ISCHEMIC STROKE / ETIOPATHOGENESIS
Stroke and idiopathic inflammatory bowel diseases
Updated on 10/01/2024, published on 16/02/2023
- idiopathic inflammatory bowel diseases (IBDs) are chronic inflammatory disorders of the gastrointestinal (GI) tract with unknown etiopathogenesis. Generallly, idiopathic IBDs include the following forms:
- ulcerative colitis (UC) – characterized by transmural segmental involvement
- Crohn’s disease (CD) – characterized by superficial inflammation without T-cell activation, with humoral mechanisms predominating
- IBD-unclassified (IBD-U)
- ulcerative colitis (UC) – characterized by transmural segmental involvement
- the incidence and prevalence of IBD are increasing worldwide
- IBDs are associated with an increased risk of thromboembolic events (including stroke) (Sun, 2023)
- meta‐analysis indicates that IBD was associated with an increased risk of stroke (OR/RR = 1.21, 95% CI 1.08 to 1.34, I 2 = 83.6%, p < .001) (Chen, 2021)
- the study also showed that CD was more relevant to the risk of stroke than UC
- increased risk of stroke is probably related to inflammatory mechanisms (elevated CRP), as it is also associated with other systemic diseases such as psoriasis, systemic sclerosis, and systemic lupus erythematosus (SLE)
- diagnosis is based on the following:
- clinical presentation
- endoscopic and radiologic findings
- histology
- IBD-related stroke lacks specific features; complete etiologic work-up is required to rule out other etiologies
Etiopathogenesis of complications
- systemic inflammation leads to the production of cytokines and free oxygen radicals
- the exact etiology of IBD remains unclear; however, epidemiologic data suggest multiple associated risk factors, including diet, smoking, and genetic predispositions
- probable mechanisms increasing the risk of stroke and other CV diseases (CVD) include:
- systemic inflammation (leading to inflammation‐mediated premature atherosclerosis)
- intestinal microflora has also been implicated as a potential contributor to CVD
- abnormalities in the coagulation system (→ hypercoagulable state)
- protein C and S deficiency
- high fibrinogen concentrations
- hyperhomocysteinemia [Romagnuolo, 2001]
- antiphospholipid syndrome [Mevorach, 1996]
Clinical presentation
Extraintestinal non-thrombotic symptoms
- non-neurological
- arthritis
- sclerosing cholangitis
- gluten-sensitive enteropathy
- neurological
- peripheral neuropathies
- myelopathy
- myasthenia gravis
Extraintestinal thrombotic symptoms
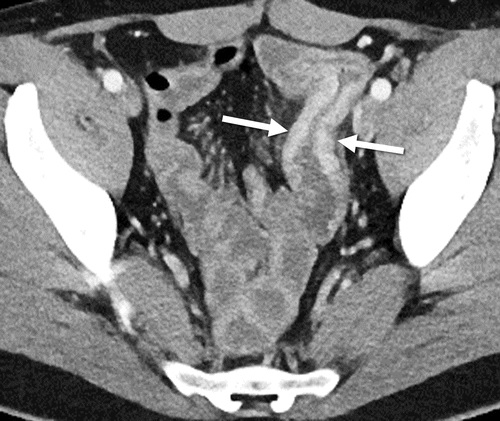
- deep vein thrombosis and/or pulmonary embolism (VTE)
- including venous thrombosis of atypical localization (mesenteric, etc.)
- stroke and cerebral venous sinus thrombosis (CVST)
- mostly due to a hypercoagulable state
- vasculitis is rare
Management
Acute stroke management
- recanalization therapy for eligible patients
- intravenous thrombolysis (IVT) may carry an increased risk of bleeding
- mechanical recanalization or local thrombolysis may be preferred [Brosch, 2012]
- antiplatelet therapy if recanalization therapy is not indicated
Stroke prevention
- the mainstay of prevention includes managing the inflammatory disease and treating traditional vascular risk factors
- low-dose anticoagulation or antiplatelet therapy can reduce thromboembolic risk but may increase the risk of bleeding
- start vitamin supplementation in case of hyperhomocysteinemia


