INTRACEREBRAL HEMORRHAGE / VASCULAR MALFORMATIONS
Dural arteriovenous fistula (DAVF)
Updated on 29/02/2024, published on 21/04/2021
- dural arteriovenous fistula (DAVF) is characterized by abnormal connections (shunts) between an artery and a vein; DAVF typically presents with tinnitus, hemorrhage, or venous hypertension
- DAVF accounts for ∼ 10-15% of vascular malformations and most commonly affects patients aged 40-60 years
- most DAVFs are idiopathic; some patients have a history of previous craniotomy, head trauma, or dural sinus thrombosis [Gandhi, 2012]
Pathology
- DAVFs usually have multiple feeders
- supratentorial
- middle meningeal artery, superficial temporal artery (from ECA)
- ethmoidal branches of the ophthalmic artery
- cavernous sinus (ICA and/or ECA branches) → Carotid-cavernous fistula (CCF)
- posterior fossa
- vertebral arteries
- occipital artery (fom ECA)
- supratentorial
- most typical drainage paths:
- transverse/sigmoid sinus (usually fed by the occipital artery) → Anatomy of cerebral veins and sinuses
- cavernous sinus (Carotid-cavernous fistula)
- superior sagittal sinus (SSS)
- straight sinus
- cortical veins
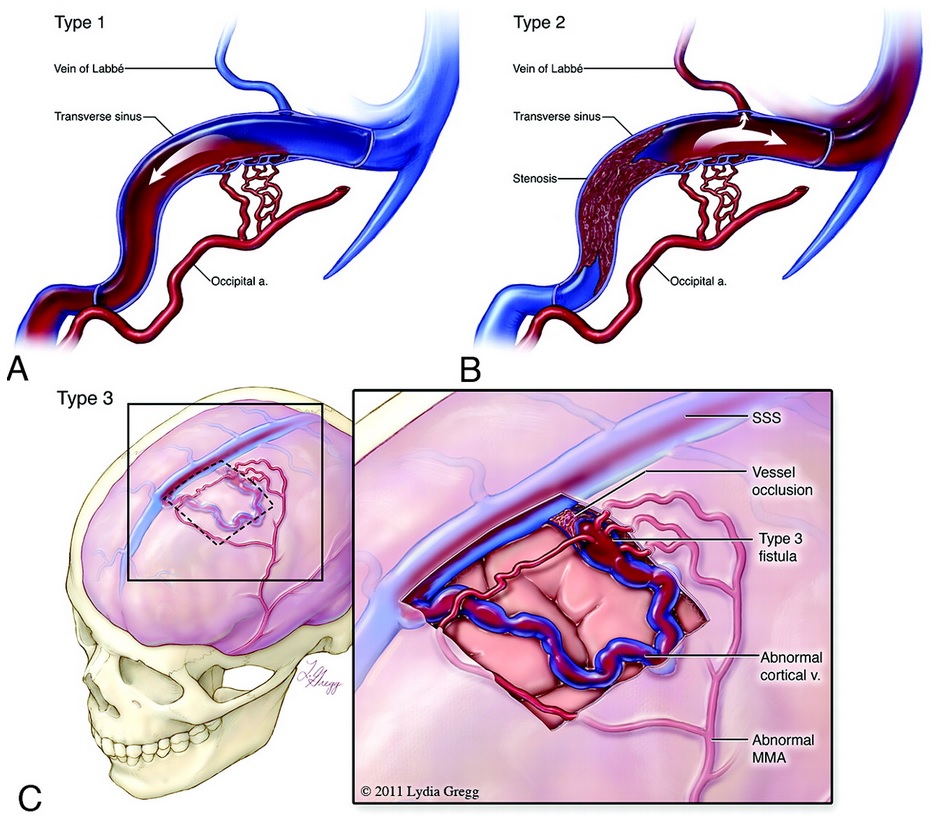
Classification
|
Borden [Borden, 1995]
|
|
|
Type I – anterograde drainage directly into dural venous sinuses/meningeal veins
Ia – 1 feeding artery Ib – >1 feeding arteries |
|
|
