NEUROIMAGING / COMPUTED TOMOGRAPHY
Computed tomography (CT) in stroke diagnosis
Updated on 02/01/2024, published on 21/03/2021
- computed tomography (CT) is essential in the management of patients with acute neurological deficits
- because of its rapid acquisition and immediate availability of results, it is usually the primary imaging modality used to rule out bleeding and stroke mimics
- magnetic resonance imaging (MRI) may be used in some cases to provide additional data on tissue viability and to assess the underlying cause of the stroke
CT stroke protocol
The following questions should be answered in every patient presenting with an acute neurologic deficit:
- is there an acute ischemic stroke (AIS), intracranial bleeding, or another obvious medical condition (tumor, contusion, etc.)?
- is there any arterial or venous occlusion/stenosis present?
- what is the degree of stenosis or extent of the occlusion?
- what is the current status of the collateral circulation in the presence of an occlusion?
- can recanalization therapy save the affected area?
- a complete CT protocol includes non-contrast CT (NCCT), CT perfusion (CTP), and CT angiography (CTA) and should help answer the above questions to assist in planning recanalization procedures
- NCCT helps identify early signs of ischemia
- CTP provides information about cerebral perfusion, identifying regions of reduced blood flow or ischemia
- CTA visualizes the cerebral vasculature and detects vascular abnormalities, such as arterial occlusions, stenosis, or aneurysms
- NCCT helps identify early signs of ischemia
- advantages of CT over MRI
- CT is faster than MRI; approx. duration of 10 minutes, including CT angiography and CT perfusion
- CT can be performed on agitated patients with severe neurological deficits, ventilated patients, or patients with MRI contraindications (such as those with pacemakers or other metallic implants)
- NCCT results are immediately available; CTA and CTP analysis and processing can be performed after the patient is admitted to the Intensive Care Unit (ICU)
