ISCHEMIC STROKE
Stroke mimics
Updated on 24/06/2024, published on 24/05/2023
- stroke is a medical emergency presenting with focal neurological deficits; stroke mimics are non-vascular conditions that present with symptoms similar to those of stroke
- incidence of stroke mimics is ~3-10% [Okano, 2018] [Winkler, 2009] [Scott, 2003] [Tsivgoulis, 2011]
- the most common mimics are epileptic seizures, migraine, brain tumors, functional disorders, TGA, hypoglycemia and other metabolic disorders, syncope, or intoxication
- the existence of mimics causes troubles in the acute setting (should we initiate thrombolysis?) but also in the chronic stage (is it a recurrent stroke? should we change the secondary prevention? is CEA indicated for carotid stenosis?)
- incorrectly administered IVT may harm the patient, although available data show the relative safety of thrombolysis in stroke mimics [Tsivgoulis, 2011]
- on the other hand, failure to adequately treat unrecognized stroke reduces chances for recovery
- it is essential to consider stroke mimics in the differential diagnosis of every patient with suspected stroke; however, potential candidates for thrombolytic therapy should not be excluded based on the sole concern that their neurological symptoms may be due to stroke mimics
| Characteristic | Probable stroke | Probable mimics |
| age and sex | older age (male = female) | younger age (females > males) |
| level of consciousness | usually awake at the onset (except for extensive vertebrobasilar occlusion) |
altered level of consciousness |
| onset and progress | acute and sudden | gradual |
| symptoms severity | severe at onset | fluctuations are common, usually milder deficit |
| risk factors | vascular risk factors | history of migraine, seizure, systemic illness, cognitive impairment |
| vascular territory | vascular syndromes | symptoms not corresponding to a single vascular territory |
| blood pressure at presentation | increase blood pressure is common | blood pressure usually not increased |
| signs and symptoms | focal deficit (limb paresis, gaze deviation, aphasia, or visual field defects) |
sensory symptoms, vertigo, and visual symptoms, often an absence of focal neurologic signs |
| involuntary movements | uncommon | may be present |
| imaging |
ischemic lesion or vessel occlusion, perfusion mismatch on CTP or MRI (dense sign on NCCT, occlusion on CTA) |
lesions not respecting the vascular territories |
| EEG | EEG may show slowing over the affected area | spikes and waves in seizures, PLEDS |
Recrudescence |
- recurrence of previous stroke-related deficits in the settings of metabolic, infectious, and toxic dysfunction
- may develop within weeks to years after the previous stroke
- DWI excludes new stroke
- symptoms are usually short-lived, resolving within 24 hours in most individuals
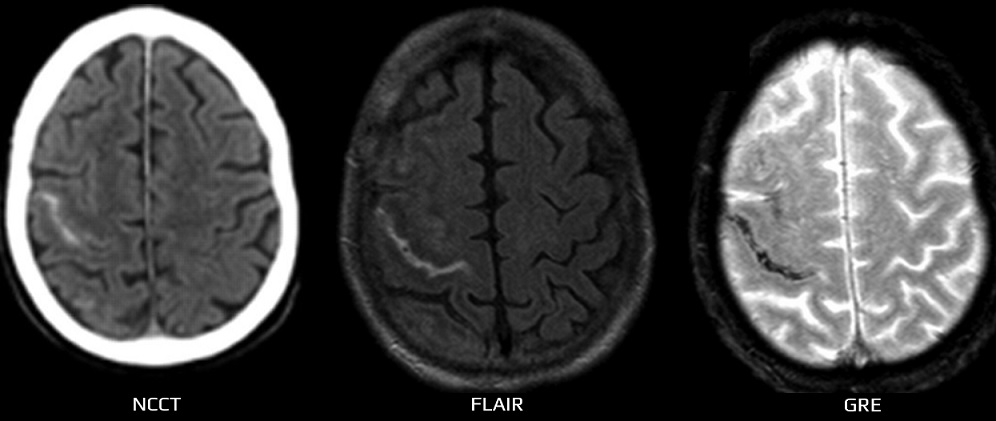
Nontraumatic convexal (focal) SAH |
- a rare cause of transient symptoms
- more common in older patients (> 60 years) [Beitzke, 2011]
- MRI confirms the diagnosis (with almost 100% sensitivity); thin-sliced multiplanar CT is also a valuable emergency diagnostic tool (however, MRI remains crucial and mandatorily and must be completed within the next 24–72 hours) [Ertl, 2014]
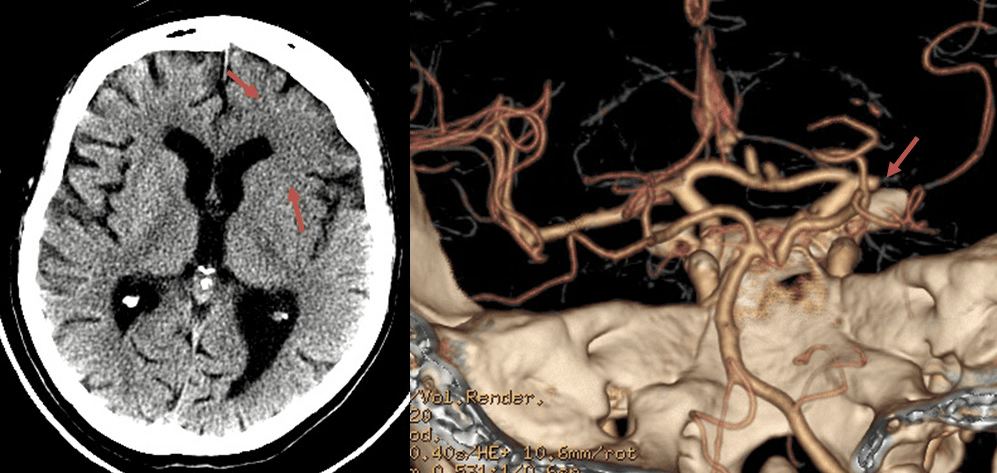
Transient symptoms in CAA (amyloid spells)
|
