ADD-ONS
Hemorrhagic Complications in Acute Ischemic Stroke
Updated on 03/03/2024, published on 26/04/2021
- hemorrhagic complications are a serious concern in acute ischemic stroke; they can be divided into two main categories:
- early hemorrhagic complications – occurring within 24 hours of stroke onset
- most commonly due to reperfusion injury when a blood clot is dissolved by thrombolytic therapy or spontaneous recanalization; SAH or remote ICH are rare
- late hemorrhagic complications
- early hemorrhagic complications – occurring within 24 hours of stroke onset
- risk factors for hemorrhagic complications:
- age
- older patients generally have a higher risk of hemorrhagic complications, possibly due to the increased prevalence of other risk factors like hypertension and the use of anticoagulants
- thrombolytic therapy
- the overall efficacy of intravenous thrombolysis has been demonstrated despite the known increased risk of bleeding
- poorly controlled hypertension during thrombolysis
- stroke severity and presence of extensive early signs of ischemia (late recanalization)
- larger lesions carry a higher risk of hemorrhagic transformation or complications
- comorbidities (hypertensive angiopathy, CAA, uncontrolled diabetes, etc.)
- concurrent antithrombotic medication
- prior hemorrhagic stroke
- age
- understanding the risk factors for hemorrhagic complications is crucial, especially given the delicate balance between treating the stroke and avoiding additional harm
- different classifications of hemorrhagic transformation have been used:
- CT-based classification does not provide direct information on the clinical consequences of hemorrhage
- clinical classification does not acknowledge the contribution of ischemic edema to clinical deterioration
- the use of both clinical and radiologic criteria seems optimal
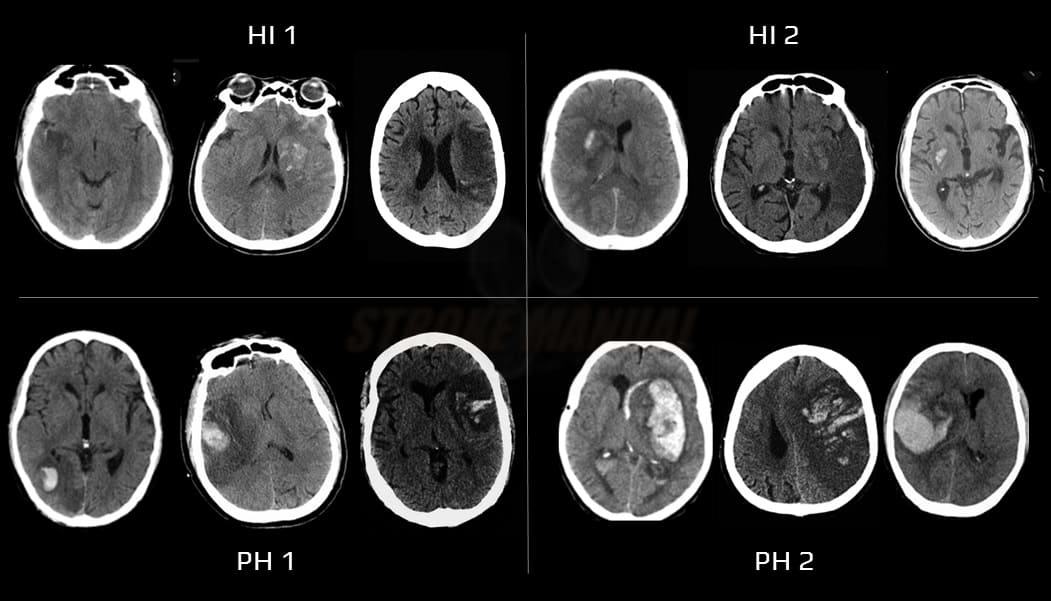
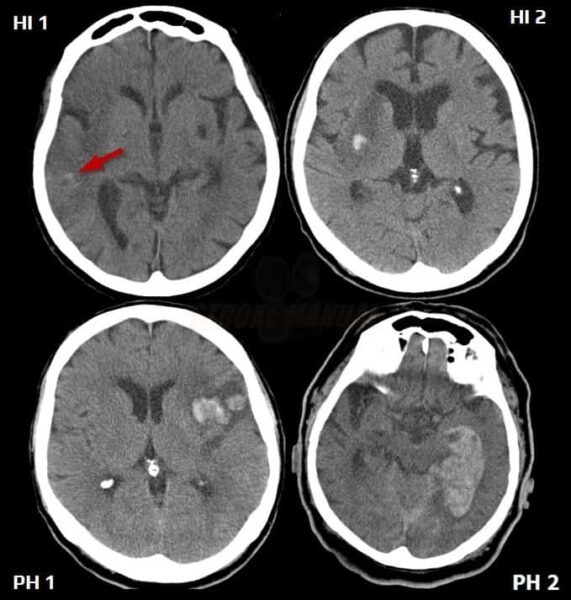
ECASS group hemorrhage classification
| Radiologic hemorrhage classification (Larrue, 2001) | |
| Hemorrhagic infarction (HI) – petechiae in the infarcted tissue without space-occupying effect |
|
| HI1 | small isolated petechiae along the margins of the infarct |
| HI2 | confluent petechiae |
| Parenchymal hemorrhage (PH) – hemorrhage with space-occupying effect |
|
| PH1 | blood clots in ≤ 30% of the infarct area with a slight space-occupying effect |
| PH2 | blood clots in > 30% of the infarct area with a substantial space-occupying effect |
Definitions of symptomatic hemorrhage (sICH)
| Definition of a symptomatic intracranial hemorrhage (SICH) in different trials |
|
|
|
| any hemorrhage + any clinical deterioration | |
| local or remote parenchymal hemorrhage type 2 (PH2) + clinical deterioration (NIHSS increase ≥ 4 or death) within 24 hours |
|
new intracranial hemorrhage detected by CT/MRI associated with any of the following:
|
|
The Heidelberg Bleeding Classification
| 1 | Hemorrhagic transformation of infarcted brain tissue | |
| 1a | Scattered small petechiae, no mass effect (HI1) |
|
| 1b | Confluent petechiae, no mass effect (HI2) |
|
| 1c | Hematoma within infarcted tissue, occupying <30%, no substantive mass effect (PH1) |
|
| 2 | Intracerebral hemorrhage within and beyond infarcted brain tissue | |
| Hematoma occupying 30% or more of the infarcted tissue, with obvious mass effect (PH2) |
||
| 3 | Intracerebral hemorrhage outside the infarcted brain tissue or intracranial-extracerebral hemorrhage | |
| 3a | Parenchymal hematoma remote from infarcted brain tissue | |
| 3b | Intraventricular hemorrhage | |
| 3c | Subarachnoid hemorrhage | |
| 3d | Subdural hemorrhage | |