NEUROIMAGING / NEUROSONOLOGY
Extracranial Doppler sonography
Updated on 01/06/2024, published on 22/10/2023
Color Doppler ultrasound of the extracranial arteries is a non-invasive imaging technique helpful in identifying stenosis/occlusion in extracranial vessels → indications for the examination
Ultrasound examination procedure
- if visualization is poor, consider using a convex probe in addition to the linear probe [Todo, 2002]
Visualization in B-mode, color, and power mode
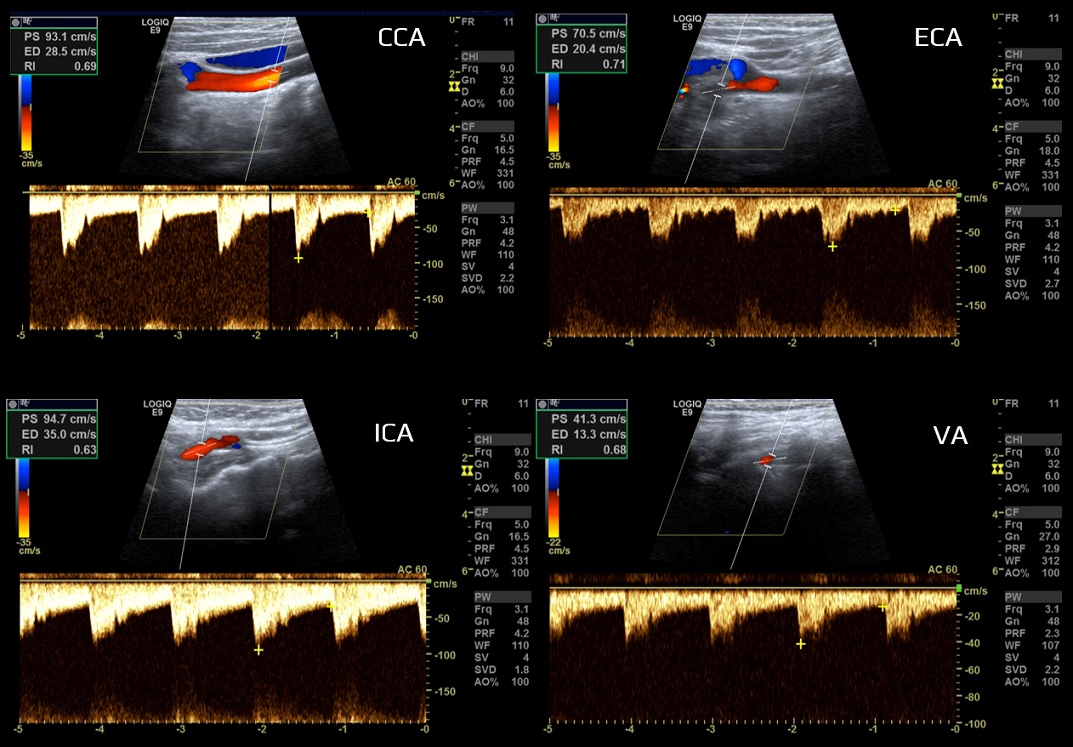
- the following vessels are examined: common carotid artery (CCA), internal and external carotid arteries (ICA and ECA), vertebral artery (VA), brachiocephalic trunk (BCT), and subclavian artery (SA)
- examine each vessel in both longitudinal and transverse section
- measure the diameter of the arteries; the usual values are:
- CCA 6-8 mm
- ICA 4-5.5 mm
- VA 3-5 mm
- assess the course of the arteries (normal, kinking, coiling)
- detect potential atherosclerotic plaques and assess their size (plaque width + artery stenosis) and morphology → Assessment and classification of atherosclerotic plaques
- detection of other pathology
- dissection
- (pseudo)aneurysm
- thrombus
- carotid artery web
- dissection
- in the absence of plaque, intima-media thickness (IMT) should be measured (see below)
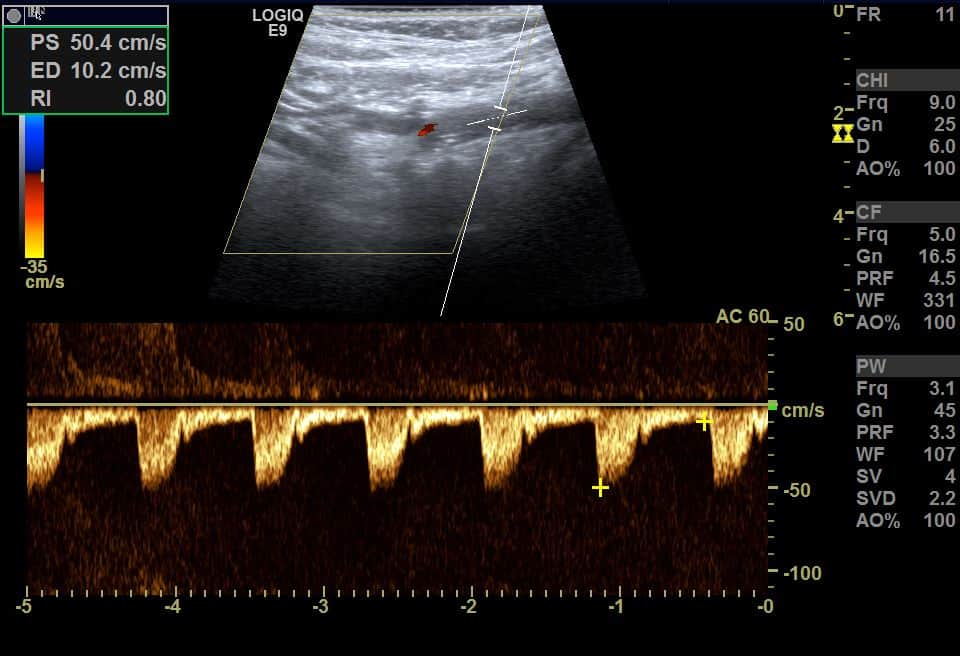
Doppler examination
- assess flow in the CCA, ECA, and ICA
- assess the V0-3 segments of the VA and subclavian artery (SA)
- triphasic high-resistance flow is typical for the subclavian artery
- origin of the VA can verified by tapping the artery behind the mastoid process (mastoid tap test), which provokes typical undulations in the Doppler waveform in the proximal segments
- flow in the thyrocervical trunk is high-resistant, unresponsive to mastoid tap test
- in the case of the SA stenosis, it is advisable to include an examination of the brachial artery
- set the correct Doppler angle
- angle between the direction of blood flow in the artery and the ultrasound beam
- correct angle is crucial for precise Doppler velocity quantification; the ideal Doppler angle for most vascular studies is 45-60 degrees
