ADD-ONS
Brain death diagnosis
Updated on 06/07/2024, published on 10/04/2023
Brain death definition
- brain death (BD)/death by neurologic criteria (DNC) is defined as the permanent (irreversible) loss of all functions of the entire brain (including the brainstem), regardless of the continued function of the cardiovascular system and other organs
- loss of all functions results in coma, brainstem areflexia, and apnea in the setting of an adequate stimulus
Etiology
- traumatic brain injury (TBI)
- cerebrovascular events (subarachnoid hemorrhage, intracerebral hemorrhage, ischemic stroke)
- global cerebral hypoxia/anoxia (post-CPR conditions)
- brain tumors
- intracranial infection (vasculitis, encephalitis, etc.)
- intoxication (methanol, opioids, carbon monoxide, etc.)
- metabolic disorders leading to malignant cerebral edema (hypoglycemia, Reye’s syndrome, etc.)
Diagnostic evaluation
Legal aspects of brain death diagnosis and organ donation vary from country to country (personnel specialization requirements, approved confirmatory methods, etc.). The protocol approved by the local authorities must be followed.
The diagnosis of brain death is generally based on the following:
- before performing the BD/DNC evaluation, patients must be observed for sufficient time to determine the severity and permanency of the brain injury and exclude confounders
- there is no standard observation period before the initiation of the evaluation for BD/DNC
- patients with any evidence of consciousness or preservation of any brainstem reflex or who display motor movements that are mediated by the brain or brainstem or are spontaneously breathing do not meet established criteria and must not undergo BD/DNC testing
- consent is not required to evaluate a patient for death. The decision to initiate an evaluation for BD/DNC after catastrophic, permanent brain injury is a clinical decision made by the attending clinician by the institution’s policy
- clinicians planning to evaluate a patient for BD/DNC should inform the patient’s family
Clinical signs of brain death
Deep non-reactive coma (GCS 3)
|
| Absent cortical functions |
|
| Absent brainstem functions |
|
The following items are usually part of the clinical brain death protocol and should ALL be negative:
- brainstem reflexes
- the oculocephalic reflexes (OCR – vertical/horizontal) can be harmful to a patient with cervical spine injury or absence of skull base integrity