- CT findings specific to ischemic stroke will be discussed below; findings related to intracranial hemorrhage (ICH), subarachnoid hemorrhage (SAH), and cerebral venous thrombosis (CVT) are discussed in relevant chapters
|
CT stroke protocol
|
|
|
NCCT
|
|
|
CTA
|
|
|
CTP
|
|
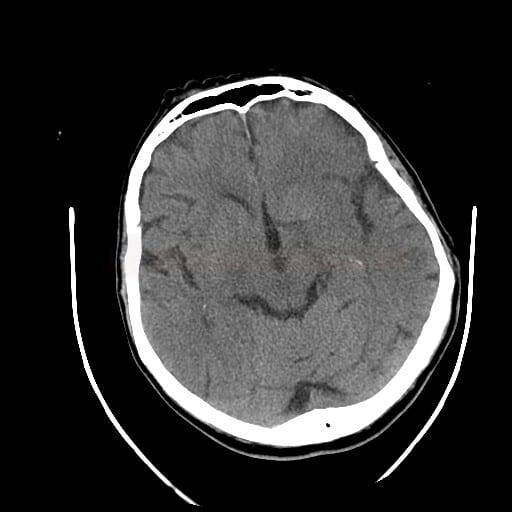
Noncontrast CT (NCCT)
- the primary function of NCCT is to rule out bleeding (for which CT is highly sensitive) and to identify other causes of neurological deficits (such as tumors and trauma)
- the occurrence and extent of ischemic changes depend on the duration of ischemia, arterial occlusion parameters (location, extent of the thrombosis), and the status of the collateral circulation
- typically, parenchymal changes occur within the first 6 hours, indicating ongoing tissue ischemia (early CT signs of ischemia)
- hypodensity develops as a consequence of cytotoxic edema (a 1% increase in water content results in a 2.5HU decrease in density)
- the earlier these signs are observed, the more severe ischemia can be expected
- note the Prévost (Vulpian) sign – conjugate ocular deviation (direction depends on whether cortex or brainstem is involved)
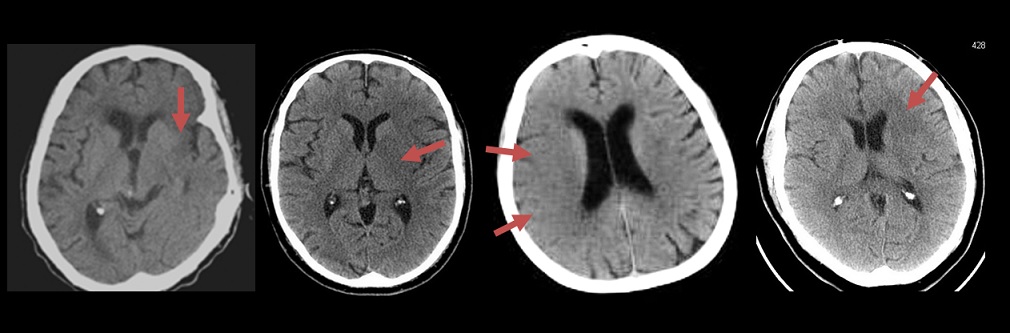
Early CT signs of brain ischemia
- decreased parenchymal X-ray attenuation (cytotoxic edema)
- obscuration of the lentiform nucleus
- loss of distinction between white and grey matter in the cortex
- insular ribbon sign – loss of definition of the gray-white interface in the lateral margin of the insular cortex (insular cortex has the least potential for collateral supply)
- focal hypodensity
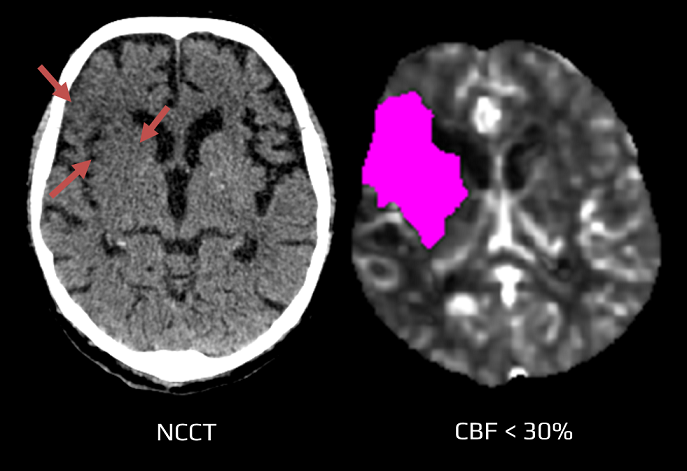
- visible hypoattenuation (not profound hypodensity) does not always represent the core; concurrent CTP may reveal penumbra in such regions
- suggested attenuation ratio (swelling/normal tissue) to identify penumbra is >0.87 (Alzahrani, 2023)