- an angle of 90 degrees yields no Doppler shift, and an angle close to 0 degrees may overestimate velocities
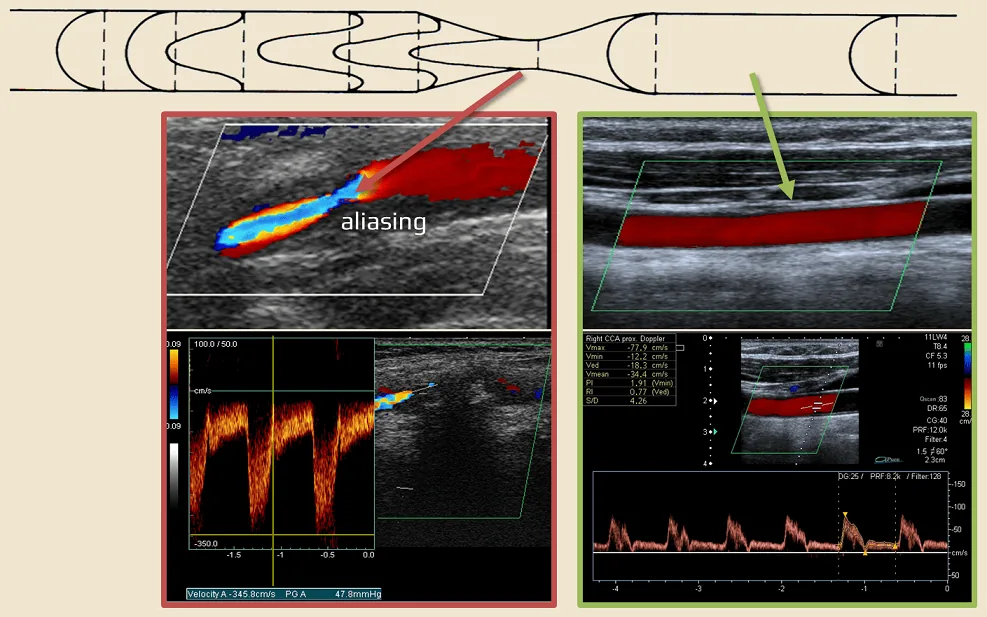
- assess the flow pattern (laminar x turbulent)
- turbulent flow (typical for stenosis) is identified by the presence of spectral broadening and aliasing
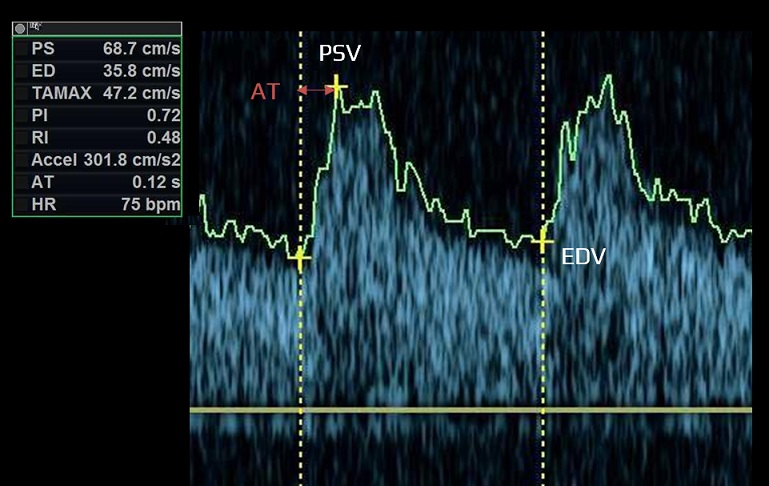
- determine PSV and EDV
- set the sample volume correctly
- identify the segment with the highest velocities (jet)
- determine the ICA/CCA index (using either PSV or EDV)
- assess systolic acceleration (acceleration time)
- slow acceleration may occur in stenosis of proximal arterial segments, due to aortic valve stenosis, or low ejection fraction (present in all arteries)
- measure the pulsatility index (RI) and resistance index (PI)
- most machines provide automatic measurement
- if necessary, dynamic tests can be performed to detect AV flow during maximal head rotation or head tilt to detect transient AV compression (→ Bow-Hunter syndrome)
- if a dural fistula fed from ECA is suspected (flow acceleration with low pulsatility), include an examination of the occipital artery
- note any arrhythmias and other Doppler waveform abnormalities
Doppler waveform characteristics
- several factors influence the character of the flow:
- heart ejection fraction (EF)
- flow volume and pressure
- resistance and geometry of the vascular system
- vessel wall elasticity
- blood viscosity
- the Doppler waveform refers to the morphology of pulsatile blood flow on spectral Doppler ultrasound
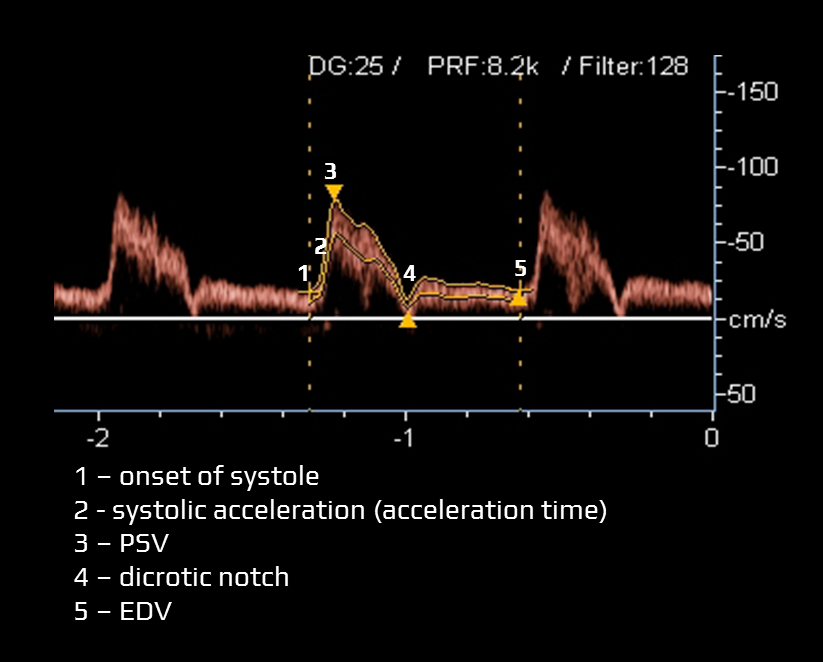
- typical items assessed within the Doppler waveform:
- acceleration time (systolic acceleration)
- time required for blood flow to reach peak velocity from the onset of systole (measured in milliseconds)
- a prolonged acceleration time may indicate proximal arterial stenosis/occlusion, stenosis of the aortic valve, or impaired cardiac contractile force
- peak systolic velocity (PSV) – the highest flow velocity during systole
- dicrotic notch