- the OVR provides a stronger vestibular stimulus than the OCR and, therefore, may be a more sensitive test of the involved brainstem pathways
- motoric response to pain stimuli in the area innervated by the trigeminal nerve
- cough reflex (provoked by deep tracheobronchial suction)
- caloric oculo-vestibular reflex (OVR)
- oculocardiac reflex (trigeminovagal reflex)- tests the integrity of the caudal brainstem – the eyeball is compressed for 10-20 s; the test is positive if pulse drops by more than 20% (8-10)
- most commonly, the reflex induces bradycardia, though it may cause arrhythmias and, in extreme cases, cardiac arrest
- atropine test
- administration of atropine 1mg IV does not cause tachycardia in brain death
- atropine test is not a standard part of the protocol for diagnosing brain death
- children – 2 clinicians must each perform a separate and independent examination with a minimum interval of 12 hours (AAN guidelines, 2023)
- adults – a minimum of 1 examination for BD/DNC; a second clinician may perform a separate and independent examination for BD/DNC to decrease the risk of a false-positive determination due to diagnostic error
- the patient must not be pharmacologically depressed and relaxed to the extent that inhibits brainstem reflexes
- these activities may be preserved:
- vasomotor activity, which maintains blood pressure without vasopressor support (cervical sympathetic activity is probably sufficient to maintain it temporarily)
- osmoregulation (e.g., diabetes insipidus is not a prerequisite for brain death; it is absent in up to 20% of cases)
- repeated tests show the irreversibility of the clinical condition (interval > 4 hours)
- when the accurate evaluation of a component of the BD/DNC neurologic examination cannot be assessed safely, clinicians must perform ancillary testing to complete the BD/DNC determination
Known cause of brain damage
- there must be no doubt about the cause of BD/DNC and the irreversibility of brain damage
- it may not be an etiological diagnosis (e.g., in the case of extensive intracranial hemorrhage, the exact etiology may not be known)
- death may be caused by a primary structural brain lesion or a secondary metabolic or hypoxic lesion causing brain edema