- suggested attenuation ratio (swelling/normal tissue) to identify penumbra is >0.87 (Alzahrani, 2023)
- tissue swelling (mass effect)
- loss of sulcal effacement
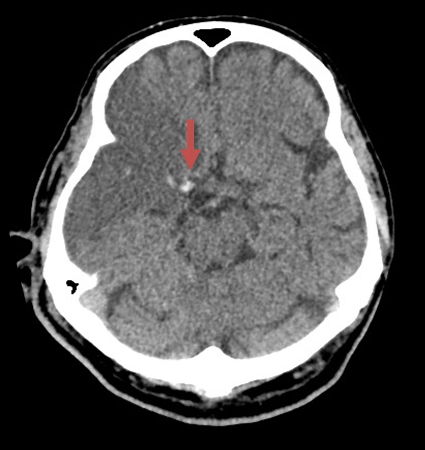
- dense artery sign (DAS)
- direct evidence of thrombosis
- sensitivity for detecting early signs is approx. 70% (range 20-87%), and specificity is 87% (range 56-100%) – the experience of the evaluating physician is crucial
- compare the affected area with the contralateral hemisphere
- adjust window parameters (window/level) to better detect early ischemic changes
- standardized scales were introduced for MCA territory (ASPECTS) and posterior circulation (PC-ASPECTS)
- assessment of early CT signs in the posterior circulation is less reliable ⇒ MR DWI is preferred
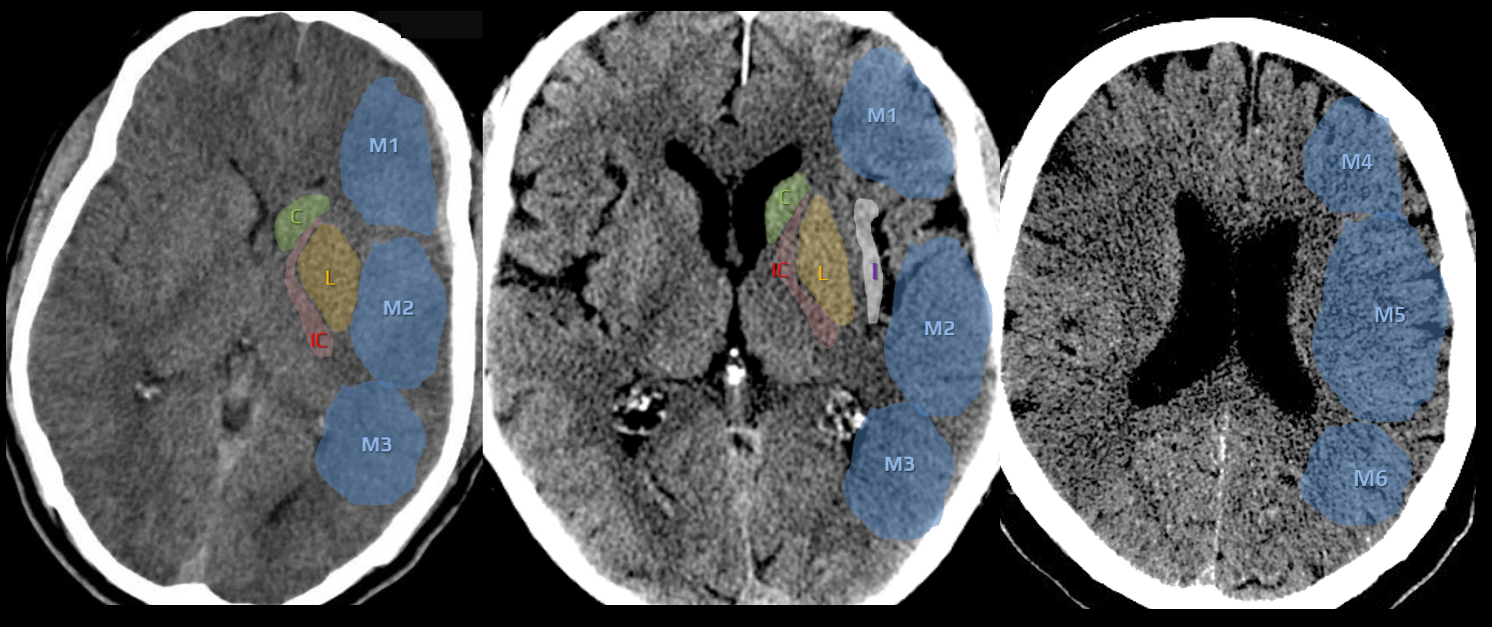
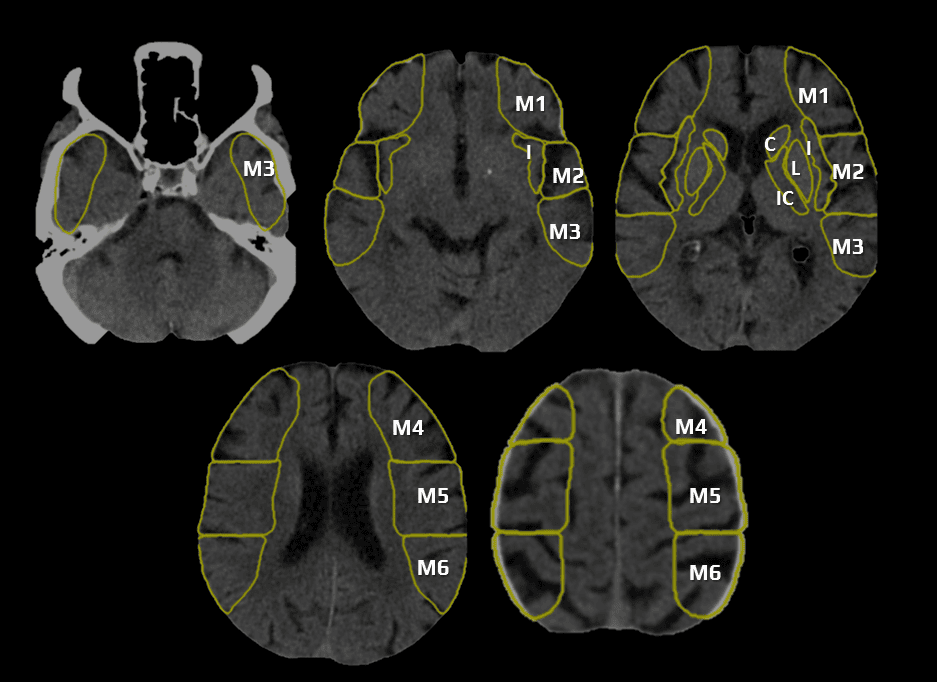
ASPECT score (Alberta Stroke Program Early CT Score)
- the Alberta Stroke Program Early CT Score (ASPECTS) is used to standardize and increase the reliability of detecting early signs of ischemia
- early ischemic changes are defined as incipient parenchymal hypodensity or loss of grey and white matter differentiation
- ASPECTS can be assessed on:
- noncontrast CT (NCCT) – adjust width/level
- CT perfusion (CTP) [Aviv, 2007]
- CTA source images (CTA-SI) [Puetz, 2009]
- noncontrast CT (NCCT) – adjust width/level
- ASPECTS primarily evaluates the MCA territory
- PC-ASPECTS was designed to evaluate changes in the posterior circulation
- commercial software programs for automated ASPECTS evaluation are available (e.g., BRAINOMIX)
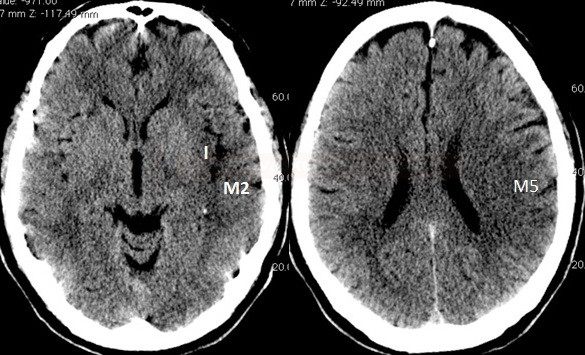
MCA territory
- a 10-point quantitative CT scan score used for evaluating patients with stroke in the MCA territory
- a score of 10 points indicates a normal finding; 1 point is subtracted from the initial score of 10 for each region exhibiting early signs of ischemia
- C – caudate nucleus
- L – lentiform nucleus
- IC – internal capsule (any portion)
- I – insular cortex
