ISCHEMIC STROKE / CLASSIFICATION AND ETIOPATHOGENSIS
Radiation-induced vasculopathy
Updated on 07/06/2024, published on 14/02/2022
Patients after head and neck radiotherapy should be regularly monitored with ultrasound to detect carotid steno-occlusive disease
- radiation therapy (RT) plays an important role in managing both primary and metastatic tumors
- structures such as the brain, cranial nerves, spinal cord, and brain and heart vessels may be adversely affected by RT
- radiation-induced vasculopathy (angiopathy) is a heterogeneous and poorly defined complex of vascular injuries attributable to radiation exposure
- both small and large vessels may be affected, manifesting as extracranial carotid stenosis, intracranial stenosis, and other vascular anomalies (e.g., cavernous malformations, aneurysms, moya-moya syndrome, etc.)
- vasculopathy is not limited to cerebral arteries, premature coronary artery disease (CAD) usually involves the ostium or proximal coronary arteries
- total dose, duration of exposure, and tissue type exposed are factors influencing the development and severity of vasculopathy
- vasculopathy carries an increased risk of cardiovascular complications in the decades following the initial RT
- occlusive vasculopathy may manifest years after initial RT (2-25 y) with an increased incidence due to improved oncological treatment and extended patient survival rates
- early identification of radiation vasculopathy is critical for initiating early therapeutic interventions
- occlusive vasculopathy may manifest years after initial RT (2-25 y) with an increased incidence due to improved oncological treatment and extended patient survival rates
- radiation-induced vasculopathy is also associated with an increased risk of autonomous dysregulation (baroreceptor failure) (Sharabi, 2003)
Etiopathogenesis
Vascular injury
- acute radiation exposure leads to impaired blood-brain barrier (BBB) integrity ⇒ vasogenic edema occurs
- the late vascular complications are primarily attributed to endothelial damage within the vascular system, manifesting as:
- telangiectasia
- aneurysm formation
- microangiopathy leading to impaired blood flow and tissue damage
- atherosclerosis affecting medium to large vessels
- significant carotid vasculopathy (as a late complication of radiotherapy) is predominantly observed following radiotherapy in the ear, nose, and throat (ENT) regions
Glial and white matter injury
- oligodendrocytes are more susceptible to radiation-induced damage compared to relatively resistant neurons
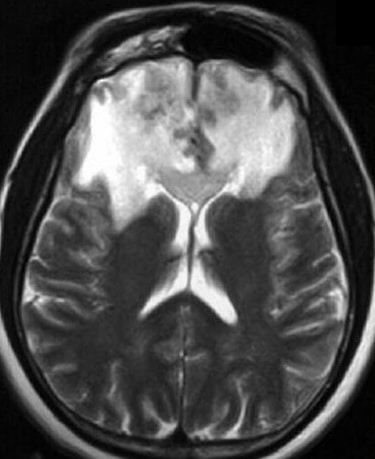
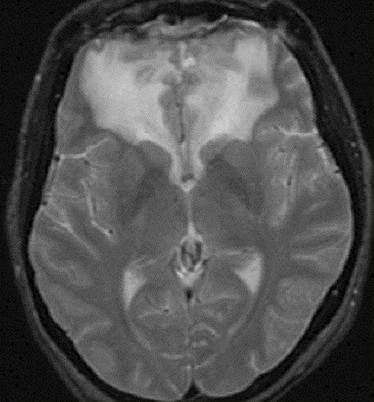