- when a patient is comatose, apneic, and has absent brainstem reflexes but there is not an identified mechanism of brain injury, there is a risk that the clinical findings may be caused by a reversible process
- exclude all potentially reversible causes:
- the effects of drugs altering the central nervous system function (sedatives, hypnotics, and opioids)
- the impact of myorelaxants or other agents that alter effective ventilation
- the metabolism of sedatives and myorelaxants may be significantly altered in critically ill patients, and their effects may persist for many hours after the last administration
- intoxication (a combination of alcohol and organic brain lesions is common)
- ensure the alcohol blood level, if clinically indicated, is ≤80 mg/dL
- if the patient has received pentobarbital, the level must be <5 μg/mL or below the lower limit of detection for that laboratory before evaluation for BD/DNC
- mydriatic agents may cause non-reactive mydriasis
- hypothermia
- may reduce the metabolic demands of brain cells and lead to a clinical image of “brain death”
- body temperature should be maintained ≥ 36°C before performing a BD/DNC evaluation
- severe metabolic and endocrine derangements
- severe hypotension ⇒ maintain SBP ≥100 mm Hg and mean arterial pressure (MAP) ≥75 mm Hg (AAN guidelines, 2023)
- patients with primary posterior fossa injury may be clinically comatose with brainstem areflexia and apnea; however, they may retain some cortical function
- to avoid determining BD/DNC in patients with primary posterior fossa injury and retained supratentorial function, clinicians should ensure that the posterior fossa process has also led to catastrophic supratentorial injury (as demonstrated by neuroimaging)
- neuroendocrine function can persist in patients with permanent injury to the brain and is not inconsistent with the whole brain standard of death
- diabetes insipidus is reported in up to 90% of adults with BD/DNC
- for patients who meet clinical criteria for BD/DNC, clinicians must assign the time of death as the time during the final apnea test (where PaCO2 and pH levels are consistent with BD/DNC criteria)
- for patients in whom an ancillary test is required and performed, the time of death is when an attending clinician (e.g., nuclear medicine physician or angiographer) documents in the medical record that the ancillary test results are consistent with BD/DNC