- a slight, downward deflection observed after the peak systolic velocity. This notch corresponds to aortic valve closure and the beginning of diastole in the cardiac cycle
- a prominent dicrotic notch may be indicative of increased peripheral resistance, commonly observed in conditions such as hypertension
- conversely, a blunted or absent dicrotic notch may indicate low systemic vascular resistance and may be seen in conditions like sepsis
- end-diastolic velocity (EDV)
- EDV is the velocity at the end of diastole; it is influenced by peripheral resistance (including distal stenosis)
- mean velocity (Vmean) is calculated
- resistance index and pulsatility index can be calculated from the above-stated values
- acceleration time (systolic acceleration)
- vessels are classified according to the peripheral resistance
- high-resistance limb type (typically the ECA)
- low-resistance parenchymal type (typically the ICA, VA)
- the CCA waveform has an intermediate profile under physiological conditions because it depends on peripheral resistance in both intracranial (brain) and extracranial regions (skin, muscles)
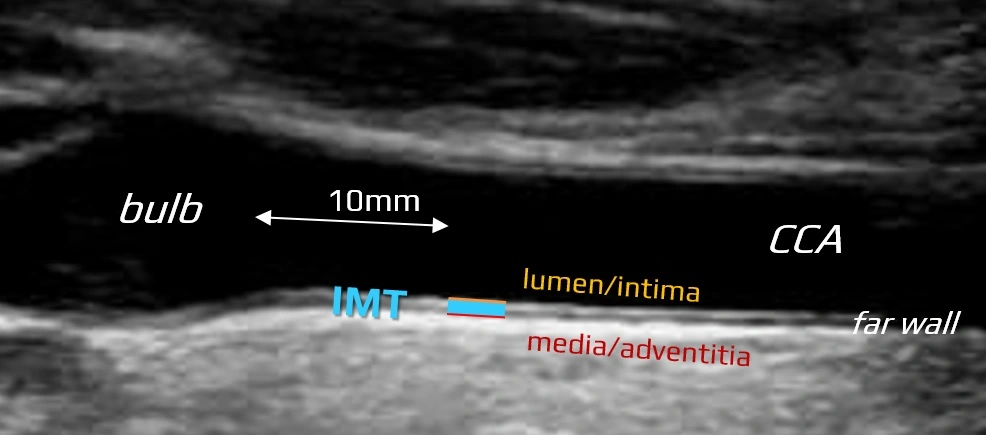
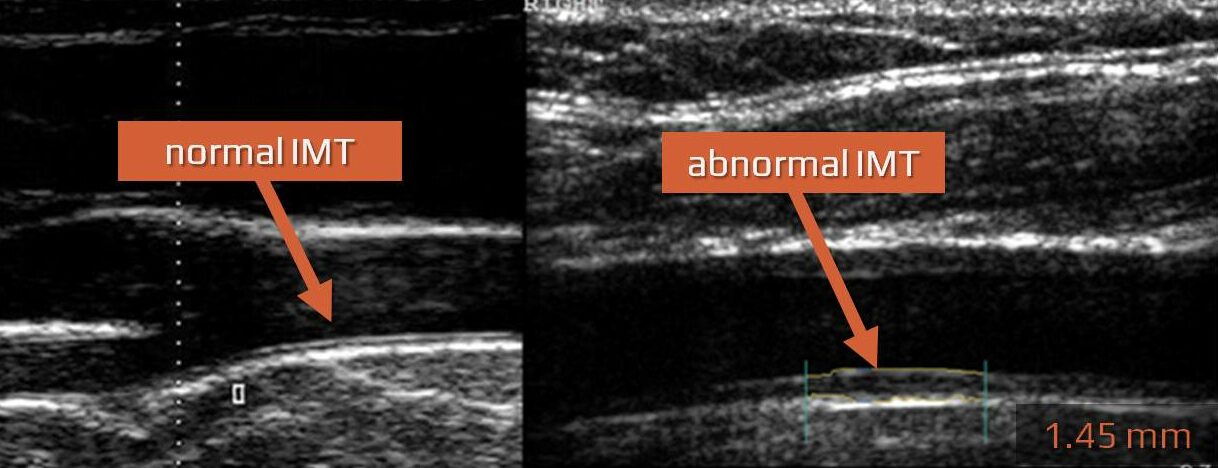
Intima-media thickness
- decades of silent arterial wall alterations precede atherosclerotic disease with clinically evident cardiovascular events
- the first detectable morphological abnormalities (enlargement of intima-media) can be visualized using B-mode imaging
- the intima-media extends from the luminal edge of the artery to the boundary between the media and the adventitia
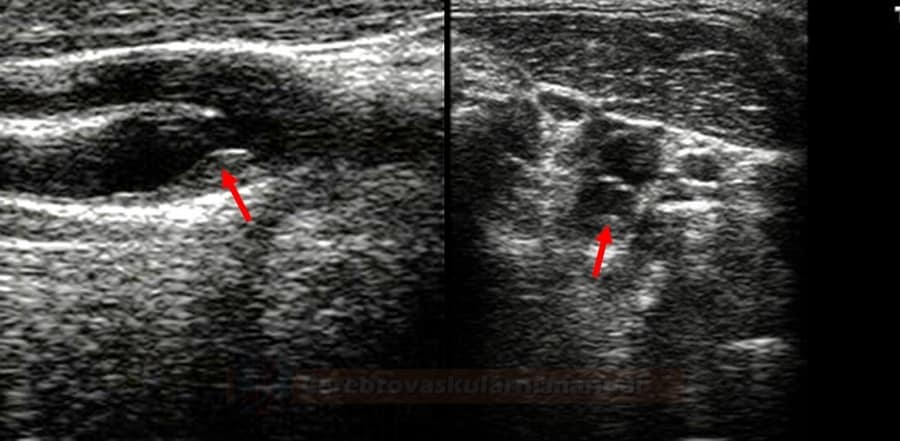
How to measure IMT?
- the standard measurement is performed in B-mode on the far wall of the common carotid artery (CCA), 10 mm proximal to the bifurcation
- use high-resolution images and adjust depth of focus and gain settings to obtain optimal image quality
- employ linear ultrasound transducers at frequencies above 7 MHz
- optimize the insonation angle (90° to the vessel wall)
- values obtained from different sites (such as distal ICA, bulb) should be documented separately
- values from the near wall are dependent on gain settings and are thus less reliable