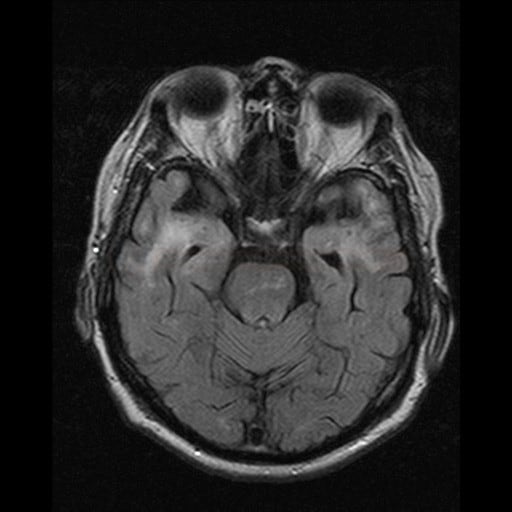
- MRI shows brain atrophy and extensive leukoencephalopathy
Classification
| Classification of post-radiation CNS injuries |
| Acute (< 14 days after radiation therapy) |
|
|
Early delayed (> 2 weeks to several months)
|
|
| Late (months to years) |
|
Diagnostic evaluation
Imaging findings of radiation vasculopathy exhibit a predictable location and time course. Acute injury occurs within several weeks of treatment, early delayed injury within several weeks to months, and late injury emerges months to years post-treatment
CT/MRI of the brain
- specific finding: extensive leukoencephalopathy
- CT – white matter hypodensities, vasogenic edema
- T2/FLAIR – often symmetric hyperintense lesions
- hypointense lesions suggest vascular anomalies (e.g., cavernous malformations or telangiectasias)
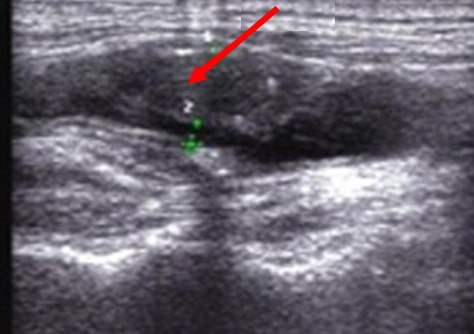
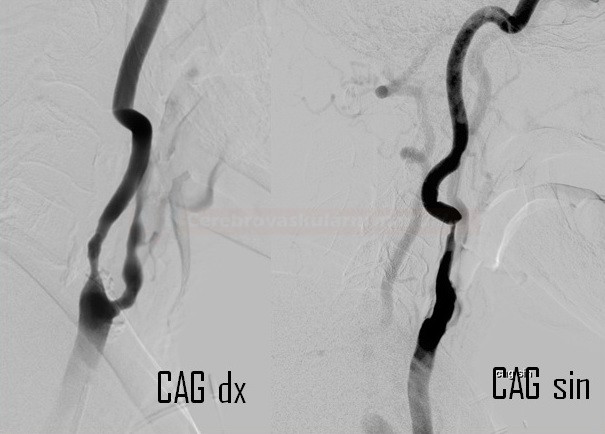
Neurosonology
- significant bilateral common carotid artery (CCA) involvement is common
- especially after radiotherapy in the ENT region
- especially after radiotherapy in the ENT region
- radiation-induced stenoses tend to be severe and involve longer segments than the traditional atherosclerotic disease
- non-calcified plaques with hypoechoic foci predominate in B-mode [Lam, 2012]
CT/MR angiography
- vascular imaging studies identify the above-stated vascular changes extra-/intracranially
- pathognomic is the focal presence of stenoses predominantly in the irradiated area and the absence of pathology in other segments
- MRA/CTA/DSA may help to identify radiation-induced aneurysms or moyamoya revascularization patterns
Management
- antiplatelet therapy
- in case of cancer-related thrombosis, LWHMs or DOACs are prescribed
- vascular risk factors modification
- statins – play a role in reducing vascular inflammation and stabilizing plaques
- blood pressure monitoring and aggressive treatment of hypertension
- smoking cessation
- statins – play a role in reducing vascular inflammation and stabilizing plaques
- follow-up is essential to detect premature carotid artery stenosis and CAD
- consider CEA or CAS if significant stenosis is identified
- vascular anatomy, surgical risk factors, and the patient’s prognosis must be taken into account
- both options share good short-term outcomes and similar perioperative complication rates; CEA probably offers more durable vessel patency
- CABG can be challenging in the presence of heavily calcified or friable internal mammary arteries
- both open and endovascular treatment of intracranial radiation-induced aneurysms have been reported