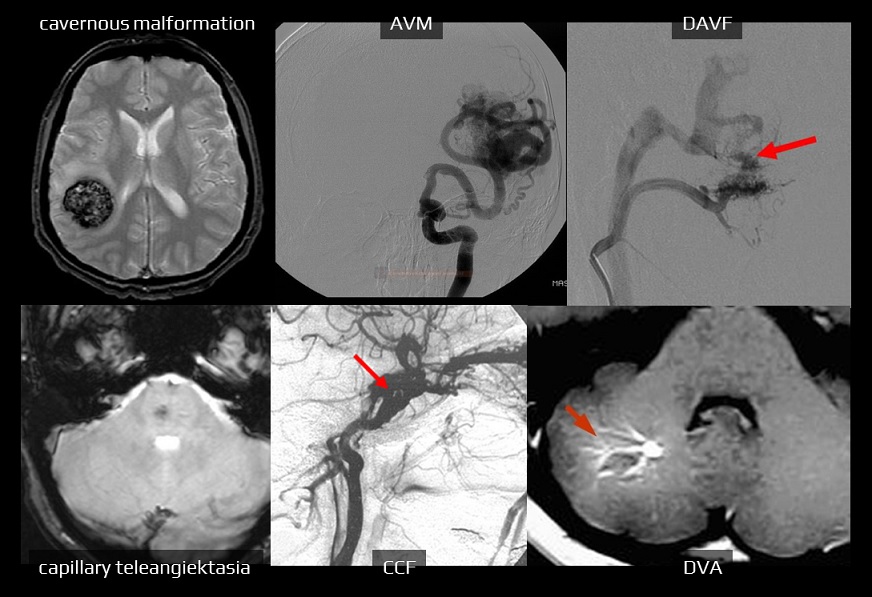
INTRACEREBRAL HEMORRHAGE / VASCULAR MALFORMATIONS
Cerebral cavernous malformation
Updated on 01/09/2024, published on 20/06/2023
Definiton
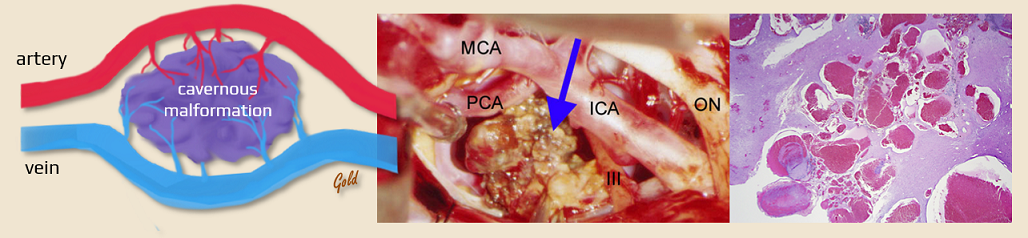
- cerebral cavernous malformation (CCM) is a well-circumscribed accumulation of dilated, thin-walled vessels that affect the brain
- only a layer of endothelium and subendothelial stroma is present; smooth muscle cells and elastic fibers are absent
- the pathogenesis of CM remains unclear
- only a layer of endothelium and subendothelial stroma is present; smooth muscle cells and elastic fibers are absent
- forms:
- sporadic
- incidence in the population 0.4-0.9% [Sage, 1993]
- accounts for 8-15% of all vascular malformations
- usually one lesion (in about 70% of cases)
- familial
- sporadic
- can be localized anywhere (approximately 80% are supratentorial)
- CM-associated anomalies:
- Café au lait spots
- DVA (developmental venous angioma)
| MRI | 0.25-0.7% rebleeding 4.5% |
|
| MRI, DSA | 0.2-0.4% | |
| DSA, CTA | 2-4 % rebleeding 6-18% |
|
| MRI | very low |
|
| DSA, MRA, CTA |
type I – very low
type II, III – up to 8%
|
|
| Carotido-cavernous fistula (CCF) | DSA, MRA | very low |
- familial cases of CCM have autosomal dominant (AD) inheritance with incomplete penetrance
- account for 10–50% of all cases
- mutations have been identified in three genes:
- KRIT1 (Krev interaction trapped 1) on 7q21-q22 (CCM1)
- MGC4067 (Malcavernin) on 7p13 (CCM2)
- PDCD10 (programmed cell death 10) on 3q26-q27 (CCM3)
- genotype–phenotype correlations between the three forms are emerging
