ISCHEMICKÉ CMP / KLASIFIKACE A ETIOPATOGENEZE
Neurosarcoidosis
Updated on 14/06/2024, published on 02/03/2024
- sarcoidosis is a multisystem granulomatous disorder of unknown etiology, usually affecting younger people (most commonly between 25-50 years of age), more prevalent in women
- neurosarcoidosis = manifestation of sarcoidosis in the central nervous system
- rare but serious disease (~ 5-10% of cases; exact prevalence can vary, and some cases may be asymptomatic or mildly symptomatic)
- mostly accompanied by systemic symptoms and intrathoracic involvement
- isolated nervous system involvement is extra rare [Hodge, 2007]
- diagnosis is challenging and often requires a combination of clinical presentation, imaging findings, histological confirmation, and exclusion of other causes of granulomatous inflammation
Etiopathogenesis
- the exact cause of sarcoidosis is unknown
- it is believed to involve an aberrant immune response to an unknown noxious agent in a genetically predisposed individual
- histologically, neurosarcoidosis involves the formation of granulomas
- the lesions contain T lymphocytes, macrophages, and epithelioid cells
- sarcoidosis is associated with increased synthesis of ACE (angiotensin-converting enzyme) and 1,25-dihydroxycholecalciferol with subsequent hypercalcemia and hypercalciuria
- an elevated immunoregulatory index in bronchoalveolar lavage fluid serves as an important marker in the diagnosis of sarcoidosis
- this elevation reflects an imbalance between helper (CD4+) and suppressor (CD8+) T-cells, typically demonstrating an increased CD4+/CD8+ ratio
Vascular involvement in neurosarcoidosis
- typical manifestation of neurosarcoidosis is progressive encephalopathy rather than stroke [Brown,1989]
- however, case reports have been published describing the combination of neurosarcoidosis and stroke [Corse, 1990] [Nakagaki, 2004] [Hodge, 2007]
- various mechanisms may be involved:
- arteriolopathy due to perivascular granulomatous inflammation
- cardioembolic stroke due to cardiomyopathy or arrhythmias
- compression of large arteries by adjacent granulomas
- inflammation of large artery walls with thrombus formation (vasculitis)
- coagulation and fibrinolysis disorders [Hasday, 1988]
- venous sinus thrombosis (⇒ venous infarction) due to a hypercoagulable state or direct sinus infiltration
Clinical presentation of neurosarcoidosis
- neurosarcoidosis occurs in 5-10% of cases; almost all of these patients have known concomitant extracerebral involvement
- clinically, focal symptoms, encephalopathy, and epileptic seizures predominate
- spinal cord involvement usually has a subacute course, with long T2 lesions (more than 3 segments) with irregular enhancement; shorter multifocal lesions without enhancement have also been reported
- the definitive diagnosis of sarcoidosis is usually made only by biopsy
| Most commonly affected organs in sarcoidosis: |
|
-
meningeal involvement (10-25%)
-
hydrocephalus (10%)
-
parenchymal involvement (50%)
-
vasculopathy (5-10%) with ischemic stroke
-
cranial neuropathy (50-75%)
-
most commonly CN II, V, VII, VIII
-
-
diabetes insipidus or other endocrine disorders
- dural sinus thrombosis (presumably due to either an acquired coagulopathy or direct infiltration of the sinus)
-
infiltration of meninges and spinal cord; large extramedullary granulomas compressing the spinal cord are rare
- mostly subacute/chronic myelopathy; cauda equina syndrome may occur
- T2 hyperintense lesions over 3 segments with irregular enhancement are typical (shorter multifocal lesions without enhancement have also been described!) – DDx of acute transverse myelitis
-
mononeuritis multiplex
-
cranial neuropathy
-
polyradiculopathy, plexopathy
-
Guillain-Barré syndrome
-
symmetrical sensorimotor, sensory, or motor polyneuropathies
-
symptomatic and asymptomatic
-
biopsy demonstrates typical granulomas with giant cells
Diagnostic evaluation
Sarcoidosis should always be considered in the differential diagnosis of multifocal nervous system involvement
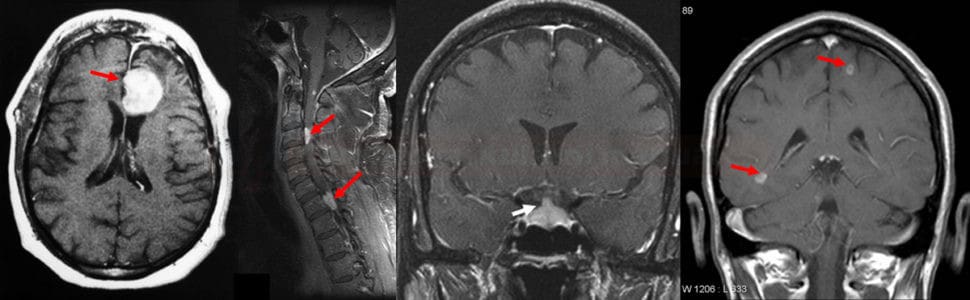
- neurosarcoidosis can affect various neural structures; MRI is the preferred diagnostic method
-
leptomeninegal involvement is best seen on contrast-enhanced MRI; enhancement may be nodular or diffuse
-
parenchymal lesions are best seen on T2 images
-
granulomas are hyperintense in T2, often localized in periventricular white matter, hypothalamus, pituitary gland or brainstem
- granulomas are most often small, but some may be as large as a few centimeters
- some lesions show postcontrast enhancement
-
spinally granulomas may cause mass effect within the spinal canal
-
- cranial nerve involvement (especially the facial and optic nerves)
- hydrocephalus can occur due to the obstruction of cerebrospinal fluid (CSF) pathways by granulomas or meningeal involvement
- sarcoid granulomas can affect the dura mater and skull bones, visible as dural thickening or lytic bone lesions
- DWI may demonstrate recent ischemia
- MRI findings in neurosarcoidosis are not specific and can mimic other conditions such as multiple sclerosis, CNS lymphoma, or infectious meningitis; MRI results must be interpreted in conjunction with clinical findings and other diagnostic tests
-
normal in up to 30% of cases
- pathologic findings
-
chronic inflammation with lymphocytic pleocytosis and increased protein levels
-
reduced glucose levels
-
positive oligoclonal bands
-
Angiotensin-converting enzyme (ACE)
- produced by epithelioid cells that are part of granulomas
- an increase below twice the upper limit of normal is nondiagnostic
- an increase above twice the normal suggests diagnosis of sarcoidosis, but the finding is not specific (also ↑ in TB, histoplasmosis, Crohn etc.)
