ADD-ONS / MEDICATION
Perioperative and Periprocedural Management of the Anticoagulant Therapy
Updated on 21/12/2023, published on 09/02/2022
- long-term anticoagulation therapy often needs to be interrupted for various reasons (most commonly due to planned diagnostic or surgical procedures); interruption in emergencies is discussed elsewhere (→ Neutralizing the anticoagulant effect)
- the decision to discontinue anticoagulation periprocedurally represents a complex balancing act between the estimated risk of thromboembolism and bleeding
- these questions need to be addressed:
- is it necessary to discontinue anticoagulation?
- if so, how long before the procedure should it be discontinued?
- is bridging therapy necessary? at what dose?
- when should anticoagulant therapy be restarted after the procedure?
- to answer these questions, the following factors must be evaluated:
- individual risk of thromboembolism
- risk of bleeding (considering the characteristics of the patient and the planned procedure)
- type of procedure and its risk of bleeding
- features of the prescribed anticoagulant agent (warfarin x DOAC)
- renal functions
- type of procedure and its risk of bleeding
- warfarin requires a rather complex procedure – timely discontinuation (at least 3-5 days before the procedure), followed by monitoring of INR decline and starting LMWH once INR gets below 2 (if bridging is indicated)
- DOACs simplify the situation because of their rapid onset of action and predictable, relatively short-lasting normalization of coagulation parameters (thus, LMWH bridging is not necessary in most cases)
Is it really necessary to stop anticoagulant therapy?
- it is always a matter of better or worse estimation because the balance between the risk of thromboembolism when anticoagulation is withdrawn, and the risk of bleeding when it is continued is often unclear
- TE is relatively rare but can be fatal
- bleeding with continued anticoagulation is more common but typically less clinically relevant, usually without permanent sequelae
Thromboembolism risk assessment
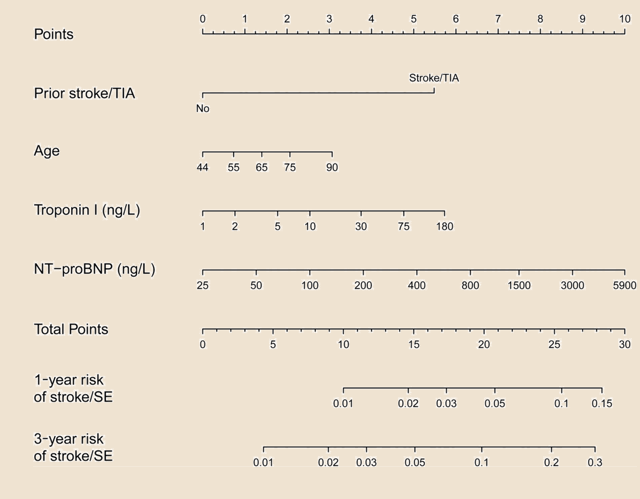
- use the CHA2DS2-VASc score in patients with Afib
- in patients with venous thrombosis (VTE), consider the time elapsed since the VTE diagnosis and the presence/absence of thrombophilia (a prothrombotic state)
- in patients with a mechanical valve, the risk depends on the type and location of the valve and the presence of contributing risk factors (AFib, heart failure, hypertension, diabetes, age >75 years, previous stroke)
| Clinical Indication for Anticoagulant Therapy | |||
| Thromboembolic Risk Category | Atrial Fibrillation | Mechanical Heart Valve | VTE |
| High risk (annual risk >10%) |
|
|
|
| Moderate risk (annual risk 5% to 10%) |
CHADS2 score 3-4 | bileaflet aortic valve prosthesis with ≥1 risk factor |
|
| Low risk (annual risk <5%) | CHADS2 score 0–2 (no prior stroke or TIA) | bileaflet aortic valve prosthesis without any risk factors | VTE >12 months ago |
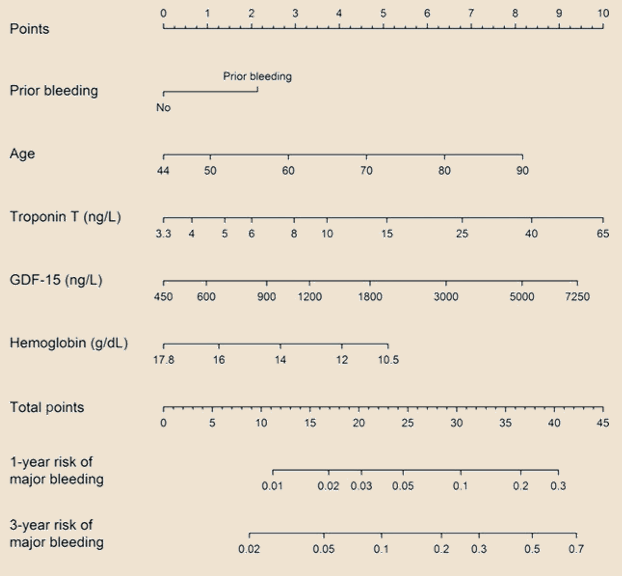
Bleeding risk assessment
- consider a combination of individual patient´s risks and the risk associated with the procedure itself
- take into account the location and invasiveness of the procedure
- many procedures can be safely performed without interrupting anticoagulation (either warfarin or DOACs), such as dermatological, ophthalmological, and dental procedures
| The risk of bleeding is unlikely to be increased |
simple dental procedures
|
| The risk of bleeding is probably not increased |
cataract surgery
dermatological procedures TRUS (ultrasound-guided prostate biopsy) spinal and epidural punctures carpal tunnel surgery |
| The risk of bleeding is apparently not increased |
EMG
transbronchial biopsy
colonoscopic polypectomy endoscopic gastric biopsy ultrasound-guided biopsies sphincterotomy |
| The risk of bleeding is possibly increased | |
| The risk of bleeding is probably increased | total endoprosthesis (TEP) |
Timing of anticoagulant therapy discontinuation
Discontinuation of DOAC before neuraxial anesthesia
- a higher perioperative hemorrhagic risk is assumed; therefore, a longer interval is recommended
- dabigatran: discontinue 4-5 days before surgery
- Xa inhibitors: discontinue 3-5 days before surgery
- restart DOAC ≥ 24 hours after the procedure
- consider LMWH bridging in high-risk patients
- separate guidelines for spinal and analgesic procedures are here and here
Is bridging required?
| Content available only for logged-in subscribers (registration will be available soon) |
Restart of the anticoagulant therapy
- the timing of anticoagulation restart is sometimes a neglected issue, although it is a crucial factor influencing the outcome
- generally, it is not necessary to start full anticoagulation (heparin, LMWH, DOAC) within 6-12 hours after the procedure
- according to the BRIDGE trial, initiating full anticoagulant therapy within 24-72 hours after the procedure is not recommended
- in patients at high risk of bleeding, wait for 72 h (especially for DOACs or LMWH, where the onset of anticoagulant effect is rapid)
- warfarin may be given earlier due to its delayed onset of full action