- CCM1 mutation carriers appear to have a milder hemorrhage phenotype but may present with more seizures and extraneurologic manifestations
- CCM3 patients may have a more aggressive clinical course with an earlier age of onset of symptoms and greater risk of ICH
Pathophysiology
- erythrocyte diapedesis through the pathological cavernoma wall
- hemoglobin degradation products induce pathological excitability, oxidative damage, and gliosis, leading to epilepsy
- hemoglobin degradation products induce pathological excitability, oxidative damage, and gliosis, leading to epilepsy
- bleeding into the cavernoma ⇒ ↑ malformation volume
- bleeding into the surrounding area
Clinical presentation
- asymptomatic in up to 44% of cases
- epileptic seizures (45-70%) [Májovský, 2014] [Sage, 1993]
- mostly associated with lesions localized in the frontal and temporal lobes
- cavernous malformations account for approximately 4% of refractory epilepsy
- bleeding
- low risk (0.25-0.7% per year), increased after prior bleeding episodes (⇒ 4.5% / year)
- higher risk with infratentorial lesions
- hemorrhages are generally non-fatal due to low pressure within the malformation; however, repeated hemorrhages may ultimately lead to severe neurological deficit
- headache (20-30%)
- focal neurological deficit (e.g., in case of cerebellar or brainstem lesion)
- risk factors for adverse outcome
- multiple lesions
- presence of CCM3 genotype
- early clinical presentation
- infratentorial localization
- lesion diameter >1 cm
- associated developmental venous anomaly (DVA)
Diagnostic evaluation
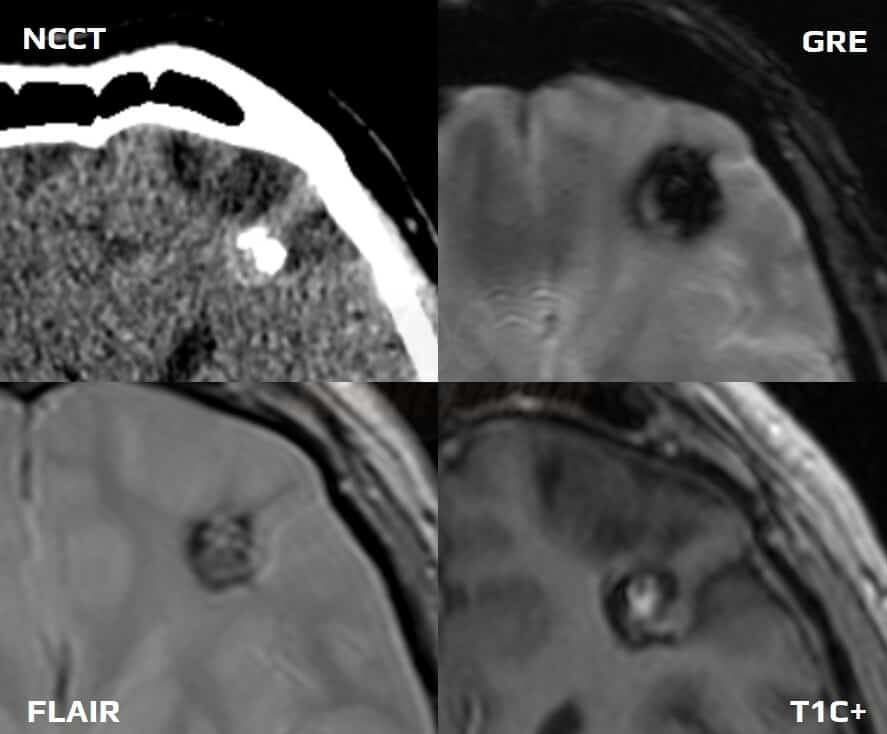
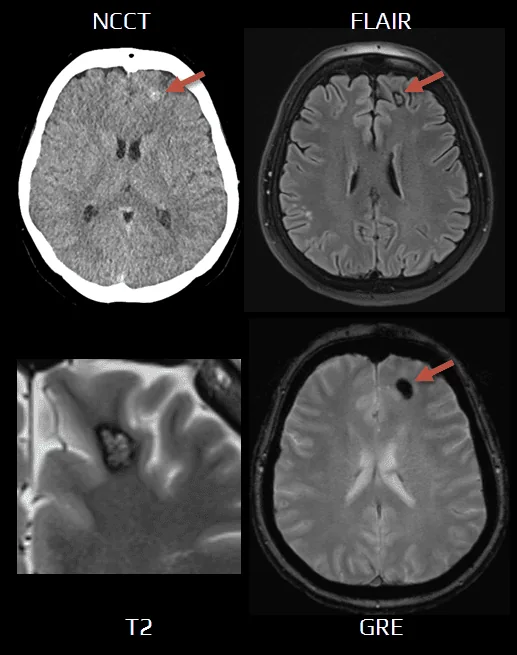
- CT
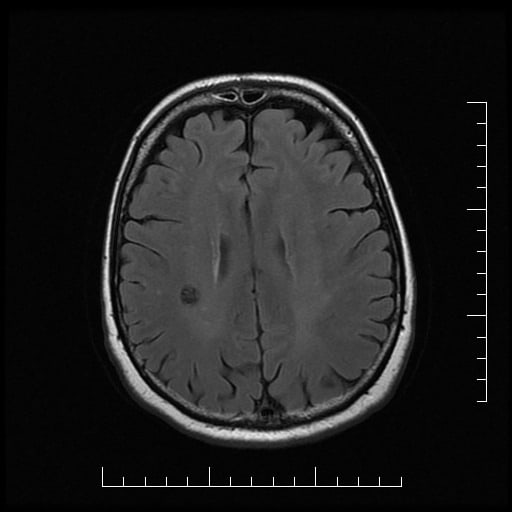
- MRI (sensitivity 100%)
