ADD-ONS / GENERAL NEUROLOGY
Relative afferent pupillary defect (RAPD)
Updated on 20/01/2024, published on 01/05/2022
Definition
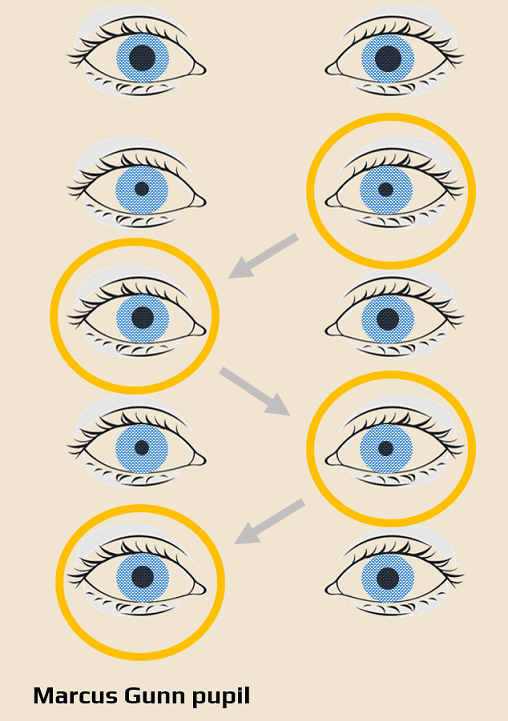
- relative afferent pupillary defect (RAPD), also known as Marcus-Gunn pupil, is the term referring to a specific abnormal response of the pupils to light stimuli
- RAPD is characterized by bilateral dilation of the pupils, instead of constriction, during the swinging flashlight test
- RAPD serves as the hallmark of a unilateral or bilateral asymmetric afferent sensory lesion
- many factors may influence the identification and accurate quantification of RAPD; subtle abnormalities are difficult to detect
Examination
- initially, assess the size, equality, and regularity of the pupils during a standard eye examination
- test response to a standard light stimulus
- under normal conditions, both pupils constrict equally and briskly
- a single light stimulus of the Marcus-Gunn pupil (with an aberrant afferent part of the visual pathway) results in weak bilateral pupil constriction
- alternating light stimulus to both eyes (“swinging flashlight test“)
- shine a penlight into one eye, then swing it to the other
- alternate quickly and observe the response of the patient’s pupils
- both pupils should constrict quickly and equally during intermittent exposure to direct light
- after swinging the light stimulus from the healthy eye to the Marcus Gunn eye (swinging test), bilateral pupil dilation occurs
- the swinging flashlight test, showing RAPD, is most valuable in the detection of optic nerve lesions, as retinal lesions usually present with pathologic fundoscopic findings
- the only challenge arises with the bilateral symmetric afferent optic pathway defects anterior to the chiasm, which do not lead to the detection of a relative afferent defect
- however, RAPD may be present in bilateral asymmetric prechiasmatic, chiasmatic, and optic tract lesions (contralateral to the lesion, as crossing fibers outnumber noncrossing fibers)
- lesions affecting the final neuron of the optic pathway (tractus geniculocalcarinus) do not lead to abnormalities in the pupillary reflex
Conditions associated with RAPD
- optic neuritis (multiple sclerosis, neuromyelitis optica spectrum disorder, anti-MOG, etc.)
- even mild optic neuritis with minimal vision loss or normal vision can lead to RAPD
- ischemic optic neuropathies (arteritic and nonarteritic causes)
- glaucoma (if one optic nerve is particularly severely damaged, RAPD may be observed)
- other optic nerve autoimmune disorders (sarcoidosis, systemic lupus erythematosus, Sjögren’s syndrome)
- optic nerve infections (cat scratch disease, syphilis, Lyme disease, toxoplasmosis, cytomegalovirus, cryptococcus, and tuberculosis, etc.)
- hereditary optic neuropathies, such as Leber’s optic neuropathy (usually bilateral) and other inherited optic neuropathies
- optic nerve tumor (glioma, meningioma of the optic nerve, or tumors compressing the optic nerve)
- compressive optic neuropathy, with or without the orbital disease (thyroid-related orbitopathy, orbital tumors, or vascular malformations)
- traumatic optic neuropathy
- radiation-induced optic neuropathy
- optic atrophy (e.g., due to papilledema)
- postsurgical optic nerve damage
- idiopathic optic neuropathy
- the symmetrical bilateral retinal disease does not show RAPD
- ischemic retinal disease
- central retinal vein occlusion (CRVO)
- central retinal artery occlusion (CRAO)
- severe ischemic branch retinal artery occlusion (BRAO)
- severe ischemic diabetic or sickle-cell retinopathy)
- Ischemic ocular disease (Ocular ischemic syndrome due to ophthalmic or carotid artery stenosis/occlusion)
- retinal detachment
- severe macular degeneration (if unilateral and severe)
- intraocular tumor (retinal and choroidal tumors including melanoma, retinoblastoma, and metastatic lesions)
- retinal infection (cytomegalovirus, herpes simplex, and other causes of retinitis)
- amblyopia (RAPD can be present in severe amblyopia; the visual acuity would usually be worse than 20/400
- cerebral vascular disease