- once BD/DNC has been determined, the mechanical or pharmacologic support that maintains respiratory or cardiac function is generally discontinued unless organ donation is being considered
- pregnant patients who develop catastrophic, permanent brain injuries and may be determined to meet BD/DNC criteria (pregnancy is not a contraindication to BD/DNC evaluation)
- in these situations, the fetus may still be viable, and continued organ support may lead to the delivery of a viable newborn
- the ethical analysis of whether to continue organ support in a pregnant person determined BD/DNC should largely focus on the welfare of the fetus
Ancillary testing as part of the BD/DNC evaluation
- in most circumstances, the diagnosis of BD/DNC is based on the clinical demonstration of coma, absent brainstem reflexes, and apnea and does not require ancillary testing
- clinicians should only perform ancillary testing to assist with the diagnosis of BD/DNC when the BD/DNC neurologic examinations or apnea test cannot be completed, or the findings cannot be interpreted adequately (AAN guidelines, 2023)
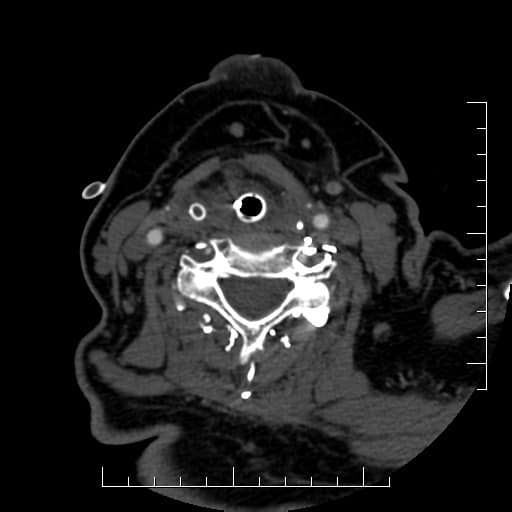
- injuries such as fractures of the cervical spine, skull base, or orbits, severe facial injuries or abnormalities that preclude accurate assessment of any components of the neurologic examination (with the exception of the OCR if untestable due to concern for C-spine or skull base integrity), or injuries to the cervical spinal cord that limit the adequate assessment of extremity movement or spontaneous respirations
- the inability to perform or complete the apnea test safely because of the patient’s risk of cardiopulmonary decompensation or the inability to interpret the PaCO2 levels in a patient with chronic hypercarbia for whom the chronic baseline PaCO2 level is unknown
- neurologic examination findings that may be difficult to interpret, such as limb movements that may or may not be spinally mediated
- metabolic derangements that are unable to be adequately corrected
- clinicians must not use ancillary tests to assist in the diagnosis of BD/DNC in the setting of hypothermia or high levels of sedating medications or to avoid performing otherwise testable elements of the BD/DNC assessment
- if ancillary testing is needed to diagnose BD/DNC, before proceeding to an ancillary test, BD/DNC neurologic examination(s) and apnea test(s) still need to be performed to the fullest extent possible, and findings must be consistent with BD/DNC