- measure the distance between the 2 parallel echogenic lines
- the first line represents the lumen-intima interface
- the seond line represents the media-adventitia interface
- obtain at least five measurements on each side and calculate the average value (“average IMT”); specialized software may be helpful
 [Baldassare, 2000]
[Baldassare, 2000]
- automated systems can rapidly provide the mean maximal value of 150 measurements performed over a 10 mm segment of the CCA
- perform IMT measurements in a region free of atherosclerotic plaque, which is defined as:
- lesion ≥1.5 mm
- structure encroaching into the arterial lumen by at least 0.5 mm or 50% of the surrounding IMT value
- lesion ≥1.5 mm
- interadventitial and lumen diameter must also be obtained, as IMT correlates with arterial diameter
- echogenicity, especially of the media, may be increased in the presence of fatty infiltration and thickening
What is normal IMT?
- IMT > 75-95th percentile for age and sex is considered abnormal
- some authors suggest simple cut-off values:
- IMT < 0.8 mm – value associated with normal healthy individuals
- IMT ≥ 1 mm – value associated with atherosclerosis and a significantly increased risk of cardiovascular disease (CVD) in any age group
| Women (95. percentile) |
Men (95. percentile) |
||||
|
45 y
|
55 y |
65 y |
45 y | 55 y |
65 y |
|
0.73
|
0.91 | 1.04 |
0.89
|
1 | 1.3 |
95.th percentile [Howard, 1993]
| Age |
P25 | P50 |
P75 |
| men <30 | 0.39 | 0.43 | 0.48 |
| men 31-40 | 0.42 | 0.46 | 0.50 |
| men 41-50 | 0.46 | 0.50 | 0.57 |
| men >50 | 0.46 | 0.52 | 0.62 |
| women <30 | 0.39 | 0.40 | 0.43 |
| women 31-40 | 0.42 | 0.45 | 0.49 |
| women 41-50 | 0.44 | 0.48 | 0.53 |
| women >50 | 0.50 | 0.54 | 0.59 |
Prognostic value of IMT measurement
- not only atherosclerotic plaques but also IMT can quantify atherosclerosis burden in asymptomatic patients
- IMT should be assessed in each extracranial ultrasound examination
- increased IMT represents the first stage of atherosclerosis and, if left untreated, is followed by plaque formation
