ISCHEMIC STROKE / CLASSIFICATION AND ETIOLOGY
Thromboangiitis obliterans (Buerger´s disease)
Updated on 29/01/2024, published on 10/05/2023
Definition
- Buerger’s disease (also known as thromboangiitis obliterans) is a nonatherosclerotic, segmental inflammatory disease that most commonly affects small and medium-sized arteries and veins of the upper and lower extremities
- cerebrovascular involvement is rare but has been reported
- the disease predominantly affects young men under 45 years of age who are heavy smokers or chew tobacco (the prevalence among female smokers is low)
- the average age for the onset of symptoms is around 35 years
- the average age for the onset of symptoms is around 35 years
- inflammation leads to arterial stenosis and potential thrombosis, causing pain, tissue damage, and even gangrene (in severe cases, amputation may be required)
- quitting smoking is the most important step in preventing and managing the disease
Etiopathogenesis
- the exact cause and pathogenesis remain unclear
- there is strong evidence indicating that smoking is a major contributor
- an inflammatory process with granulomas occurs in peripheral small and medium-sized arteries and veins
- elevated pro- and anti-inflammatory cytokines and various kinds of autoantibodies have been identified in patients with TAO (Kaiser, 2021)
- this extensive stenotic process and thrombosis lead to limb ischemia
Clinical presentation
- fingers and toes are pale or bluish and feel cold to the touch; progressive necrosis may occur
- pain in hands or feet at rest
- pain may feel like a burning or tingling sensation
- pain may worsen when the hands and feet get cold or during emotional stress or exercise
- intermittent claudication – pain in the legs, ankles, or feet (arch of the foot) when walking
- skin changes, incl. small painful sores on the fingers or toes; gangrene may occur in severe cases
- although CNS symptoms (including stroke) have been sporadically reported, they are not common (Kaiser, 2021)
Diagnostic evaluation
Diagnosis is based on typical clinical presentation, vascular imaging, and patient characteristics (age, smoking history)
Blood tests
- there is no specific blood test to diagnose thromboangiitis obliterans
- it is necessary to exclude other vasculitides
Biopsy
- in rare cases, a biopsy may be performed
- the gold standard to establish a definitive diagnosis
- acute phase histology of the affected superficial vein shows a hypercellular, inflammatory thrombus with less pronounced inflammatory changes in the vessel wall
Vascular imaging
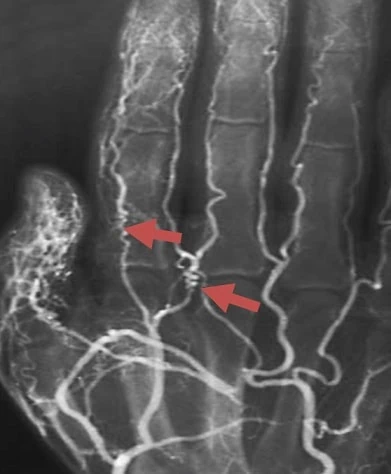
- ultrasound, CTA, MRA, or DSA may be used
- multilimb involvement with a predilection for the lower extremities
- typical extensive obliteration of small and medium-sized vessels + thin corkscrew-like collaterals
- normal findings in proximal arterial segments without atherosclerotic changes
| Positive points | ||
| Age at onset |
<30 | +2 |
| 30-40 | +1 | |
| Foot intermittent claudications |
present | +2 |
| by history | +1 | |
| Upper extremity |
symptomatic | +2 |
| asymptomatic | +1 | |
| Migrating superficial venous thrombosis (SVT) |
present | +2 |
| by history | +1 | |
| Raynaud color changes |
present | +2 |
| by history | +1 | |
| Angiography | typical | +1 |
| Biopsy | typical | +1 |
| Negative points | ||
| Age at onset |
45-50 | -1 |
| > 50 | -2 | |
| Sex, smoking |
female | -1 |
| non-smoker | -2 | |
| Location |
single limb |
-1 |
| no lower extremities involved |
-2 | |
| Absent pulse |
brachial | -1 |
| femoral | -2 | |
| Vascular risk factors (diabetes, HT, etc.) |
discovered after diagnosis 5-10 years | -1 |
| 2-5 years | -2 | |
| Points | probability of diagnosis |
| 0-1 | diagnosis excluded |
| 2-3 | suspected, low probability |
| 4-5 | probable, medium probability |
| ≥ 6 |
definite, high probability |
Management
- no evidence-based causal therapy; the only effective measure to prevent the worsening of Buerger’s disease is to stop smoking → smoking cessation
- no significant effect of antiplatelet, anticoagulant, or steroid therapy has been demonstrated
- avoid cold temperatures and other conditions that reduce blood flow to the limbs
- treat infections promptly, use anti-inflammatory drugs for phlebitis, or consider vasodilators
- the efficacy of immunoadsorption is under discussion
- revascularization options are limited; sympathectomy may be considered in certain cases
- amputation is necessary if gangrene develops