NEUROSONOLOGY
Intima-media thickness (IMT)
Updated on 19/06/2024, published on 26/03/2021
- the measurement of carotid intima-media thickness (IMT, CIMT) can quantify atherosclerosis burden in asymptomatic patients, which may require a more aggressive approach to managing vascular risk factors
- decades of silent arterial wall alterations precede atherosclerotic disease with clinically evident cardiovascular events
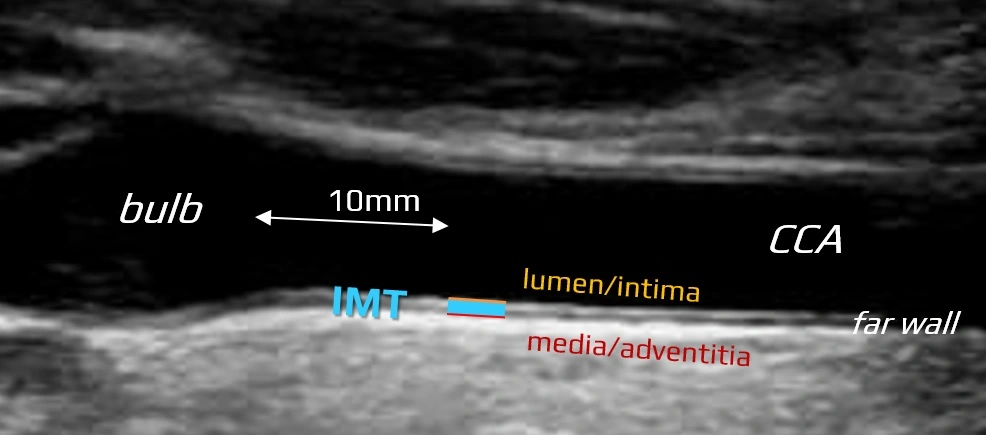
- the first detectable morphological abnormalities (enlargement of intima-media) can be visualized using B-mode imaging
- the intima-media extends from the luminal edge of the artery to the boundary between the media and the adventitia
How to measure IMT?
- the standard measurement is performed in B-mode on the far wall of the common carotid artery (CCA), 10 mm proximal to the bifurcation
- use high-resolution images and adjust depth of focus and gain settings to obtain optimal image quality
- employ linear ultrasound transducers at frequencies above 7 MHz
- optimize the insonation angle (90° to the vessel wall)
- values obtained from different sites (such as distal ICA, bulb) should be documented separately
- values from the near wall are dependent on gain settings and are thus less reliable
- measure the distance between the 2 parallel echogenic lines
- the first line represents the lumen-intima interface
- the seond line represents the media-adventitia interface
- obtain at least five measurements on each side and calculate the average value (“average IMT”); specialized software may be helpful
 [Baldassare, 2000]
[Baldassare, 2000]
- automated systems can rapidly provide the mean maximal value of 150 measurements performed over a 10 mm segment of the CCA
- perform IMT measurements in a region free of atherosclerotic plaque, which is defined as:
- lesion ≥1.5 mm
- structure encroaching into the arterial lumen by at least 0.5 mm or 50% of the surrounding IMT value
- lesion ≥1.5 mm
- interadventitial and lumen diameter must also be obtained, as IMT correlates with arterial diameter
- echogenicity, especially of the media, may be increased in the presence of fatty infiltration and thickening
What is normal IMT?