- clinical and epidemiological studies have shown an association between IMT and coronary artery disease (CAD), stroke, and peripheral vascular disease (PAD) (ROTTERDAM, ACAPS trials ) [Lorenz, 2007]
- thickening of IMT correlates with the presence of traditional vascular risk factors (high BMI, hypertension, hypercholesterolemia, diabetes, smoking)
- some authors recommend including both IMT and the presence of atherosclerotic plaquess among the classic vascular risk factors [Chambless, 2010]
- some publications question significance of IMT in predicting cardiovascular events [Costanzo, 2010] [Ruijter, 2012]
- detection of subclinical atherosclerosis is important in patients with borderline risk and multiple risk factors, as it shifts the patient into the high-risk category (SCORE ≥ 5%) with all therapeutic consequences
- pharmacological studies have shown a reduction in the rate of progression of IMT with hypolipidemic therapy and antihypertensive drugs (ACAPS, METEOR)
- on the other hand, a meta-analysis of 41 randomized trials showed regression of cardiovascular events with hypolipidemic drugs but did not show a relationship between a decrease in CV events and a regression of IMT [Costanzo, 2010]
- an enlarged arterial wall can also be found in non-atherosclerotic diseases (e.g., Takayasu arteritis)
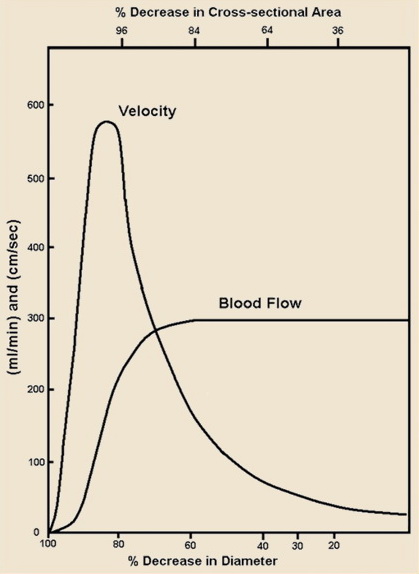
Assessment of arterial stenosis
The stenosis grade can be determined by measuring:
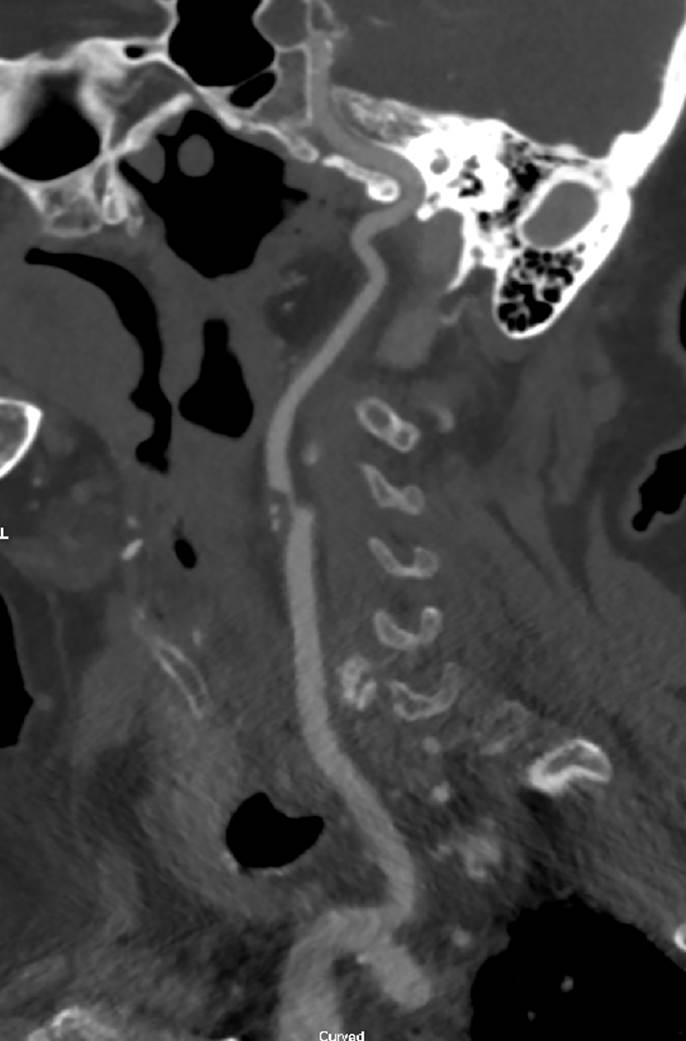
- diameter – calculation is performed according to the NASCET or ECST (DSA, CTA) → evaluation of carotid stenosis on CTA
- for smaller stenoses in the carotid bulb, the stenosis may reach negative values when assessed using the NASCET criteria
- for smaller stenoses in the carotid bulb, the stenosis may reach negative values when assessed using the NASCET criteria
- cross-sectional area (CTA)
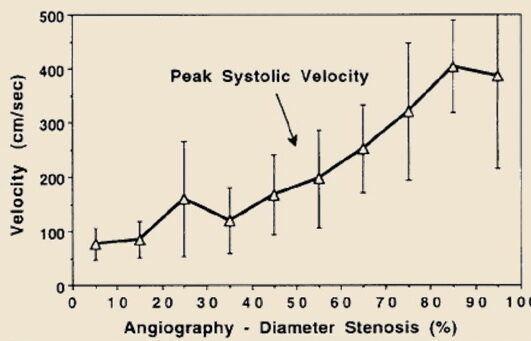
- peak systolic velocities and calculating velocity indices (ultrasound)
When evaluating stenoses on CTA, MRA, or DSA, the NASCET method is commonly used. Ultrasound findings correlate well with this measurement technique.
