INTRACEREBRAL HEMORRHAGE / VASCULAR MALFORMATIONS
Capillary telangiectasia
Updated on 06/11/2023, published on 24/02/2022
- the second most common vascular malformation after venous angioma (DVA) (16-20% of all malformations)
- the lesion is composed of vessels resembling dilated capillaries (lumen 20-500μm) separated by normal brain tissue (unlike cavernous malformations)
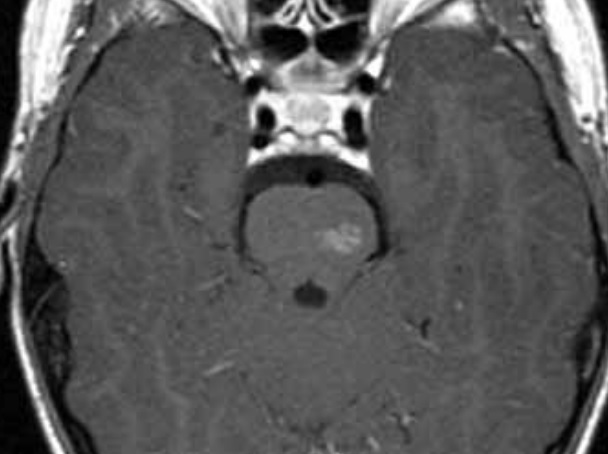
- approx. 2/3 of the lesions have a visible small draining vein
- typical locations:
- pons
- cerebellum
- spinal cord
- the vast majority of telangiectasias are asymptomatic (incidental finding on MRI)
Diagnostic evaluation
- MRI
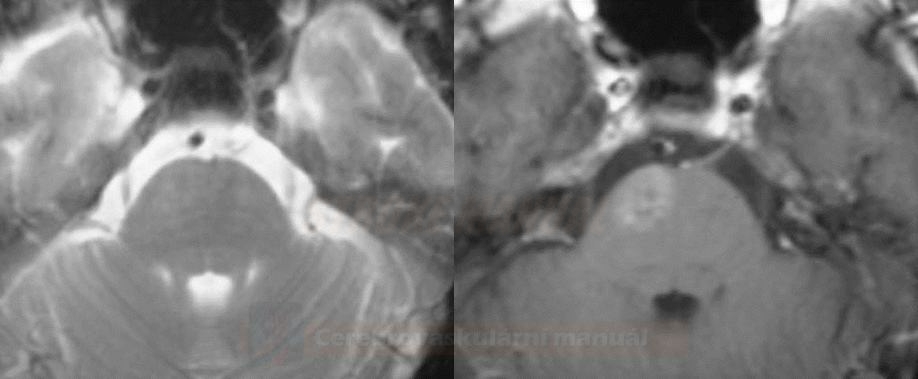
- small, usually solitary lesions without mass effect in typical locations (pons, cerebellum, and spinal cord)
- T1: iso- to a hypointense lesion
- T1C+: enhancing lesion, draining veins may be seen in large telangiectasias
- T2: normal or only slightly hyperintense
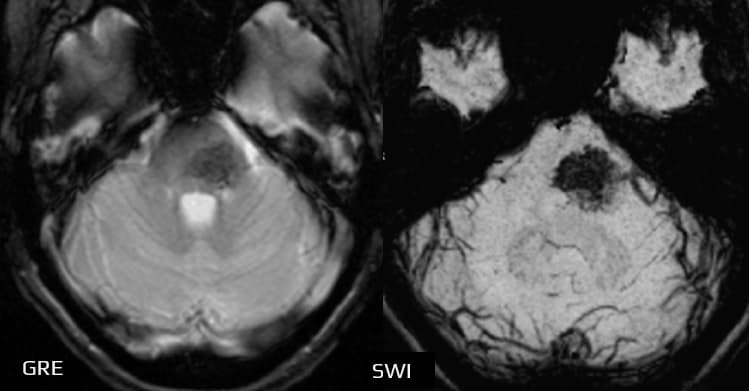
- GRE/SWI: hypointense (low signal caused by slowed flow, not hemorrhage) [Castillo, 2001]
- CT – usually negative or shows a nonspecific small enhancing lesion
- DSA – negative
Differential diagnosis
- tumor or metastasis
- subacute ischemia with hemorrhagic component
- cerebritis
- vascular malformation
Management
- usually conservative approach
- the lesion is difficult to access
- almost always asymptomatic
- MRI follow-up is not required if the imaging is typical