NEUROIMAGING
Carotid artery occlusion
Updated on 24/06/2024, published on 12/04/2024
Carotid artery occlusion typically results from atherosclerotic disease (with thrombosis), dissection, or embolism. The clinical significance depends on the location of the occlusion, the acuteness of the event, and the presence of collateral blood flow.
Thus, it is important to evaluate the patient clinically and with imaging methods to answer these questions:
- is the occlusion acute or chronic?
- acute occlusion is most commonly symptomatic, and stroke severity depends on collateral circulation, location of the occlusion, and concurrent vascular pathology)
- chronic occlusion is usually asymptomatic but is associated with an increased risk of stroke in future years
- ICA occlusion is associated with a 2-year stroke risk of about 10-15%; the risk is higher in the presence of impaired vasomotor reactivity (VMR)
- which segment is occluded?
- establishing the occlusion site is important for planning mechanical thrombectomy
- it is essential to differentiate between extracranial and intracranial ICA occlusion, as well as the detection of an underlying lesion which could require angioplasty ± stenting
- in almost 50% of intracranial ICA occlusions, cervical ICA is non-opacified on CTA
- it is caused by blunted flow and can simulate an extracranial occlusion (pseudo-occlusion)
- the thrombus, in such cases, extends below the origin of OA (affecting anterior choroidea, posterior communicating, and ophthalmic arteries)
- is there concurrent distal intracranial occlusion?
Clinical presentation
- acute carotid occlusion – symptoms usually present suddenly and are severe
- chronic carotid occlusion – may be asymptomatic due to the development of collateral circulation; if symptoms occur, they are often less severe and have a gradual onset
- extra- and intracranial occlusion can not be reliably distinguished clinically; intracranial occlusion is almost always symptomatic, while isolated extracranial occlusion may remain asymptomatic
Imaging methods
Neurosonology
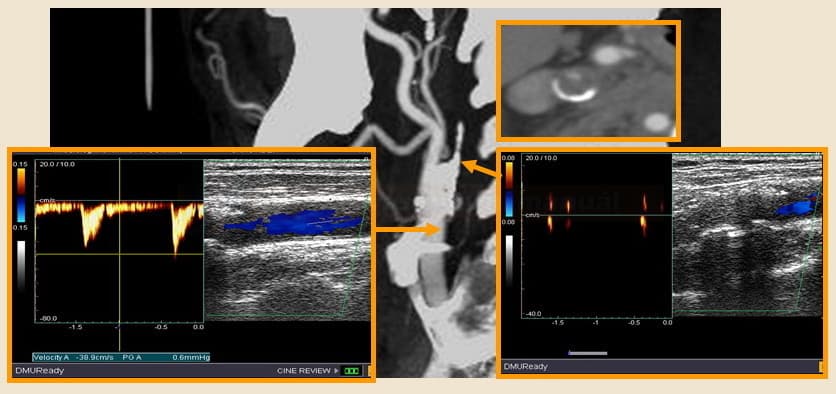
Detection of an occluded segment
-
- in pseudo-occlusion, the origin of ICA shows systolic peaks, and the lumen is hypoechoic (dark)
- pseudo-occlusion is difficult to differentiate from acute ICA thrombosis with fresh intraluminal hypoechoic thrombotic masses
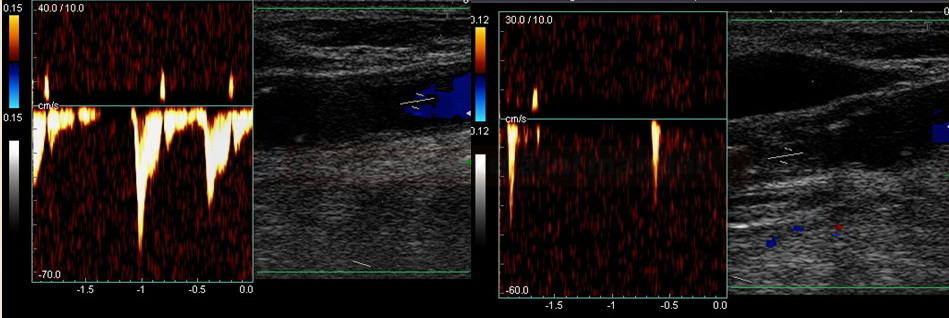
Differentiation of acute and chronic ICA occlusion
- ultrasound is useful for diagnosing acute ICA occlusion [Herzig, 2011]
- B mode:
- chronic occlusion – the lumen is filled with heterogeneous atherosclerotic masses and is retracted and poorly visualized in distal segments
