment (precommunicating)
- originates at the termination of the basilar artery and ends at the origin of the PComA
- occlusion of the P1 segment (proximal to the PComA) leads to infarction of the cerebral peduncle, thalamus, medial temporal, and occipital lobes
- P2 segment (post-communicating)
- P3 segment (quadrigeminal) and P4 segment (cortical)
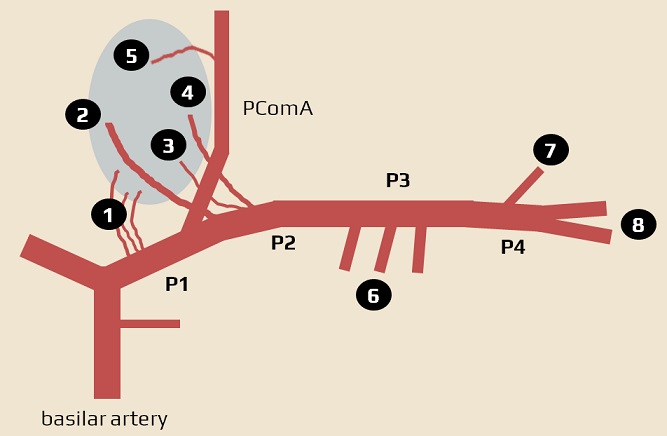
1 – thalamo-subthalamic arteries (paramedian branches), 2 – posteromedial choroidal arteries, 3 – thalamogeniculate artery, 4 – posterolateral choroidal arteries, 5 – polar (thalamotuberal) artery, 6 – temporal branches, 7 – occipitotemporal artery , 8 – parieto-occipital artery and calcarine artery
- main subcortical branches (P1/P2 segment)
- thalamo-subthalamic arteries (paramedian branches)
- these branches may arise from only one PCA supplying both thalami (bilateral infarction occurs when such PCA is occluded)
- posteromedial choroidal arteries
- thalamogeniculate artery
- posterolateral choroidal arteries
- thalamo-subthalamic arteries (paramedian branches)
- main cortical branches
- temporal branches
- anterior inferior temporal artery (AITA)
- middle inferior temporal artery (MITA)
- posterior inferior temporal artery (PITA)
- anterior inferior temporal artery (AITA)
- occipital branches
- calcarine artery (CA)
- parieto-occipital artery (PoA)
- splenial artery
- calcarine artery (CA)
- temporal branches
Vertebral artery (VA)
- hypoplasia (usually on the right side) is a common anatomical variant
- important branches:
- posterior inferior cerebellar artery (PICA) (may also originate from the BA)
- anterior and posterior spinal arteries → Blood Supply of the Spinal Cord
- atherosclerosis typically affects the V0 and V4 segments
- dissection predominantly occurs in the V3 segment
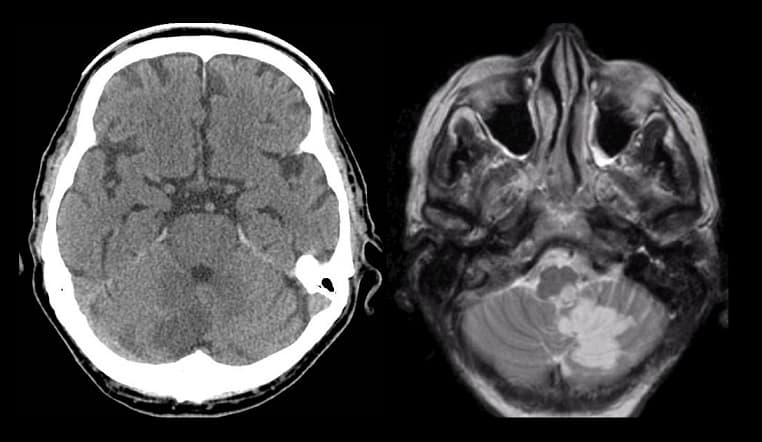
Posterior inferior cerebellar artery (PICA)
- usually arises from the VA; anatomic variants are common
- segments:
- anterior, lateral, and posterior medullary
- supratonsillar
- branches
- perforators in the anterior and lateral segments
- branches supplying the tonsil and the lower vermis (originating from the supratonsillar segment)
- etiopathogenesis of stroke in the PICA territory
- thromboembolism from proximal VA stenosis (usually V0 segment)
- thromboembolism or hypoperfusion caused by a distal VA stenosis (typically in the V4 segment)
- thromboembolism or hypoperfusion caused by the VA dissection (V3 segment)
- embolization from the heart or aortic arch
- clinical presentation
- cerebellar infarction with ataxia and vertigo (usually due to a concurrent brainstem lesion)
- lateral oblongata syndrome (Wallenberg syndrome)
- the most common posterior circulation ischemic stroke syndrome