- amyloid spells in CCA represent a stroke mimic associated with ↑risk of ICH after IVT administration → Cerebral amyloid angiopathy (CAA)
Stroke-like episodes in Sturge-Weber syndrome
|
Epileptic seizure
|
- epileptic seizure may mimic a stroke, and the patient may be mistakenly treated with thrombolysis
- conditions such as Todd’s hemiparesis, complex focal seizures mimicking symbolic dysfunction, etc., are challenging in the acute stage
- epileptic seizures can also occur in the terrain of previous ischemia (poststroke epilepsy) and transiently worsen the previous deficit
- conditions such as Todd’s hemiparesis, complex focal seizures mimicking symbolic dysfunction, etc., are challenging in the acute stage
- however, epileptic seizures can also occur during an acute stroke (~1-6%), and the patient may not receive appropriate recanalization therapy if misdiagnosed as a pure seizure [Sylaja, 2006] [Killpatrick, 1990]
- thrombolytic therapy is not contraindicated for a stroke patient experiencing an epileptic seizure as long as imaging confirms the stroke (occlusion on CTA, perfusion mismatch, fresh DWI lesion, etc.)
Clinical presentation
- symptoms indicative of a seizure → classification of seizures
- focal seizures
- isolated positive motor or sensory symptoms (FAS)
- altered awareness (FIAS)
- gradual spread (march)
- uniform attacks
- sometimes a therapeutic test with AE can be helpful in establishing the correct diagnosis
- generalized seizures
- motor (tonic-clonic convulsions or others) or non-motor components (absence)
- postictal confusion
- lost bladder control
- tongue and/or cheek injury
- focal seizures
- objective history
- a typical course of seizure, and a history of similar seizures in the past
- in general, any initial transient disturbance of consciousness should raise suspicion of another etiology
Diagnostic evaluation
- in unclear cases, imaging methods can help:
- demonstration of arterial occlusion on CTA
- demonstration of early ischemia on CT (ASPECTS)
- demonstration of fresh ischemia on DWI with the corresponding hypointensity in the ADC map
- positive CT perfusion
- prolactin may already be normal on arrival at the hospital (peak around 30 minutes), and the result is not available acutely
Migraine |
- a frequent stroke mimic
- migraine aura without the headache and the first attack of basilar or hemiplegic migraine represent the main problems
- symptoms usually develop more slowly, spread or migrate, and are typically followed by headache with nausea/vomiting and photo-/phonophobia (see table)
- migraine is likely:
- in younger patients with a history of similar recurrent attacks and no vascular risk factors
- with positive symptoms developing within minutes or tens of minutes (gradual onset)
- flashes, bright lines, and scintillations that begin in part or half of the visual field and may extend to the entire visual field or often move across the visual field
- paresthesias usually spreading or moving over half the body (march), including the head, over minutes to tens of minutes
- with subsequent development of headache
- history of repeated uniform attacks with a slow onset may be helpful
- if symptoms resolve rapidly, DDx of TIA can be problematic (mainly if the condition occurs for the first time)
- imaging, including MR-DWI or CT perfusion, is normal
- dissection should be ruled out in new-onset hemicrania with focal findings!
