ISCHEMIC STROKE / CLASSIFICATION AND ETIOPATHOGENESIS / NONINFLAMMATORY VASCULOPATHIES
Fibromuscular dysplasia (FMD)
Updated on 26/01/2024, published on 14/03/2022
- mostly sporadic, rarely hereditary, noninflammatory disease of unknown etiology affecting medium-sized arteries
- localization (usually sparing the origin of the vessel):
- an extracranial portion of the ICA/vertebral arteries
- renal arteries (most common)
- splanchnic arteries (rare)
- subclavian, axillary, and iliac arteries (rare)
- usually occurs in young to middle-aged women
- F: M ratio of 3:1
- onset typically between 30 and 50 years of age
- involved arteries show segmental stenoses and enlargements, with approximately one-third of patients having multiple lesions
- FMD can lead to serious complications (TIA/stroke, spontaneous dissection, aneurysm formation, myocardial infarction)
Pathology
- unknown etiology
- identification of YY1AP1 mutations (typical for Grange syndrome) as a cause of FMD indicates that this condition may result from various genetic disorders (Guo, 2017)
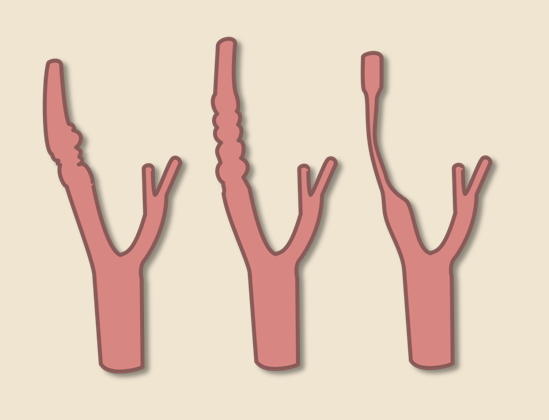
- fibrous or fibromuscular thickening of the arterial wall (intima, media, and adventitia) leading to segmental stenoses and microaneurysms
- intima is involved in < 5% of cases (⇒ intimal fibroplasia, also called carotid web)
- media involvement is predominant (90-95% of cases)
- adventitia (rare, less than 1% of cases)
- histology
- accumulations of dysplastic muscle cells + disruption of the internal elastic membrane
- no inflammatory cells are present
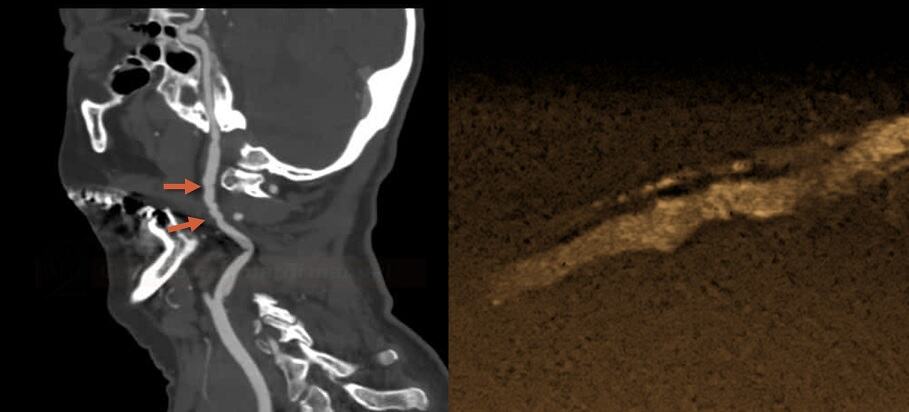
- carotid lesions are typically localized in the middle and distal segments of the extracranial internal carotid artery, often extending to the skull base
- FMD predisposes to the development of aneurysms (extra- and intracranial) and arterial dissections
- ⇒ it is advisable to examine the renal arteries in all patients presenting with arterial dissection
Clinical presentation and diagnostic evaluation
- carotid artery lesions are often asymptomatic but can cause TIA/stroke due to:
- distal thromboembolism (e.g., originating from the aneurysm)
- arterial dissection
- renal artery involvement leads to renovascular hypertension (by activating RAAS) or renal impairment
- coronary artery involvement can lead to angina pectoris, myocardial infarction, and cardiac death
- FMD is diagnosed by a typical appearance on vascular imaging (CTA, MRA, DSA, ultrasound)
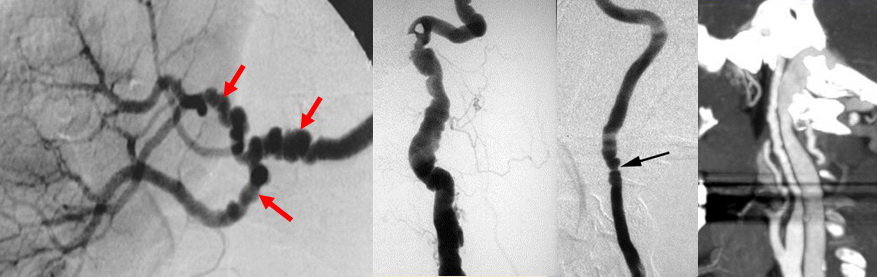
- affected arteries usually exhibit a rosary-like appearance caused by concentric luminal narrowing alternating with areas of mural dilatation (a string of beads/pearls appearance)


- this finding is present in up to 90% of patients with FMD
- less commonly, patients may present with concentric long-segment tubular stenosis
- affected arteries usually exhibit a rosary-like appearance caused by concentric luminal narrowing alternating with areas of mural dilatation (a string of beads/pearls appearance)
- FMD may manifest as carotid dissection (best seen on fat-saturated T1 imaging)

- less typical features include intracranial aneurysms that can lead to subarachnoid hemorrhage (SAH)
| Content available only for logged-in subscribers (registration will be available soon) |
Differential diagnosis
- atherosclerosis – usually present at the origin or proximal segment of the ICA
- vasculitis
- segmental arterial mediolysis (Chao, 2009)
- noninflammatory arteriopathy characterized by dissecting aneurysms resulting from lysis of the outer media of the arterial wall
- vasospasms
Management
Acute stroke therapy
- recanalization therapy for all eligible patients
- antithrombotic drugs for the rest
Stroke prevention
- asymptomatic carotid lesions – a conservative approach is preferred; antiplatelet therapy is not recommended
- stroke patients with FMD:
- the strict control of blood pressure and other vascular risk factors
- antiplatelet therapy (AHA/ASA 2021 I/C-LD)
- ASA is most commonly used (based on expert opinion, no trials available)
- statins are not routinely used unless there is another indication
- for stroke caused by carotid dissection without thrombosis, antiplatelet therapy is usually used (AHA/ASA 2021 2a/C-EO)
- if medical treatment fails or significant carotid artery stenosis develops, consider angioplasty (AHA/ASA 2021 2b/C-LD) (Tekieli, 2015)
- angioplasty for FMD has high long-term patency rates; stenting is not always required
- robust data on the clinical benefit of CAS over conservative therapy are lacking
Renovascular hypertension
- renal artery angioplasty with stenting is indicated in proven renovascular hypertension if significant stenosis of the renal artery affects blood flow to the kidney
- the RAA system provides adequate glomerular pressure by vasoconstriction; this compensatory mechanism can lead to hypertension
- ACE inhibitors, commonly used to manage hypertension, can cause renal hypoperfusion
- the RAA system provides adequate glomerular pressure by vasoconstriction; this compensatory mechanism can lead to hypertension
- the decision to perform renal angioplasty should be made based on the individual patient’s condition, the severity of renal artery stenosis, and other factors