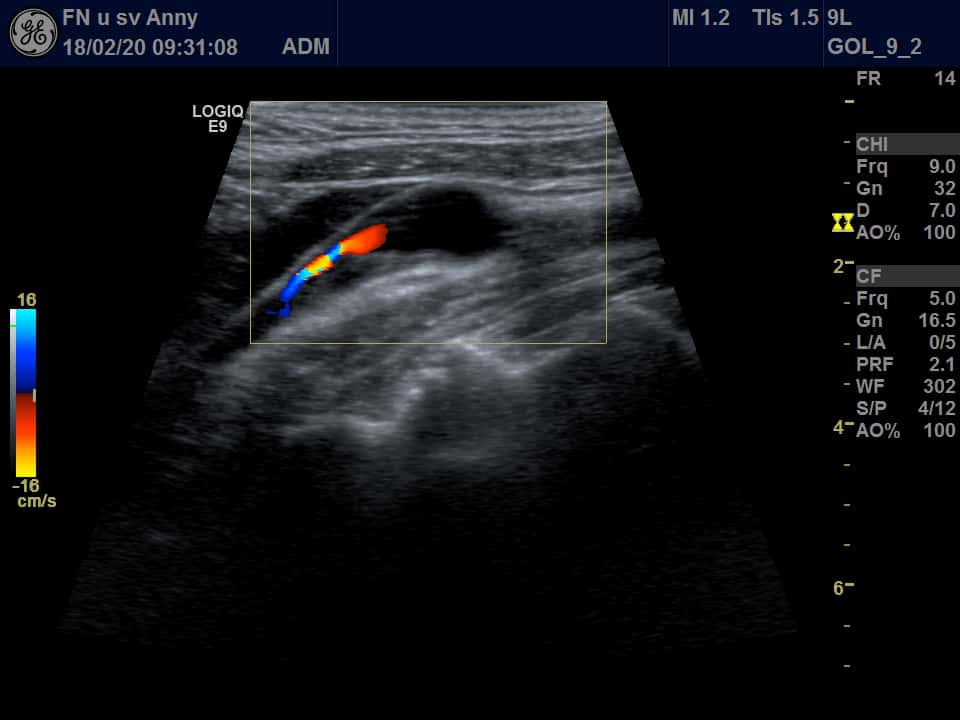
Direct signs of stenosis
- measure the width of atherosclerotic plaque and the residual lumen using B-mode
- often not possible in distal VA stenoses, distal segments of the ICA, or in the presence of acoustic shadow
- visualize stenosis using color mode or power mode (lumen reduction + aliasing)
- detect increased, turbulent flow within the stenosis (correlates well with DSA and surgical findings) [Alexandrov, 1993] [Alexandrov, 1997]
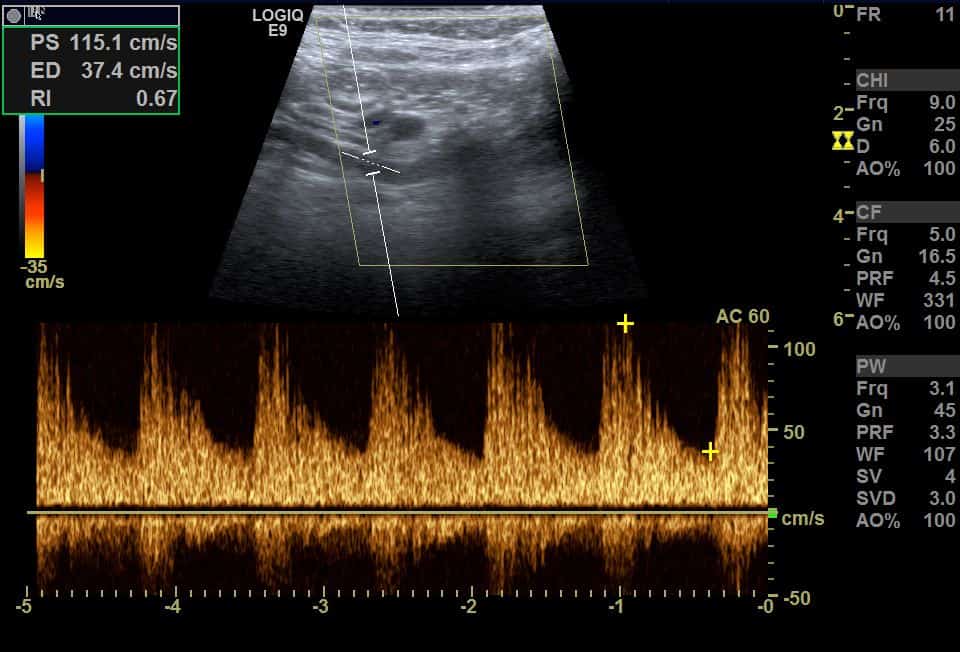
Indirect signs of stenosis
- resistant flow in proximal segments (with ↑ PI, RI)
- detection of developed collateral circulation
- “internalization” of flows in the external carotid artery (ECA), characterized by decreased resistance
- retrograde flow in the ophthalmic artery (OA)
- increased flow in the anterior communicating artery (AComA), along with retrograde flow in the anterior cerebral artery (ACA
- increased flow in the ipsilateral posterior cerebral artery (PCA) and posterior communicating artery (PComA)
- dampened flow in the distal segment (including intracranial arteries)
- ↓ PSV
- ↓PI and RI (due to compensatory vasodilation)
- prolonged systolic acceleration
- impaired vasomotor reactivity (VMR)
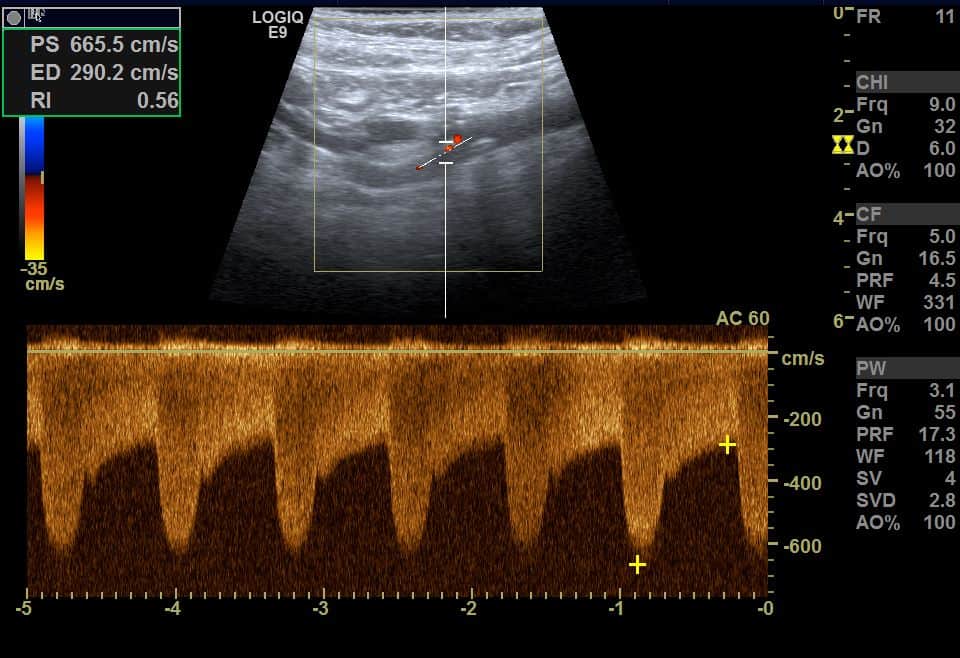
- mean velocity correlates positively with the degree of stenosis; however, a wide range of PSV values exists for each degree of stenosis
- therefore, it is advised to stratify stenosis (see table) rather than providing a single value
- refinement can be achieved through multiparametric evaluation
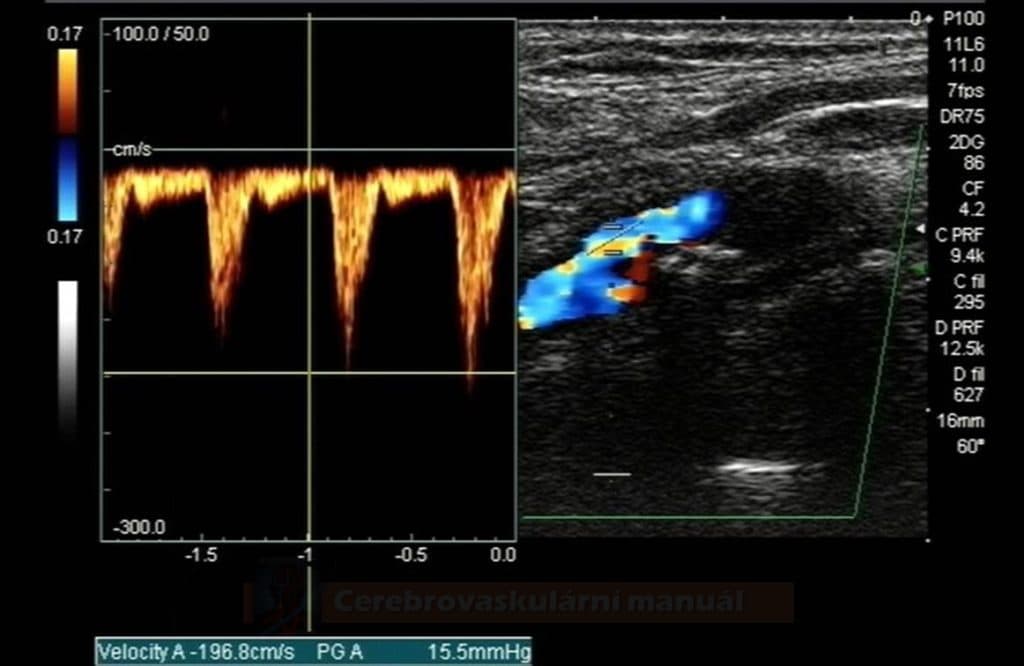
| Stenosis grade |
PSV (cm/s) |
EDV (cm/s) |
Flow pattern |
B-mode (plaque %) |
PSV ACI/ACC index |
| normal finding |
≤ 125 | < 40 | laminar | absent | < 2 |
| < 50% | < 125 | ≤ 40 | laminar | < 50% | ≤ 2 |
| 50-69% | 125-230 | 40-100 | mildly turbulent | > 50% | 2-4 |
| 70-95% | > 230 | > 100 | turbulent | > 50% | > 4 |
| subtotal stenosis (near occlusion) |
variable | variable | highly turbulent | filiform stenosis | variable |
| occlusion | – | – | – | occlusion (acute x chronic) |
– |
| [Radiology, 2003] | |||||