Migraine characteristics (must meet at least 2 of the following):
|
| TIA | Migraine aura | |
| personal history |
usually no history of a similar attack |
repeated attacks |
| symptoms onset |
sudden (seconds) | gradual (> 5 min) |
| duration | mostly minutes |
approx. 20-30 min (< 60 min) |
| timing | focal symptoms with concurrent headache | focal symptoms precede the headache |
| visual disorders |
monocular disorders hemianopia |
positive scintillating scotomas, gradually spreading across the entire visual field
negative scotomas |
| headache | migraine headache criteria see above headache most commonly follows focal symptoms but may be absent |
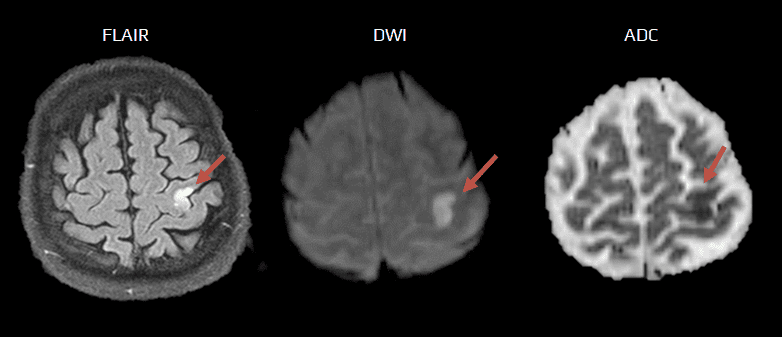
Stroke-like migraine attacks after radiation therapy (SMART) syndrome |
- SMART syndrome (stroke-like migraine attacks after radiation therapy) is a delayed complication of brain radiotherapy (usually associated with doses of ≥50 Gy)
- onset of symptoms varies widely from 1 to 40 years after initial radiation therapy
- symptoms last from several hours to several weeks and typically consist of:
- recurrent headaches with migraine-like aura
- seizures
- stroke-like symptoms referable to a unilateral cortical region (motor deficits, paresthesias, aphasia, and visual disturbances)
- full recovery in most patients has been reported
- imaging findings may include unilateral increased T2 signal with associated gyral thickening and transient cortical enhancement in the temporal, parietal, and occipital lobes; the process spares the white matter
- the pathogenesis is not as well understood as other complications of radiation, such as leukoencephalopathy and radiation necrosis
- proposed endothelial dysfunction may lead to disruption of the blood-brain barrier with subsequent marked cortical enhancement
- some case reports have described nonspecific gliosis without inflammation or no identifiable histopathologic abnormalities
Metabolic and toxic encephalopathies |
- mental status changes and epileptic seizures with possible Todd’s hemiparesis predominate in most encephalopathies (renal, hepatic failure)
- impaired level of consciousness may progress
- complications may occur even after hemodialysis (see below)
- neuroglycopenia and Wernicke encephalopathy, in particular, may present with focal symptoms, which are the most difficult to differentiate from a true stroke
Hypertensive encephalopathy |
- may accompany decompensated hypertension (usually with SBP > 220 mmHg/DBP > 120 mmHg) → hypertensive crisis
- the rate of BP increase seems to be more important than its absolute value
- failure of autoregulation leads to cerebral edema
- clinical presentation:
- confusion, headache, nausea/vomiting, visual disturbances, focal symptoms
- papilledema and hypertonic retinopathy on ophthalmoscopy
- reversible posterior hypertensive encephalopathy (PRES) may occur
Multiple sclerosis
|
- DDx of a first attack of multiple sclerosis (MS) from a stroke and recognition of the coincidence of MS and acute stroke may pose problems
- the most difficult decision is whether to administer IVT or not
- age and the presence or absence of risk factors cannot be relied upon (stroke is increasingly seen in young patients without vascular risk factors)
- in addition, MS can manifest at older ages (40-50 years) when patients may already have multiple vascular risk factors present
- the most difficult decision is whether to administer IVT or not
- findings of occlusion on CTA, perfusion defects on CTP, or early signs of ischemia (ASPECTS<10) are helpful
- MR DWI
- acute plaque may present with diffusion restriction on DWI ⇒ small lesions cannot be reliably distinguished radiologically from lacunar infarct (Davoudi, 2016)
- postcontrast enhancement of the lesion may help
- larger ischemic lesions can be distinguished by their typical shape and location corresponding to an arterial territory
- acute plaque may present with diffusion restriction on DWI ⇒ small lesions cannot be reliably distinguished radiologically from lacunar infarct (Davoudi, 2016)
Peripheral vestibular syndromes |
- typical association with position change
- dizziness and nystagmus can be provoked by specific positional tests (Dix-Hallpike, Seemont, Log-roll, etc.)