- C, L, IC, I, and M1-3 are assessed on axial scans at the basal ganglia level
- M1 – anterior MCA cortex, corresponding to the frontal operculum
- M2 – MCA cortex lateral to the insular ribbon, corresponding to the anterior temporal lobe
- M3 – posterior MCA cortex corresponding to the posterior temporal lobe
- M4-5 are above the basal ganglia at the level of the lateral ventricles (supraganglionic level)
- M4 – anterior MCA territory immediately superior to M1
- M5 – lateral MCA territory immediately superior to M2
- M6 – posterior MCA territory immediately superior to M3
- ASPECTS is a valuable technique for prognostic evaluation in acute ischemic stroke (thresholds may vary slightly between NCCT and CTP)
- patients with high ASPECTS values are more likely to have favorable outcomes
- an NCCT ASPECTS score of ≤ 7 predicts worse functional outcome at three months [Esmael, 2021]
- patients with CTP ASPECTS score of < 8 treated with thrombolysis mainly did not achieve favorable clinical outcomes [Aviv, 2007]
- the threshold for thrombectomy is gradually decreasing (probably ASPECTS 3 based on SELECT2, ANGEL ASPECT trials results) ⇒ ASPECT score will lose some of its importance because most of the patients will be treated anyway
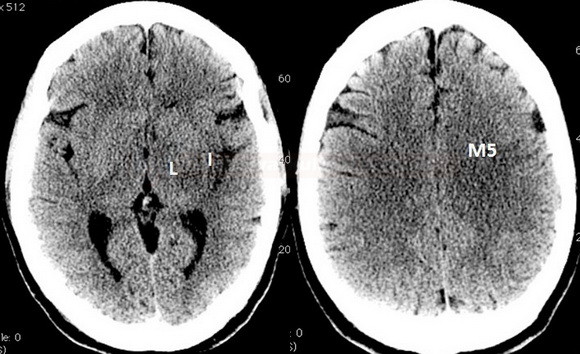
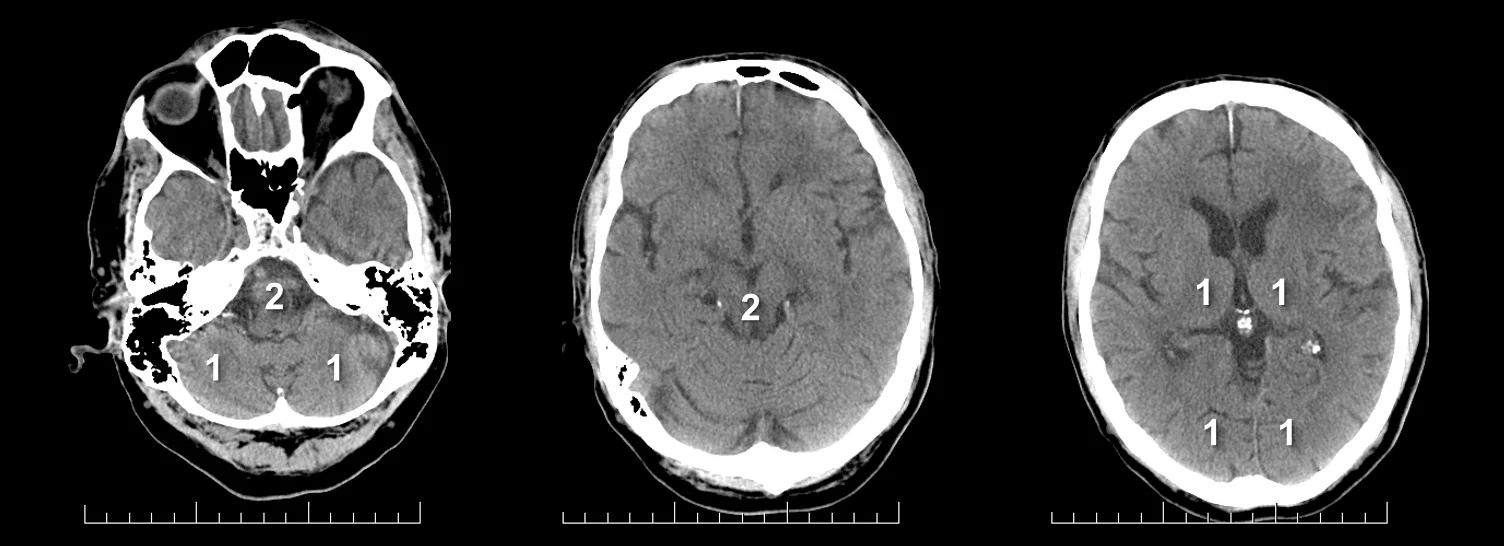
Posterior circulation
PC-ASPECTS (The posterior circulation Acute Stroke Prognosis Early CT score)
- helps to assess early ischemic changes on noncontrast (NCCT) and optionally on CTA source images (CTA-SI)
- normal brain scores 10; points are subtracted for each affected region:
- thalami (1 point each)
- occipital lobes (1 point each)
- midbrain (2 points – uni- and bilateral)
- pons (2 points – uni- and bilateral)
- cerebellar hemispheres (1 point each)
- pc-ASPECTS < 8 is associated with poor prognosis [Puetz, 2009]
- assessing can be inaccurate in the following situations:
- recent ischemia superimposed on an older lesion
- extensive leukoencephalopathy
- poor image quality