Assessment of arterial occlusion
- ultrasound is reliable for diagnosing acute ICA occlusion [Herzig, 2011]
- B mode:
- chronic occlusion – the lumen is filled with heterogeneous atherosclerotic masses and is retracted and poorly visualized in distal segments
- acute occlusion – lumen is hypoechoic (fresh thrombus)
- difficulties arise in patients with preexisting severe stenosis when a fresh thrombus occludes the remaining free lumen
- similar Doppler finding can be seen with terminal ICA occlusion, where stagnant blood fills the proximal ICA, mimicking occlusion at the vessel’s origin
- color mode: no color is visible in the arterial lumen
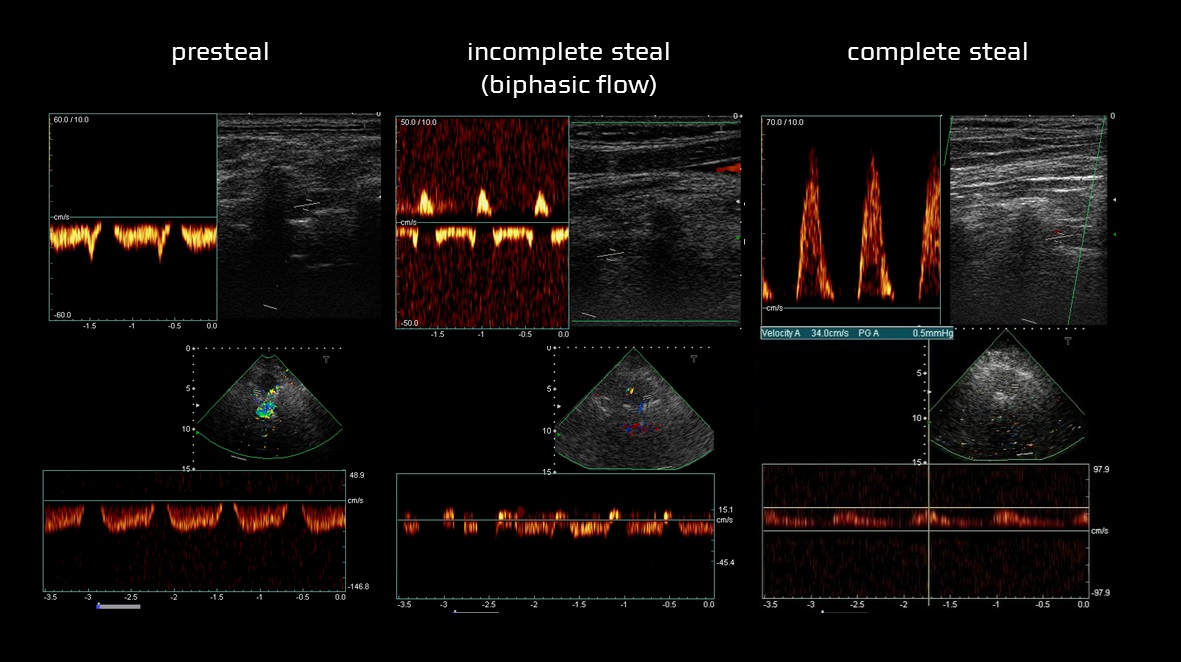
- Doppler:
- complete absence of flow, systolic peaks may be detected in the proximal segment
- resistant flow in the proximal segments (e.g., in the CCA in cases of ICA occlusion)
- in distal VA occlusions, either peaks or low, resistant flow with zero diastole are observed in the V2 segment
- in hypoplasia, the diastole is always non-zero
- complete absence of flow, systolic peaks may be detected in the proximal segment
| Acute occlusion | Chronic occlusion |
| anechoic lumen | heterogeneous AS masses |
| symmetric ICA lumen width | ICA lumen is retracted, gradually disappearing distally |
| lack of collaterals | fully developed collateral circulation |
| markedly reduced flow in the ipsilateral MCA | typically only mildly reduced flow in the MCA with slowed systolic acceleration (depending on the quality of the collateral circulation) |
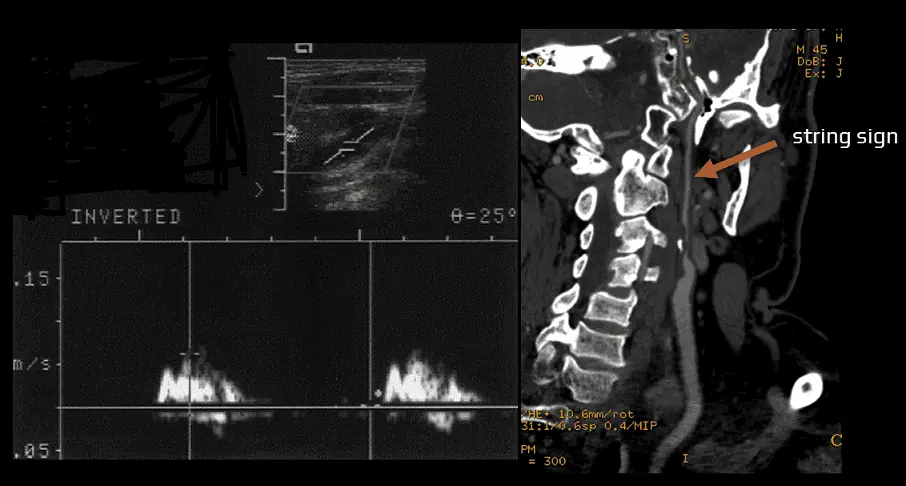
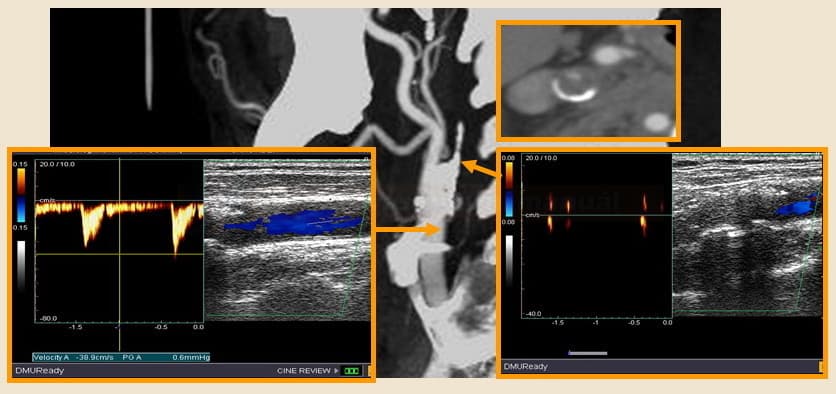
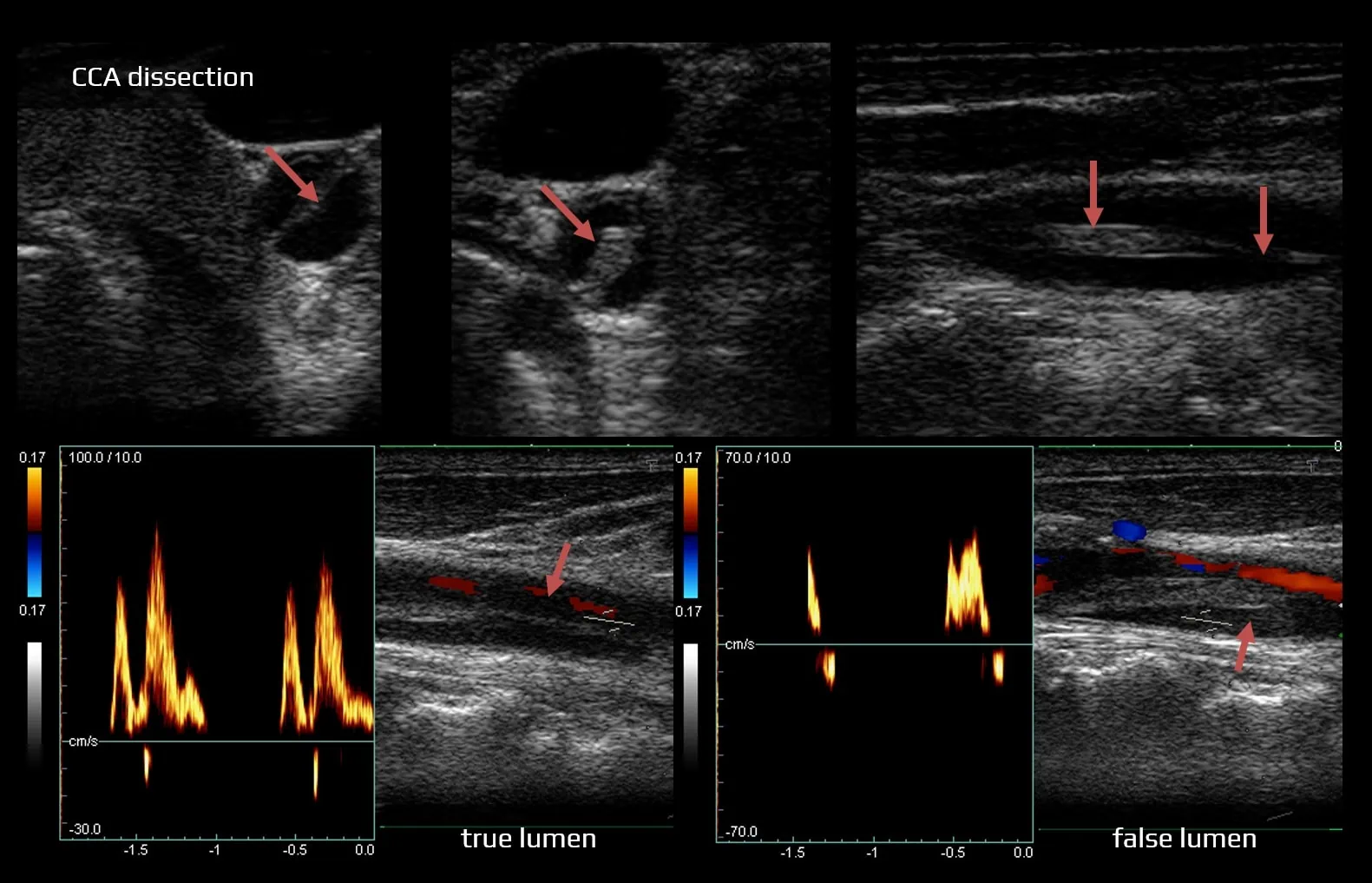
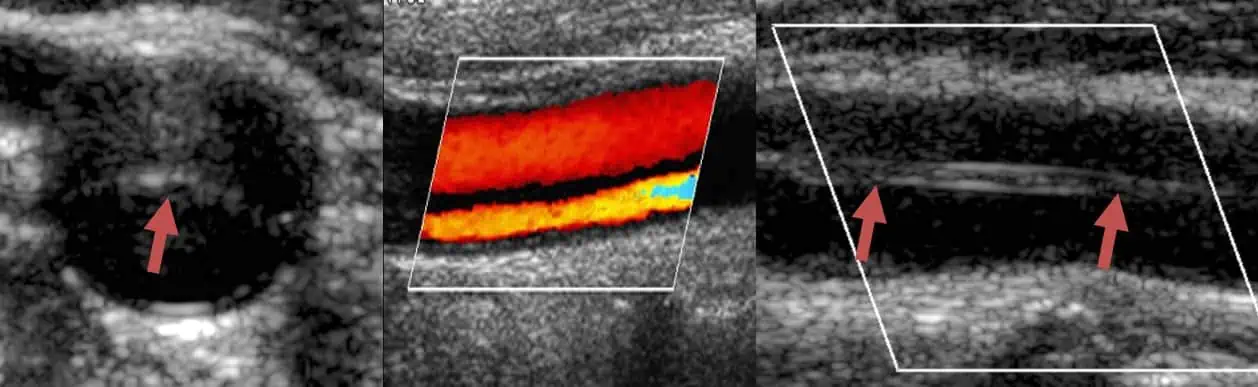
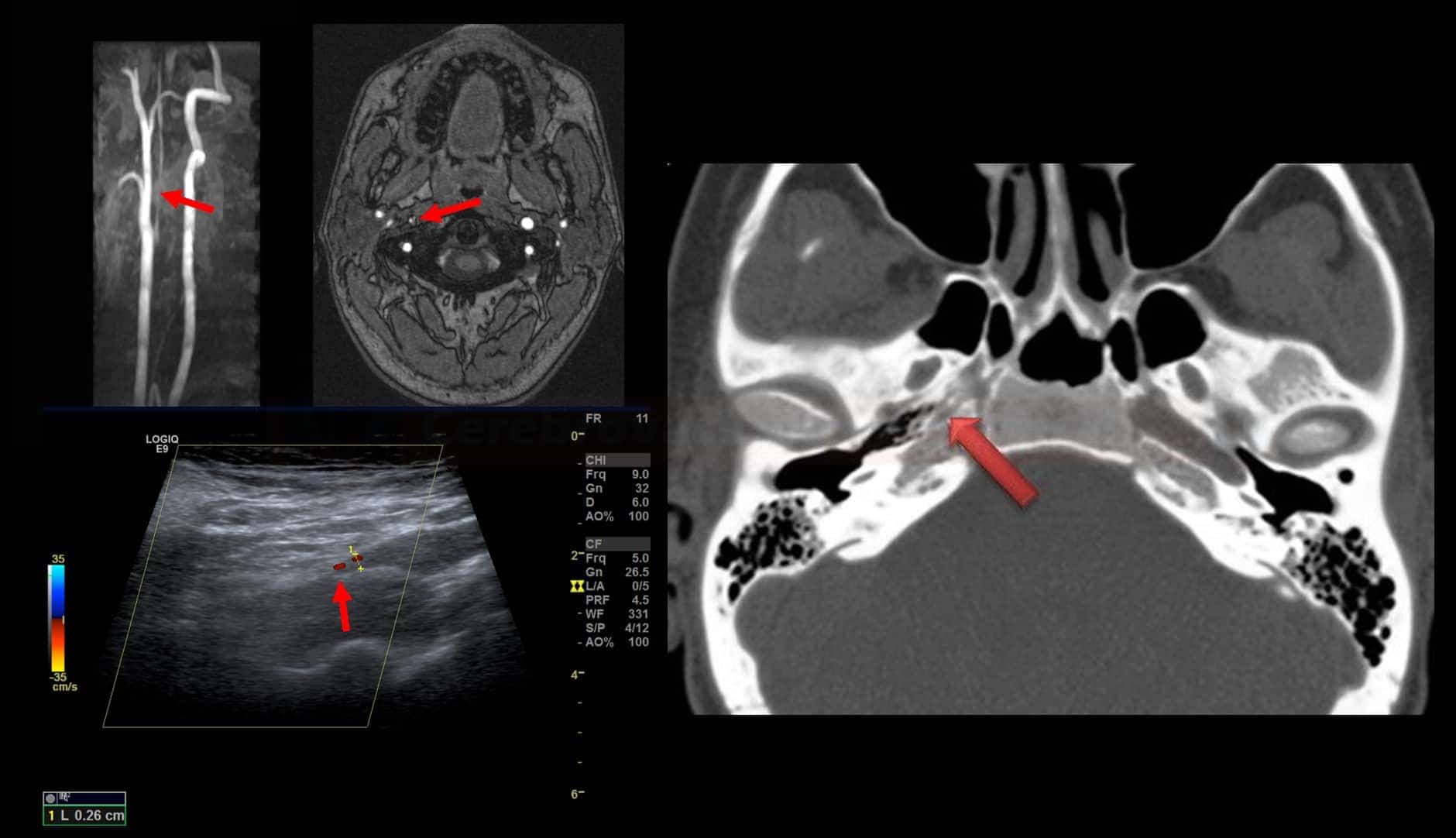
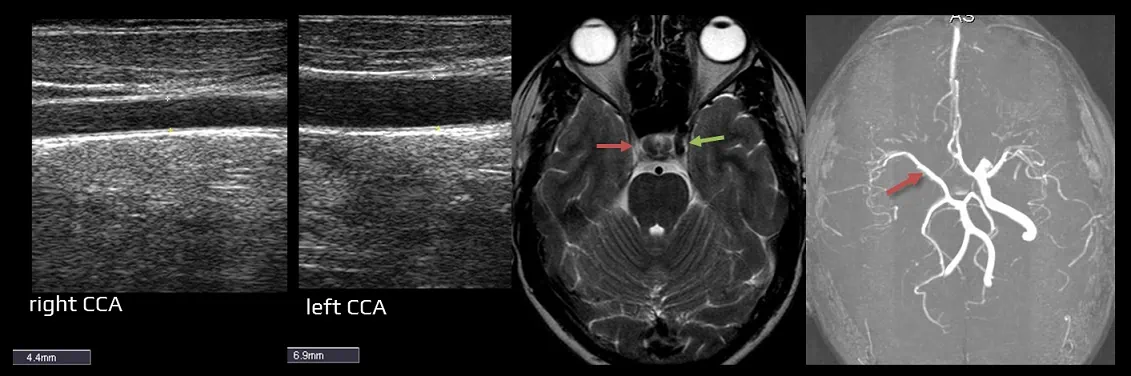
Dissection
Carotid artery
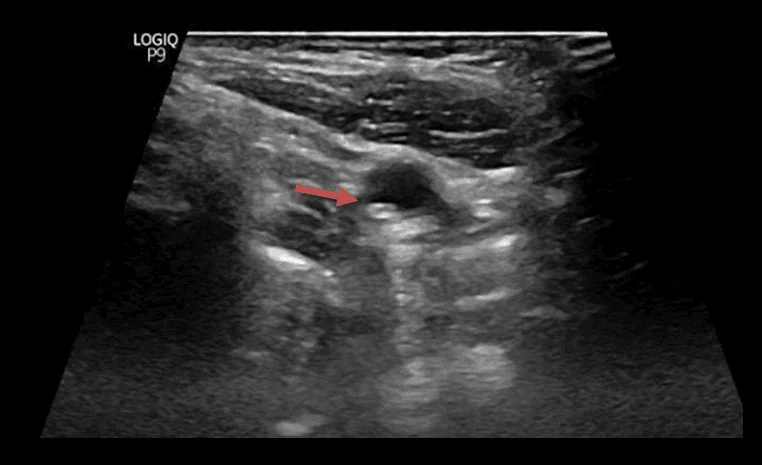
- B mode – during the acute and subacute stages, the most common finding is a homogeneous, predominantly hypoechoic hematoma causing stenosis (forming tapered lumen) or double lumen with an intimal flap
- Color Doppler Flow (CDF) mode – may identify flow in the false and true arterial lumens