- if any findings on neurologic examination or apnea test are consistent with brain-mediated activity, the patient does not meet criteria for BD/DNC, and ancillary testing must not be performed
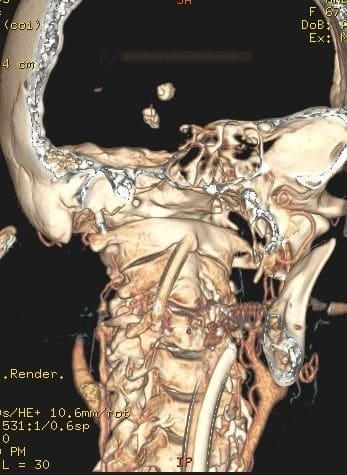
- confirmation of the cerebral circulatory arrest
- DSA
- CTA (not recommended by AAN guidelines 2023)
- TCD/TCCD
- perfusion scintigraphy
- functional testing (proof of absence of brain activity)
- EEG or evoked potentials (BAEP, SSEP) are not recommended by AAN guidelines 2023)
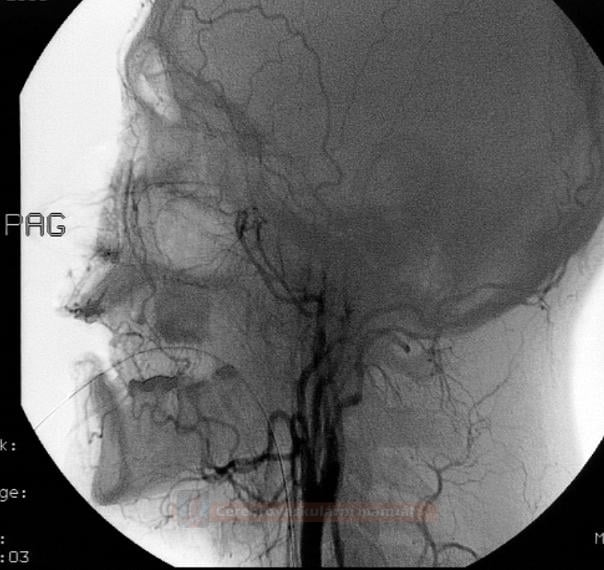
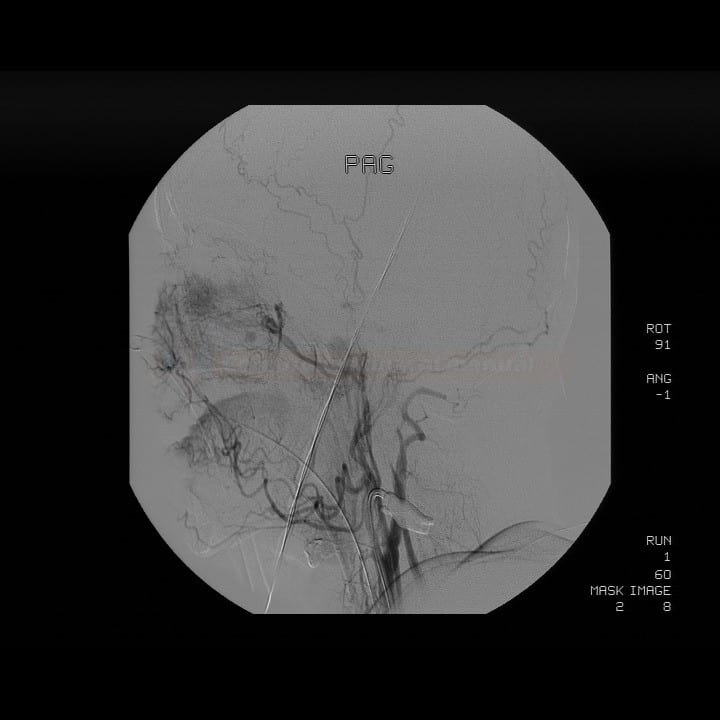
Digital subtraction angiography (DSA) |
- clinicians may use conventional 4-vessel catheter angiography as an ancillary test to aid in the diagnosis of BD/DNC (AAN guidelines, 2023)
- perform angiography with MAP > 60 mmHg
- technical aspects of DSA
- injection of contrast agent from the aortic arc – 0.5 mL/kg (minimum of 30 mg) at a rate of 15-25 mL/s
- selective angiogram of carotid arteries and one vertebral artery (CCA 5-8 mL at 4-8 mL/s, VA 3-6 ml at 4-6 mL/s)
- imaging should take ≥ 15 s after contrast administration
- both extra and intracranial circulation should be evaluated
- the circulatory arrest is confirmed when intracranial vessels are visualized only to the A1 and M1 segments and the proximal basilar artery (without filling of PICA and AICA)
- conventional angiographic evidence of cerebral circulatory arrest is of value only in the presence of concurrent clinical evidence of oblongata involvement
- in proven cerebral circulatory arrest, the oblongata survival with persistent reflexes (gag or oculocardiac reflexes) can be explained by collaterals from the spinal arteries
- conventional angiographic evidence of cerebral circulatory arrest is of value only in the presence of concurrent clinical evidence of oblongata involvement
- in patients with a traumatic calvarial defect or after craniectomy, some cerebral blood flow may be preserved. Intracranial penetration of contrast agent does not exclude brain death. However, in these patients, brain death cannot be confirmed by angiography (⇒ perform BAEP)
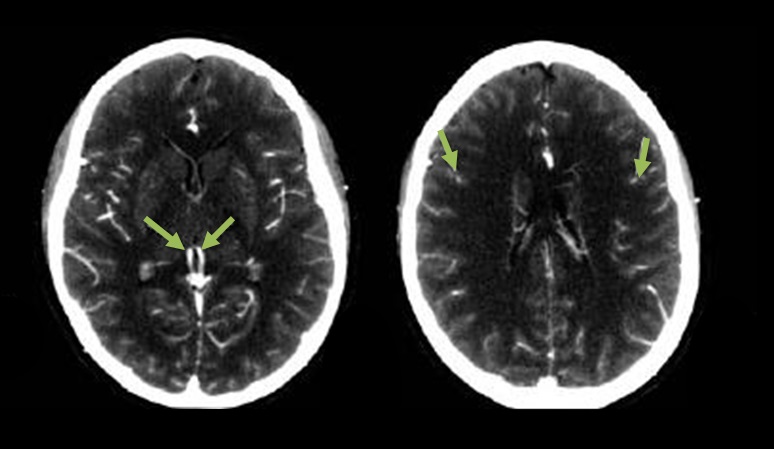
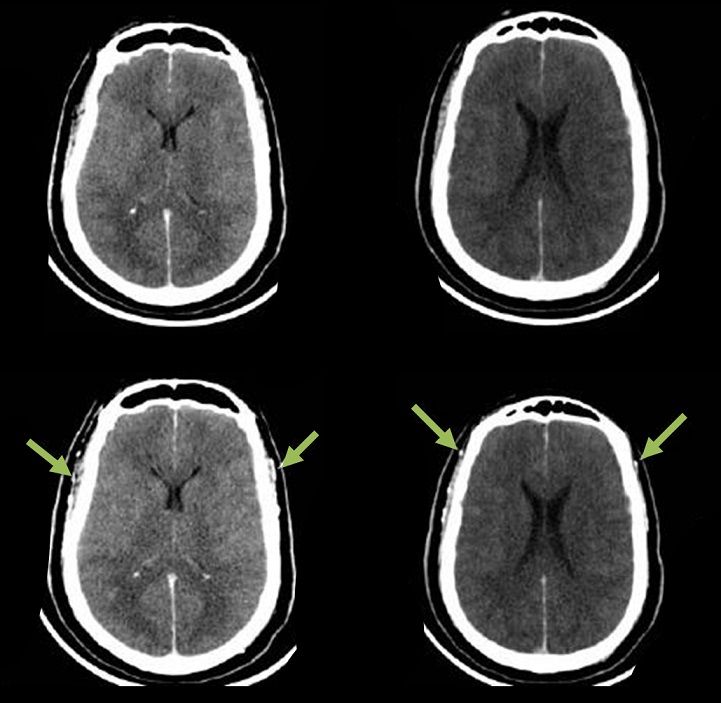
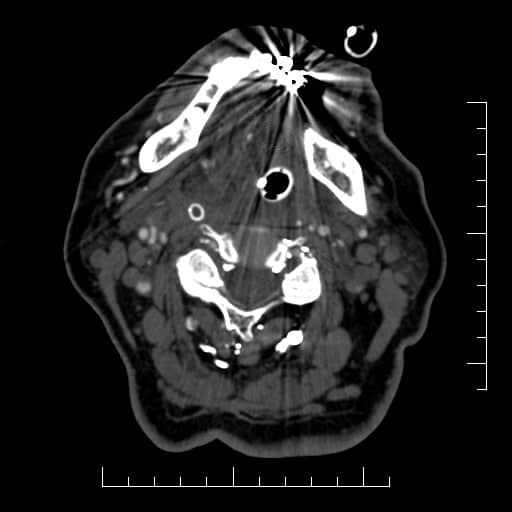
CT angiography
|
- available data demonstrate a lack of validation and the potential for false positives