- the sensitivity of the test is reported to be ~ 50%
- the value of serum ACE is also affected by polymorphisms in the gene for this enzyme and cannot be applied in patients who are treated with ACE inhibitors
Hypercalcinemia and hypercalciuria
- caused by the uncontrolled conversion of 25-cholecalciferol to 1,25-dihydroxycholecalciferol (calcitriol – active vitamin D3)
- conversion occurs in the epithelioid cells of the granuloma, and therefore, calcium levels normalize with corticosteroid therapy
- it is more often seen in the summertime when calcium is also reabsorbed by the intestine at an increased rate when vitamin D is externally activated
Hypergammaglobulinemia
- a typical finding in sarcoidosis
- elevated IgG, IgA, and IgM levels without monoclonal gammopathy are present
- circulating immune complexes (CIK) tend to be elevated in the acute stage
- intrathoracic lymphadenopathy with a predilection to the upper and middle regions of the lungs with perihilar distribution
- lesions are located along the bronchovascular bundles and lymphatic vessels
- 5 stages are distinguished on the chest X-ray (Scadding, 1961)
- stage 0 – no radiographic evidence of intrathoracic sarcoidosis
- stage 1 – bilateral hilar lymphadenopathy without pulmonary parenchymal involvement
- stage 2 – bilateral hilar lymphadenopathy with pulmonary infiltrates
- stage 3 – pulmonary infiltrates without hilar lymphadenopathy; the disease has progressed to affect the lung tissue with scarring or granulomas, while the hilar lymph nodes may no longer be enlarged or may have returned to normal size
- stage 4 – irreversible pulmonary fibrosis, leading to distortion of the lung architecture, volume loss, and possibly the development of bullae. This stage is associated with significant morbidity and potential for respiratory failure
- stage 0 – no radiographic evidence of intrathoracic sarcoidosis
- HRCT of the chest during initial evaluation is suggested, as it offers a better definition of lung parenchymal and airway abnormalities as well as vascular structures (Levy, 2018)
- definitive diagnosis of neurosarcoidosis is based on histologic confirmation
- direct brain biopsy is less common because of the potential risks
- more commonly, biopsy of more accessible tissues demonstrating granulomatous inflammation may support the diagnosis of neurosarcoidosis
- transbronchial biopsy (TBB) is preferred in cases of pulmonary impairment
- bioptic material can also be obtained from other sites (peripheral nodules, muscles, skin)
- biopsy typically reveals non-caseating granulomas formed by clusters of inflammatory cells without central necrosis
- these granulomas are often surrounded by a rim of lymphocytes and occasionally fibrosis
- the absence of central necrosis helps distinguish sarcoidosis from other granulomatous diseases such as tuberculosis and fungal infections
- used in the assessment of extrapulmonary involvement
- radioactive glucose is uptaken in organs with active inflammation
- due to the relatively high radiation load, it is used mainly in the differential diagnosis of lymph node involvement
- it cannot distinguish sarcoidosis from lymphoma
Diagnostic criteria
|
Diagnosis of neurosarcoidosis
|
Possible
|
|
Probable
|
|
Definitive
|
Therapy
- clear indication for treatment :
- hypercalciuria (hypercalcemia)
- severe organ lesions (neurosarcoidosis, cardiac sarcoidosis, ocular forms not responding to local therapy, posterior uveitis, optic neuritis, torpid skin lesions, etc.)
- treatment of isolated pulmonary involvement is debated due to the variety of stages, and possible spontaneous reversibility
- spontaneous remission occurs in 55-90% of stage I patients, 40-70% in stage II, and 10-20% in stage III.
- according to most guidelines, pulmonary forms with mild (to moderate) pulmonary function impairment without clinical symptoms are not treated
- symptomatic patients are treated
Corticosteroids
- start with prednisone 20-40 mg daily
- when other corticosteroid-sparing drugs are added (methotrexate, azathioprine, and others listed below), the corticosteroid dose can be reduced
- the effect of treatment is expected within the first 6 weeks and is evaluated after 3-6 months
- when the effect is seen, the dose is slowly reduced to 5-10 mg/d and continued for a total of 6-12 months
- in severe forms, a pulse IV therapy is suggested – prednisolone 0.5-1g daily for 3 days
Immunosuppressive drugs
- if remission is not maintained with prednisone dose < 10 mg/day alone, corticosteroid-sparing drugs should be added
- methotrexate 10 mg/week for 3-6 months
- azathioprine 2-2.5mg/kg/d for 3-9 months
- for CNS impairment, a dose of 150 mg/d is suggested
- for CNS impairment, a dose of 150 mg/d is suggested
- cyclosporin A, mycophenolate mofetil, tacrolimus
Antimalarial drugs
- hydroxychloroquine (PLAQUENIL) 200-400mg/d – especially in patients with hypercalcemia, skin and neurological impairment