Type II – anterograde drainage into dural sinuses/meningeal veins + retrograde drainage into subarachnoid veins
|
|
|
Type III – predominantly retrograde drainage into cortical veins with their dilatation, no dural sinus or meningeal venous drainage
|
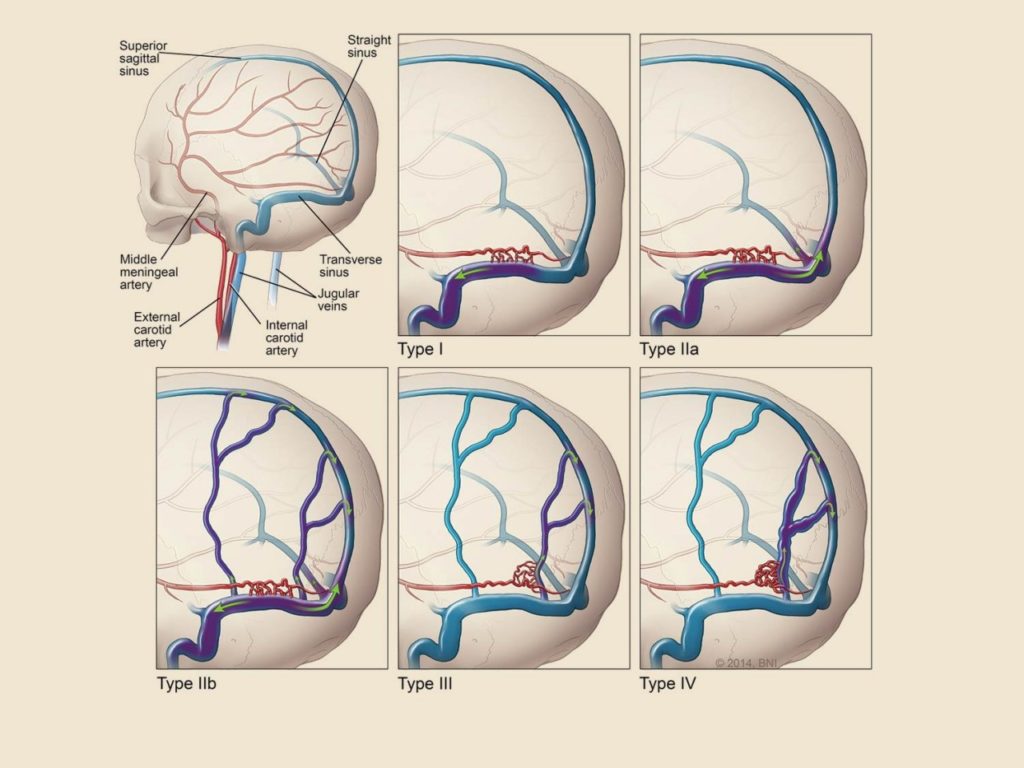
| Cognard [Cognard, 1995] This classification provides valuable data for the determination of the risk with each dural AV fistula and enables decision-making about the appropriate therapy |
|
|
Type I – only anterograde drain into dural sinuses, benign course
|
|
Type II
|
|
Type III, IV, V – no dural sinus drainage (high risk of bleeding – 40-65%)
|
Clinical presentation
Clinical presentation is variable and depends on the location of the fistula and the pattern of venous drainage. Common symptoms include:
- pulsatile tinnitus (typically with sigmoid and transverse sinus drainage)
- symptoms of venous hypertension/congestion
- headache and facial swelling
- hemorrhagic venous infarction
- spinal myelomalacia
- cranial nerve palsies (such as abducens palsy with diplopia)
- ocular (orbital) symptoms – conjunctival chemosis and swelling (carotid-cavernous fistula) – DDx of cavernous sinus thrombosis!
- intracerebral or subarachnoid hemorrhage (high risk, especially with type II and III) [Li, 2015]
- type II and III have an annual risk of ~8% [Gandhi, 2012]