- variations in protocols with different sensitivities and specificities, contrast injection parameter variation and limited data that compare this technique with other tests of cerebral blood flow currently relegate CT angiography as only investigational as an ancillary test to assist with BD/DNC determination (AAN guidelines, 2023)
- clinicians should not use MRI or MRA as an ancillary test to aid in the diagnosis of BD/DNC (AAN guidelines, 2023)
- however, CTA is used as the official method for confirming cerebral circulatory arrest in many countries
- MAP > 60 mmHg should be maintained during the examination
- technical implementation of CTA: [Frampas, 2009]
- IV administration of 60-120 mL of contrast agent (arterial phase), use 2 mm slices
- helical CT performed 60 seconds after administration of contrast agent (venous phase)
- originally, a 7-point scale was used to assess the absence of distal cerebral artery filling 60s after contrast agent administration [Dupas, 1998]
- assessed vessels:
- pericallous artery
- cortical MCA segments (M4)
- internal cerebral veins + vein of Galen
- a score of 7 indicates cerebral circulatory arrest and corresponds with clinical signs of brain death
- assessed vessels:
- a 4-point scale with high sensitivity and specificity was published in 2009 [Frampas, 2009]
- vessels assessed:
- right and left internal cerebral veins
- right and left M4 branches of the MCA
- absence of filling in all 4 regions indicates a score of 4 and is associated with clinical signs of brain death
- vessels assessed:
Transcranial Doppler sonography (TCD, TCCD) |
- clinicians may use TCD/TCCD in adult patients as an ancillary test to aid in the diagnosis of BD/DNC ⇒ confirmation of cerebral circulatory arrest (AAn guidelines, 2023)
- it should not be used in children
- non-invasive, with good availability and the possibility of monitoring/serial examinations
- vessels to be examined: ICA, MCA, PCA, ACA, VA, BA (access via foramen magnum, temporal window, or orbit)
- detection of oscillating flow or systolic spikes in proximal large intracranial arteries is consistent with BD/DNC in adults
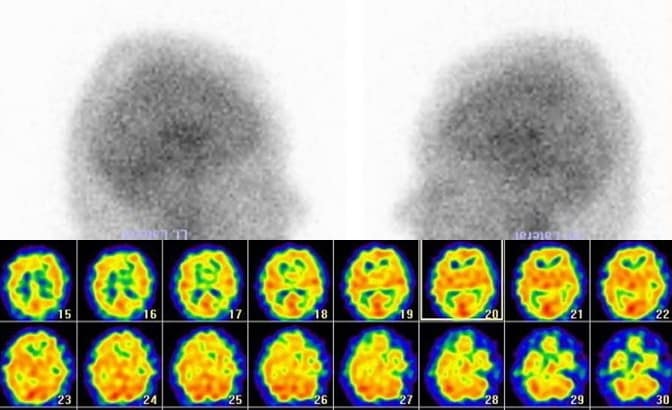
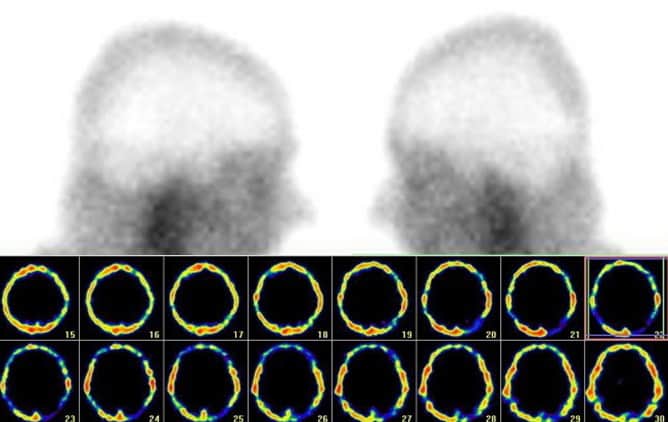
Brain perfusion scintigraphy |
- clinicians may use radionuclide perfusion scintigraphy as an ancillary test to aid in the diagnosis of BD/DNC (AAN guidelines, 2023)