- symptoms result from damage to the lateral segment of the medulla, posterior to the inferior olivary nucleus
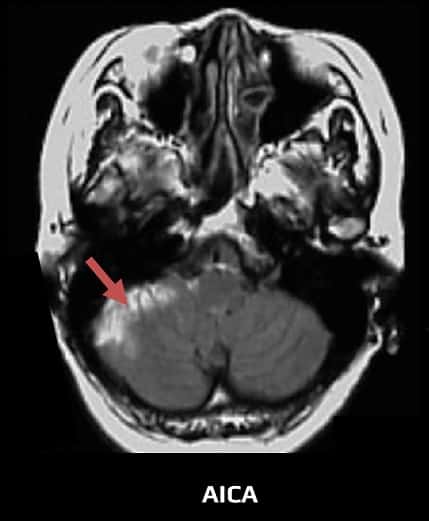
A.cerebelli inferior anterior (AICA)
- the anterior inferior cerebellar artery (AICA) contributes to the blood supply of the cerebellum
- origin:
- most commonly arises from the proximal segment (lower third) of the basilar artery (75%)
- alternatively, from the vertebrobasilar junction or middle segment of the basilar artery
- the area supplied by the AICA is variable and usually includes:
- middle cerebellar peduncle
- pons
- flocculus
- the anteroinferior surface of the cerebellum
- cranial nerves VII and VIII (via internal auditory branch = labyrinthine artery)
Superior cerebellar artery (SCA)
- the superior cerebellar artery (SCA) originates from the rostral portion of the basilar artery, just below the PCA
- it travels along the upper edge of the pons, past the crura cerebri, towards the upper surface of the cerebellum
- it supplies:
- the superior cerebellar peduncle and the superior vermis
- the superior surface of the cerebellar hemisphere (to the great horizontal fissure)
- the dorsolateral part of the midbrain and pons (via perforating branches)
- middle cerebellar peduncle
- dentate nucleus
- variants:
- SCA, unlike AICA or PICA, is rarely absent
- duplication (uni/bilateral) or enlarged origin are quite common
Circle of Willis
- intracranially, the basal arteries are interconnected to form the arterial circle of Willis
- it is a heptagon composed of the following components:
- left and right ICA
- left and right A1 segments, connected by an unpaired AComA
- left and right P1 segments
- left and right PComA (connecting the ICA and P1 segment on each side)
- PcomA originates at the anterior perforating substance and runs posteriorly through the interpeduncular cistern
- basilar artery tip
- branches of the circle of Willis also supply the optic chiasm and tracts, infundibulum, hypothalamus, and other structures at the base of the brain
- medial lenticulostriate arteries (from segment A1)
- perforating branches (from the AComA)
- thalamoperforating and thalamogeniculate arteries (from the basilar tip, proximal PCA, and PComA)
- the circle of Willis allows for the redirection of blood flow between both hemispheres and between the vertebrobasilar and carotid circulations
- a complete circle is present in < 30% of patients; individual anatomical variants are common
- different diameters of vessels on the right and left side
- predominance of carotid or vertebral blood flow
- significant asymmetry of the entire circuit
- absence/hypoplasia of one of the arteries
- AComA (~ 1%)
- proximal segment of the ACA (~ 10%)
- absent or hypoplastic PComA (~ 30%)
- AComA (~ 1%)