- acute occlusion – lumen is hypoechoic (filled with fresh dark thrombus)
- difficulties arise in patients with preexisting severe stenosis when a fresh thrombus occludes the remaining free lumen
- similar Doppler finding can be seen with terminal ICA occlusion, where stagnant blood fills the proximal ICA, mimicking occlusion at the vessel’s origin
- color mode: no color is visible in the arterial lumen
- Doppler:
| Acute occlusion | Chronic occlusion |
| anechoic lumen | heterogeneous AS masses |
| symmetric ICA lumen width | ICA lumen is retracted, gradually disappearing distally |
| lack of collaterals | fully developed collateral circulation |
| markedly reduced flow in the ipsilateral MCA | typically only mildly reduced flow in the MCA with slowed systolic acceleration (depending on the quality of the collateral circulation) |
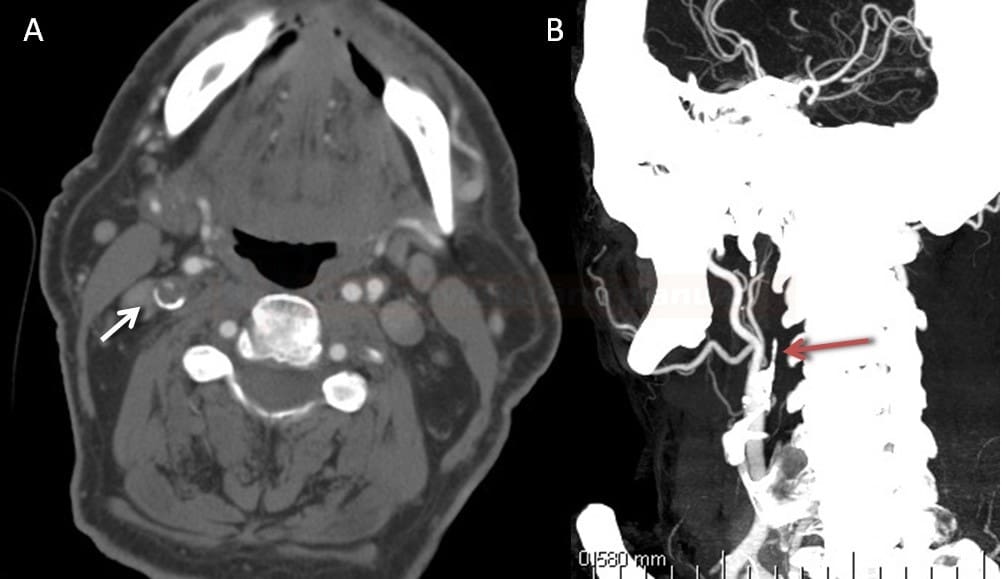
CT or MR angiography
- if the entire ICA is not visible on CTA/MRA, consider the following scenarios:
- thrombosis of the entire ICA (or even CCA) versus terminal ICA occlusion (thrombus reaches bellow OA ostium) with stagnation of contrast agent proximally (the situation is often clarified on DSA during embolectomy)
- isolated intracranial ICA occlusion (reaching OA, PComA, and AChA) can mimic extracranial affection (extracranial pseudo-occlusion) (Fernandez-Gomez, 2023)
- delayed filling sign on mCTA could be a useful and readily available finding for differentiating proximal ICA pseudo-occlusion from true occlusion (Choi, 2020)
- occlusion of the proximal ICA due to atherothrombosis combined with distal occlusion (typically uneven and calcified contour of the artery stump is found)
- occlusion due to dissection (younger patient, string sign, absence of atherosclerotic changes in other arteries)
- thrombosis of the entire ICA (or even CCA) versus terminal ICA occlusion (thrombus reaches bellow OA ostium) with stagnation of contrast agent proximally (the situation is often clarified on DSA during embolectomy)
- differentiation of acute vs. chronic occlusion
- acute occlusions may show a fresh thrombus with an abrupt cutoff
- carotid ring sign can be found in the acute total occlusion (intraluminal hypodense thrombus and/or the ring enhancement of the vasa vasorum in the arterial wall (Michel, 2011) (Yi, 2024)
- mCTA may show pseudo-occlusion which is usually caused by acute occlusion of distal ACI
- well-defined collateral pathways are typical for chronic occlusion
- challenging is acute occlusion in the terrain of chronic severe carotid stenosis
Digital subtraction angiography
- during mechanical thrombectomy, the occluded segment is reliably verified (best for detection of pseudo-occlusion)