- the principle of the method IV bolus of radioactive technetium followed by several minutes of brain perfusion imaging
- Tc 99m hexamethyl propylene amine oxime and Tc 99m ethyl cysteinate dimer are lipid soluble and brain-specific agents
- MAP > 80 mmHg is required during the scan
- dynamic and static scintigraphy + SPECT imaging are performed
- brain death is indicated by a complete absence of brain perfusion
Electroencephalography (EEG) |
- clinicians should not use EEGs as ancillary test to assist with the diagnosis of BD/DNC (AAN guidelines, 2023)
- it assesses the function of the cerebral hemispheres and not deeper structures, notably the brainstem
- the absence of any detectable EEG activity does not provide information about the presence or absence of brainstem function
- the addition of AEPs and SEPs cannot completely compensate for this inherent limitation of EEG for the purpose of assisting with BD/DNC determination
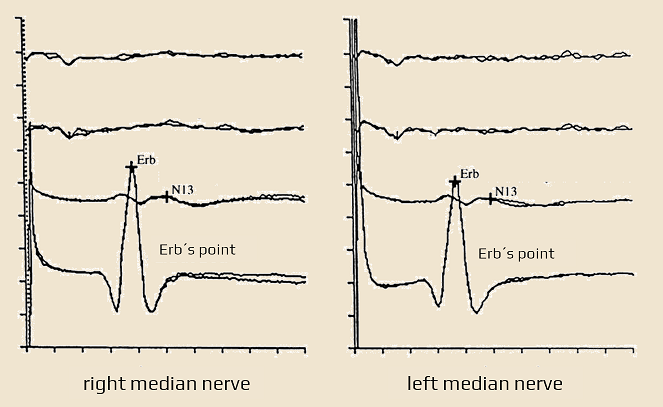
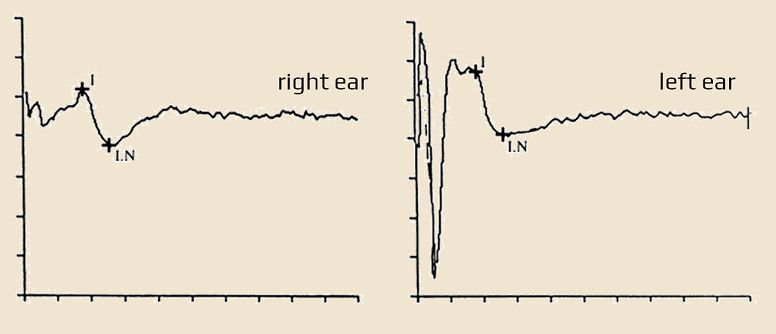
Evoked potentials (EP)
|
- clinicians should not use AEPs or SEPs as ancillary tests to assist with the diagnosis of BD/DNC (AAN guidelines, 2023)
SSEP (SomatoSensory Evoked Potentials)
- potentials evoked by bilateral median nerve stimulation show responses only from Erb’s point and the spinal component (N13)
- cortical and subcortical responses are absent
BAEP (Brainstem Auditory Evoked Potential)
- BAEP directly tests the function of the receptor, vestibulocochlear nerve, inferior pons, mesencephalon, and diencephalon; it does not test the medulla oblongata
- the test requires intact receptor structures (exclude bilateral fractures of the temporal bone and trauma to the auditory system!)
- BAEP is virtually unaffected by pharmacotherapy, incl. medically induced coma
- findings associated with brain death:
- bilateral disappearance of waves II-V with preservation of wave I (this excludes peripheral lesions)
- the disappearance of all components
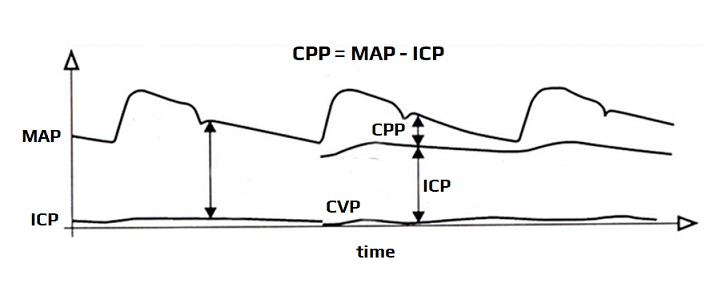
Cerebral perfusion pressure (CPP) monitoring |
- this method is not mentioned in AAN guidelines 2023
- CPP represents the difference between mean arterial pressure (MAP) and intracranial pressure (ICP), measured in mmHg
- continuous invasive ICP monitoring is required
- cerebral perfusion arrest occurs when ICP ≥ MAP