- DAVF can be high-flow and consume a significant portion of ejection fraction (EF) => exertional dyspnea, left ventricular hypertrophy (LVH)
Diagnostic evaluation
- CT/MRI
- more useful for detecting complications (hemorrhage, venous infarction, edema)
- insufficient for diagnosing DAVF itself – vascular imaging must be added (however, enlarged arterial feeders or dilated pial vessels in the subarachnoid space may sometimes be seen)
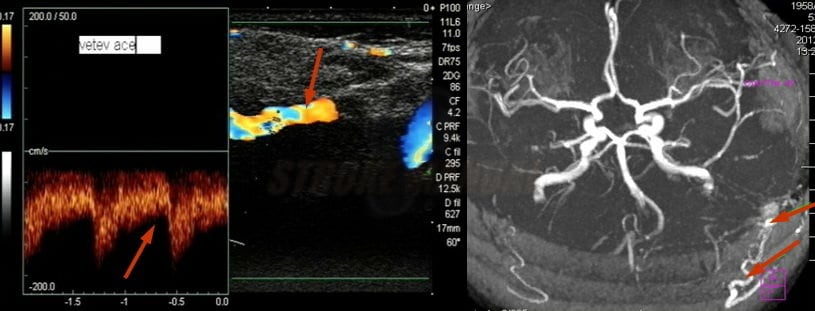
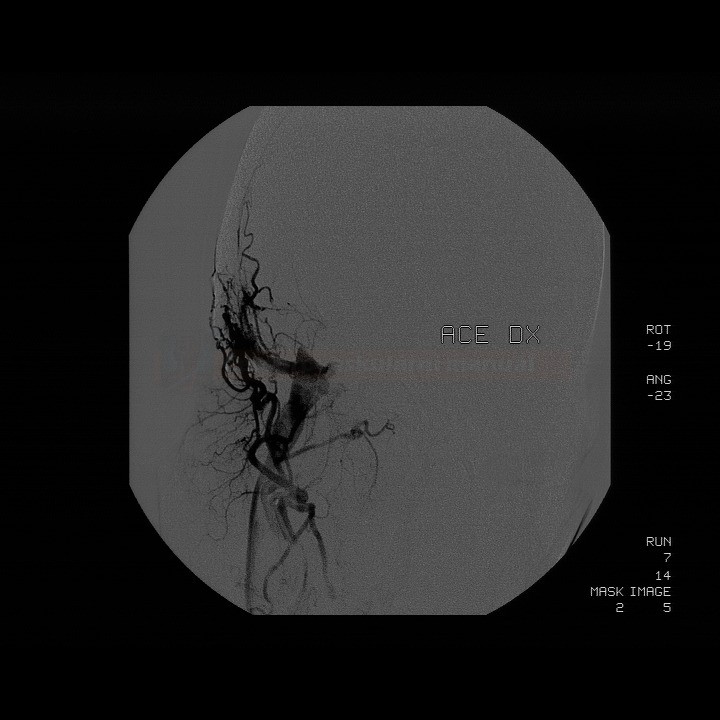
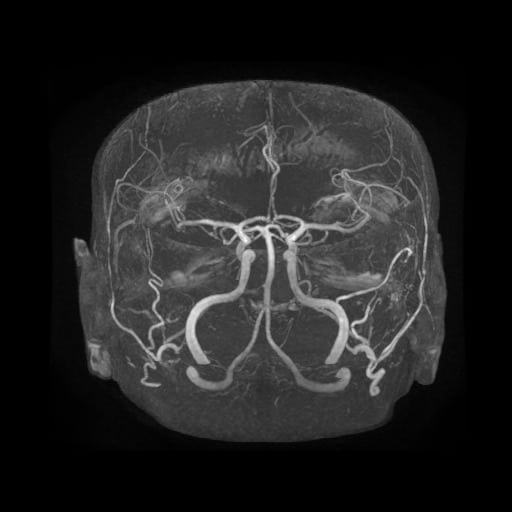
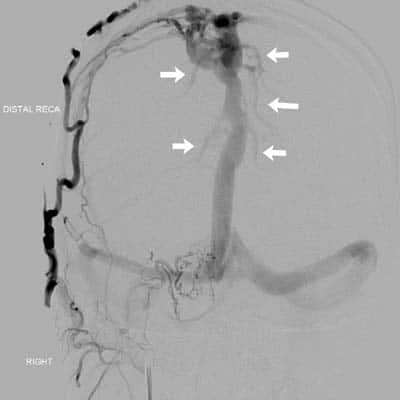
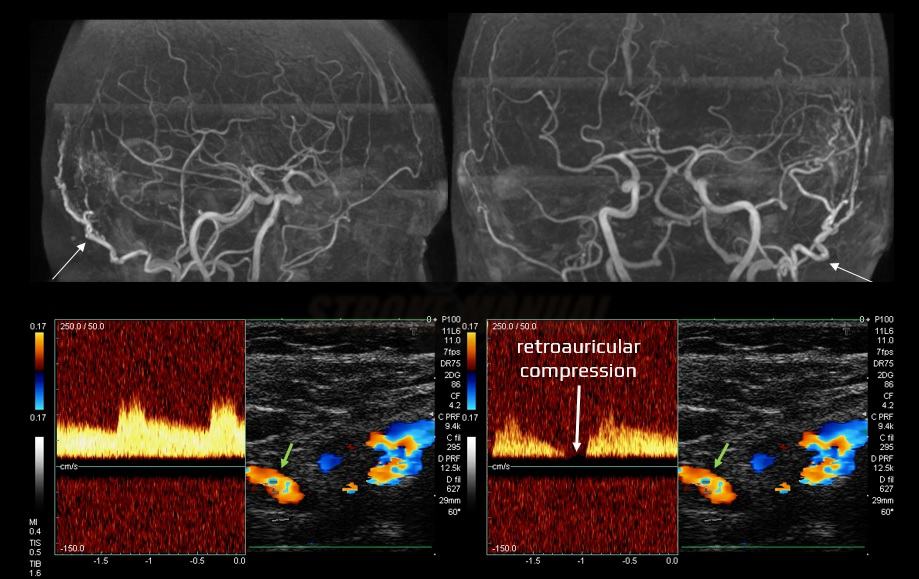
- vascular imaging (CTA/MRA or DSA)
- often, multiple feeders are present without an intervening nidus
- dural sinuses are filled with contrast during the arterial phase
- dilated and tortuous cortical veins in the subarachnoid space
- DSA remains the best method to accurately assess feeding vessels and the presence and extent of retrograde venous drainage
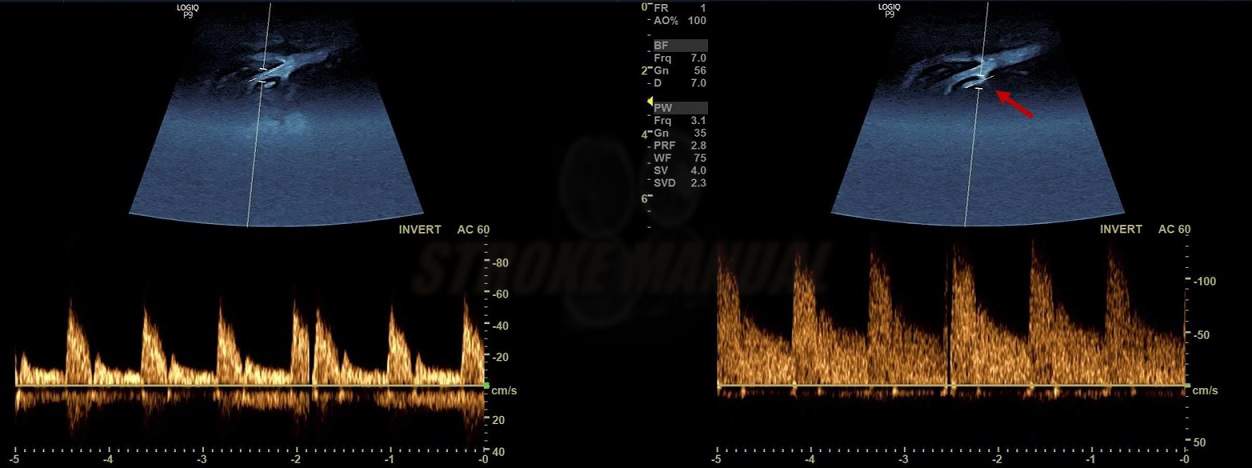
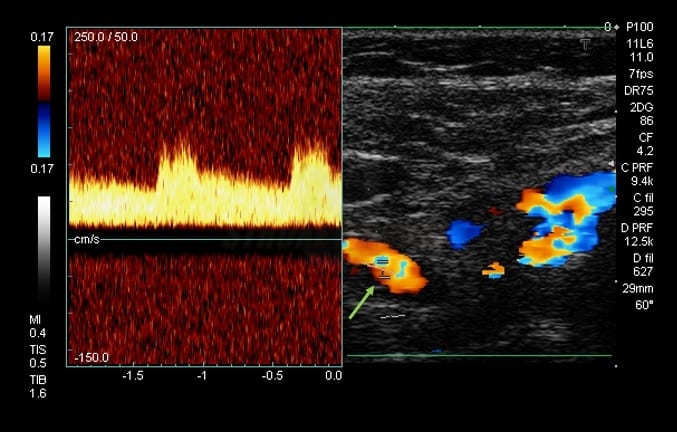
- neurosonology
- Doppler can show decreased resistance (RI< 0.45) and increased flow velocity
- not as sensitive as CTA/MRA or DSA for diagnosing DAVFs
Management
- treatment decision is based on the following factors:
- type of the fistula