- an acute vestibular syndrome characterized by sudden-onset severe vertigo, nausea, vomiting, and gait instability, without auditory symptoms
- it results from inflammation of the vestibular nerve, often due to viral infection
- diagnosis is clinical, supported by head impulse tests and the absence of central neurological signs
- management includes corticosteroids, antiemetics, and vestibular rehabilitation
- recovery is typically gradual over weeks to months, with most patients experiencing significant improvement
- Ménière’s disease is an inner ear disorder causing vertigo, tinnitus, hearing loss, and aural fullness
- it results from endolymphatic hydrops
- diagnosis is clinical, supported by audiometry and vestibular testing
- management includes lifestyle modifications, medications, and, in refractory cases, surgical interventions
- acetazolamide, hydrochlorothiazide, bethistine
- vestibular paroxysmia is a vestibular disorder characterized by brief, recurrent episodes of vertigo lasting seconds to minutes, often triggered by head movements
- auditory symptoms like tinnitus or hearing loss may occur
- it results from vascular compression of the 8th cranial nerve
- diagnosis involves clinical evaluation, MRI, and response to carbamazepine/oxcarbazepine
- initial dose: 100-200 mg twice daily, then increase gradually based on patient response and tolerability
- maintenance dose: typically 400-1200 mg daily, divided into two or three doses
- microvascular decompression is considered in refractory cases
Transient global amnesia (TGA) |
- a sudden, temporary (< 24h) episode of memory loss in the absence of other neurological signs and symptoms
- memory loss cannot be attributed to a more common neurological condition, such as epilepsy or stroke → more here
Tetany
|
- tetany is usually manifested by involuntary muscle cramps due to electrolyte abnormalities (most commonly hypocalcemia)
- diagnostic difficulties can be caused by isolated paresthesia
Brain disorders with structural lesions |
- these disorders can be differentiated by neuroimaging (CT/MRI)
- intracerebral or spinal hemorrhage
- differentiate hemorrhagic infarction (arterial and venous)
- differentiate hemorrhagic infarction (arterial and venous)
- tumor – acute deterioration may be caused by bleeding into the tumor due to decompensation of edema or epileptic seizure
- neuroinfectious diseases
- fever, headache, elevation of inflammatory markers, mental status changes, epileptic seizures
- autoimmune encephalopathy
- gradual onset
- typical MRI presentation with temporal lobe predilection
- abnormal EEG
- autoantibodies (not available in the acute phase)
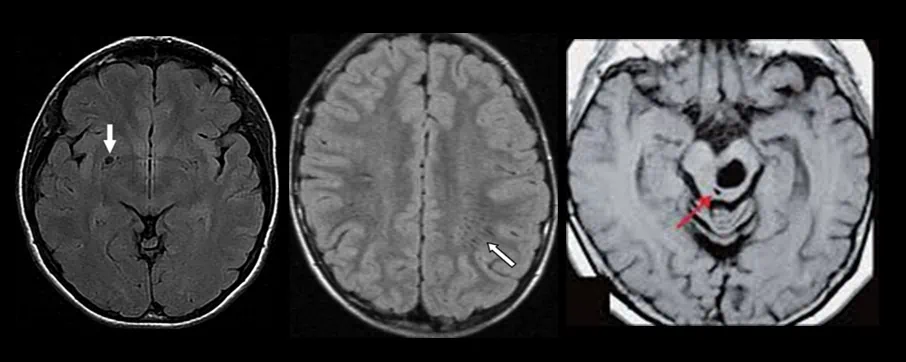
- PRES (Posterior Reversible Encephalopathy Syndrome)
- a neurological condition characterized by reversible subcortical vasogenic edema predominantly affecting the posterior regions of the brain
- no reaction in surrounding tissue, the lesion is hypointense on FLAIR (contains cerebrospinal fluid), DWI/ADC, and GRE are negative
- mostly asymptomatic; isolated cases with hydrocephalus, blepharospasm, etc., have been reported
- typical localizations:
- basal ganglia
- at the convexity
- mesencephalon-pons junction
- history of trauma is unreliable or negative in up to 50% of cases; there may be no external signs of injury
- in addition, it is often unclear whether the patient fell due to hemiparesis induced by the stroke or whether the stroke was caused by the fall (e.g., due to dissection, arterial rupture, etc.)