- Doppler:
- true lumen – may show stenotic (↑PSV, turbulence) or preocclusive flow (high-resistance flow or systolic peaks)
- false lumen – low, highly resistant flow; occasionally systolic peaks, reversed or bidirectional flow are present (depending on thrombus presence, entry and exit flaps, flap wall motion, and dissection extent)
- in the chronic stage, after the resorption of the hematoma, the ultrasound image becomes nonspecific (residual stenosis, occlusion, or even a normal finding)
Vertebral artery
- typically involves segments V3/4 (check atlas loop) or V1/2 (at the level of C6)
- B-mode – irregular, often multisegmental stenosis or occlusion without obvious atherosclerotic changes, rarely double lumen, intimal flap, pseudoaneurysm, and hypoechoic hematoma in the vessel wall are visualized
- Doppler
- highly resistant, biphasic flow, or absent flow
- low post-stenotic blood flow in distal segments
- ultrasound is useful for follow-up of vertebral artery dissection in patients with stenosis or occlusion, but pseudoaneurysm formation may not be detected
- if dissection is clinically suspected, further imaging should be performed even if ultrasound results are negative
Other pathological findings and anatomical variants
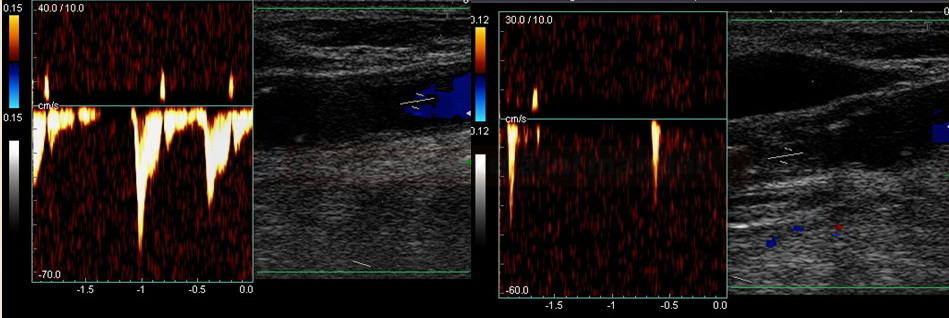
Kinking and coiling
- both conditions (congenital or acquired) may occasionally result in altered hemodynamics
- arterial kinking
- arterial coiling
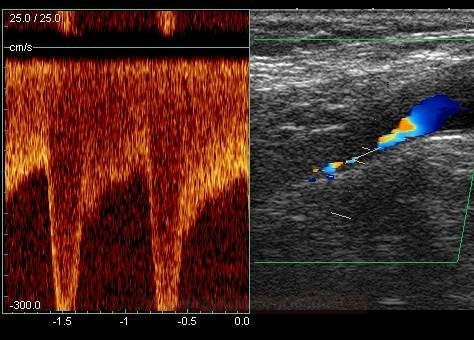
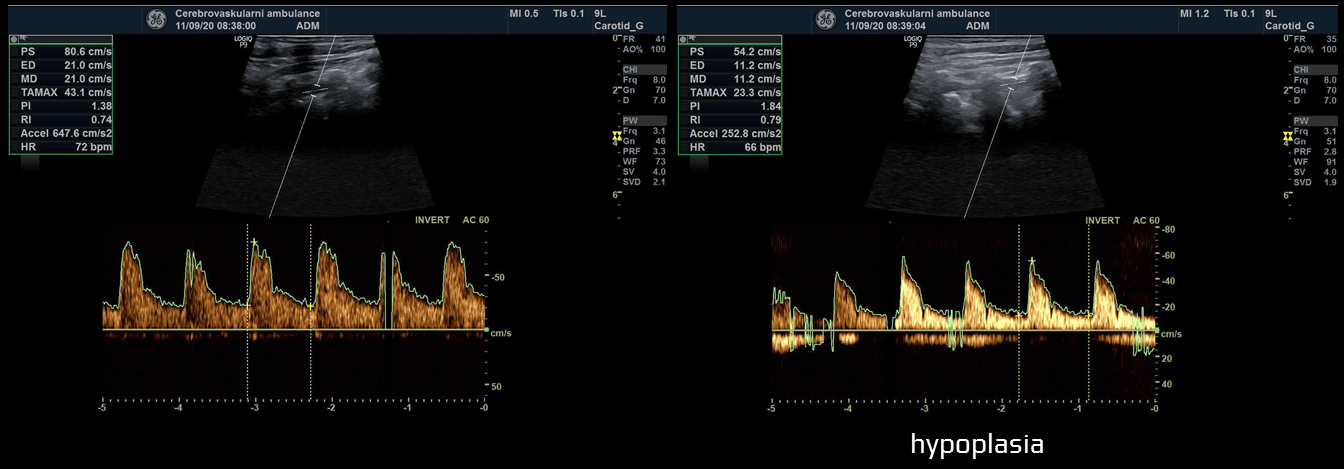
Hypoplasia/aplasia of the vertebral artery
- hypoplasia
- relatively common anatomical variant (~1-6%, more often on the right side)
- lumen < 2-3 mm (limits reported variously), definitely < 2 mm
- PSV is usually < 40 cm/s, with increased peripheral resistance (↑ PI, RI) but non-zero diastolic flow (adjust scale or PRF properly)
- an indirect criterion for hypoplasia is a compensatorily wider contralateral VA
- the hypoplastic vessel may terminate distally as the PICA
- aplasia
- rare (~1%)
- compensatorily larger contralateral VA (> 4mm)
- only the vertebral vein is detectable