- patient’s age and comorbidities (older patients and those with comorbidities may be better candidates for conservative treatment)
- presence of symptoms attributable to the fistula
Endovascular and surgical treatment
- typically considered for DAVFs with a higher risk of bleeding, such as Borden II and III or Cognard IIb-V DAVFs (an annual risk ~ 8%)
- type I with severe tinnitus may also be indicated for endovascular treatment
Endovascular treatment
- endovascular treatment involves occluding the abnormal connection between the artery and vein using embolization techniques
- transarterial approach (TAE) – super-selective distal catheterization with injecting embolic agents into the feeding arteries
- e.g., using Onyx [Lv, 2009]
- transvenous approach (TVE) – involves occluding the venous drainage pathways; mainly used in cases with multiple small feeding arteries unsuitable for embolization
- combined approach (TAE + TVE)
Surgery
- typically reserved for cases where endovascular treatment is not possible or has been unsuccessful/partially successful
Stereotactic radiosurgery (SRS)
- a minimally invasive second-line treatment option if endovascular or surgical treatment is not feasible or has been unsuccessful
- typically dose of 20-30 Gy is used ⇒ irradiated vessels become thrombosed
- obliteration is gradual, occuring within 2-3 years
- unsuitable as primary treatment if there is reflux into cortical veins