- if trauma is suspected, search for:
- don’t miss chronic SDH as it is isodense on CT in 1-3 weeks (look for signs of edema, add MRI if in doubt)
- traumatic changes (contusions):
- do not correlate with vascular territories
- are typically located in the temporal and frontobasal regions of the brain
- often have a hemorrhagic component and edema and may be associated with mild SAH
Psychosomatic disorders
|
- first episode of conversion disorder with a focal deficit (paresis, etc.) pose the biggest problem; the situation is easier with anxiety disorders
- a simplified classification can be made:
- panic attacks, anxiety
- conversion somatomorphic disorders
- simulation
- in the first attack, an organic cause must always be carefully excluded (negative imaging, incl. DWI)
- what to do during the clinical examination:
- assess the signs while distracting the patient’s attention (fluctuations in paresis severity can be observed)
- objectify the findings using EMG, EP, brain imaging
- look for discrepancies and fluctuations in motor impairment (e.g., rapid fall in Minagazzini in a walking patient, seeing a paretic patient walking in a hospital park, etc.)
- investigate the exact borders of hemihypesthesia (in psychosomatic disorders, the border is usually in the midline)
- search for the provoking moment and the potential benefit of the current condition (partner’s interest, financial motivation, etc.)
- note emotional inertia to severe deficits (e.g., a smiling patient who has suddenly “gone blind”)
- exclude rare Anton (denies blindness) and inverse Anton syndrome (patient sees but thinks he is blind)!
- look for psychiatric history
- clinical presentation
- in somatomorphic disorder or simulation, impaired mobility of one or more limbs, impaired hearing or blindness, and bizarre gait are not uncommon
- there is a long history of difficulties, repeated hospitalizations in different departments with negative findings
- vivid depiction of polymorphic difficulties, extensive documentation, keeping a diary of difficulties, etc.
- absence of pyramidal signs and atrophy of paretic limb, etc.
- purposeful, deliberate action for specific gain (e.g., compensation, pension, etc.)
- disorders in which physical symptoms are present without an obvious organic cause, have a presumed psychogenic cause and are not consciously produced or simulated
- mechanisms:
- reactivation of past emotions by a relatively recent provoking stressor
- reactions to a serious current trauma (e.g., rape, recent history of physical or psychological abuse)
- chronic suppression of anger followed by a series of frustrations in adulthood
- panic disorder with or without agoraphobia
- acute stress disorder
- post-traumatic stress disorder
- often accompanied by hyperventilation, strong feelings of fear (must be actively questioned), shortness of breath, palpitations
- the typical triggering factor usually occurs
- attacks tend to be uniform (typically paresthesias and dysesthesias, but there may also be motor manifestations)
- a trial with anxiolytics can be performed
Peripheral neurogenic lesions |
- usually can be distinguished by history, typical areal distribution of sensory and motor impairment, and usually present with pain
- a detailed neurological examination should distinguish peripheral from central symptoms
- small pre- or postcentral infarcts can be problematic, causing isolated motor or mixed deficits involving only specific muscle groups (e.g., cortical hand syndrome)
- may cause a problem in cases of sudden onset, e.g. due to infection or drugs, and with asymmetric presentation
- in particular, sudden onset of bulbar involvement with diplopia may raise suspicion of a vascular etiology, but if bilateral ptosis is present, it is more likely to be a manifestation of myasthenia gravis
- in the event of an acute diagnostic emergency, the effect of injectable neostigmine can be tested