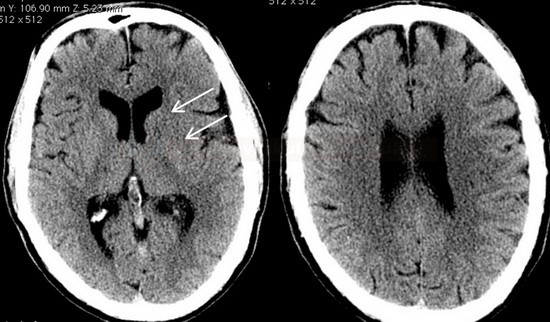
Dense artery sign (DAS)
- increased attenuation at the site of arterial occlusion (caused by thrombus)
- DAS has high specificity but low sensitivity
- the location and approximate extent of the occlusion can be assessed (longer thrombus ⇒ worse response to thrombolytic therapy ⇒ worse prognosis)
- to avoid false-positive results, density should be measured on both sides
- thrombus density > 43 HU
- ipsi- and contralateral MCA density ratio > 1.2 [Koo, 2000]
- thrombus density > 43 HU
- false-positive findings:
- polycythemia
- calcifications
- compare the arteries on both sides; changing the window parameters may be helpful if severe calcifications are present
- try to confirm occlusion on CT angiography
- look for DAS in the peripheral segments (“dot sign“)
- follow the entire course of the ACA, including the A2 segments
- exclude basilar artery occlusion (BAO) in a patient with an altered level of consciousness
Some authors focus on the quantitative and qualitative assessment of thrombus on the NCCT. Thrombus size is predictive of the likelihood of recanalization. In a cohort of 138 thrombolyzed patients with MCA occlusion, none with a thrombus > 8 mm recanalized. Qualitative evaluation of the thrombus with measurement of its density seems to help estimate prognosis and determine stroke etiology. Arterial density is measured on the affected and healthy sides, and their ratio (rHU) is calculated. White thrombi associated with large artery involvement are composed of platelets, atheromatous masses, and relatively fewer erythrocytes. Therefore, they have a lower density than cardioembolic thrombi (in which erythrocytes and fibrin predominate). A lower rHU value predicts a poor response to thrombolytic therapy because white thrombi are more resistant to fibrinolysis


![pc-aspects_prognosis - Puetz pc-ASPECT score predicts prognosis [Puetz, 2009]](https://www.stroke-manual.com/wp-content/uploads/2021/03/pc-aspects_prognosis-Puetz.jpg)