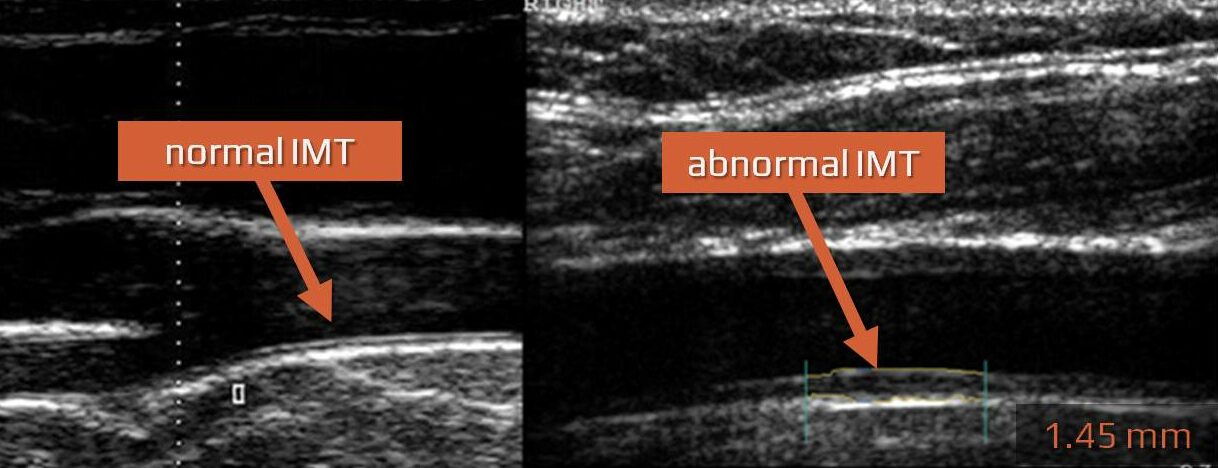
- IMT > 75-95th percentile for age and sex is considered abnormal
- some authors suggest simple cut-off values:
- IMT < 0.8 mm – value associated with normal healthy individuals
- IMT ≥ 1 mm – value associated with atherosclerosis and a significantly increased risk of cardiovascular disease (CVD) in any age group
| Women (95. percentile) |
Men (95. percentile) |
||||
|
45 y
|
55 y |
65 y |
45 y | 55 y |
65 y |
|
0.73
|
0.91 | 1.04 |
0.89
|
1 | 1.3 |
95.th percentile [Howard, 1993]
| Age |
P25 | P50 |
P75 |
| men <30 | 0.39 | 0.43 | 0.48 |
| men 31-40 | 0.42 | 0.46 | 0.50 |
| men 41-50 | 0.46 | 0.50 | 0.57 |
| men >50 | 0.46 | 0.52 | 0.62 |
| women <30 | 0.39 | 0.40 | 0.43 |
| women 31-40 | 0.42 | 0.45 | 0.49 |
| women 41-50 | 0.44 | 0.48 | 0.53 |
| women >50 | 0.50 | 0.54 | 0.59 |
Prognostic value of IMT measurement
- not only atherosclerotic plaques but also IMT can quantify atherosclerosis burden in asymptomatic patients
- IMT should be assessed in each extracranial ultrasound examination
- increased IMT represents the first stage of atherosclerosis and, if left untreated, is followed by plaque formation
- clinical and epidemiological studies have shown an association between IMT and coronary artery disease (CAD), stroke, and peripheral vascular disease (PAD) (ROTTERDAM, ACAPS trials ) [Lorenz, 2007]
- thickening of IMT correlates with the presence of traditional vascular risk factors (high BMI, hypertension, hypercholesterolemia, diabetes, smoking)
- some authors recommend including both IMT and the presence of atherosclerotic plaquess among the classic vascular risk factors [Chambless, 2010]
- some publications question significance of IMT in predicting cardiovascular events [Costanzo, 2010] [Ruijter, 2012]
- detection of subclinical atherosclerosis is important in patients with borderline risk and multiple risk factors, as it shifts the patient into the high-risk category (SCORE ≥ 5%) with all therapeutic consequences
- pharmacological studies have shown a reduction in the rate of progression of IMT with hypolipidemic therapy and antihypertensive drugs (ACAPS, METEOR)
- on the other hand, a meta-analysis of 41 randomized trials showed regression of cardiovascular events with hypolipidemic drugs but did not show a relationship between a decrease in CV events and a regression of IMT [Costanzo, 2010]
- an enlarged arterial wall can also be found in non-atherosclerotic diseases (e.g., Takayasu arteritis)