- characteristic popcorn appearance
- heterogeneous lesion with a hemosiderin rim (T2-hypointense)
- prominent finding on GRE – “blooming artifact”
- slight enhancement is possible [Pinker, 2006]
- characteristic popcorn appearance
- Digital Subtraction Angiography (DSA) – cavernomas are typically not seen on DSA
It is a “susceptibility artifact” caused by paramagnetic substances
- hemosiderin
- cavernous malformation
- old hemorrhages, microbleeds
- SAH (even small superficial)
- diffuse axonal injury (DAI)
- superficial siderosis
- older thrombus
- detection of cerebral venous thrombosis (CVT)
- excessive blooming from hemosiderin is an unfavorable predictor of recanalization
[Chen, 2015]
- detection of cerebral venous thrombosis (CVT)
- cavernous malformation
- calcification
- e.g., neurocysticercosis
- Fahr disease
- metals
- gas
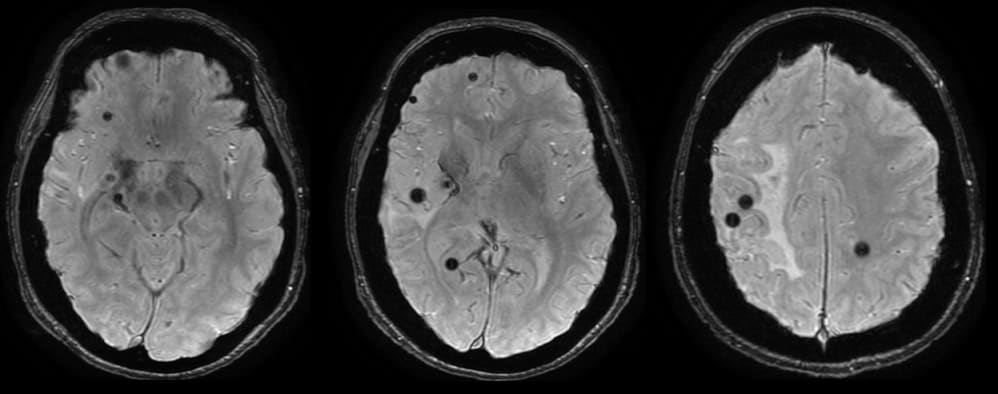
- due to the artifact, SWI is highly sensitive in detecting even small lesions, particularly those associated with hemorrhage or mineralization
- the Zabramski MRI classification has been proposed for the classification of cerebral cavernous malformations
- primarily useful for scientific purposes
- type I: subacute hemorrhage
- T1: hyperintense
- T2: hypo-/hyperintense
- type II: classic “popcorn” lesion
- T1 and T2: mixed-signal intensity centrally
- T2*/GRE/SWI: hypointense rim with blooming
- type III: chronic hemorrhage
- T1: hypointense/isointense centrally
- T2: hypointense centrally
- T2*/GRE/SWI: hypointense rim with blooming
- type IV: multiple punctate microhemorrhages
- GRE/SWI: “black dots” with blooming
- difficult to distinguish from small capillary telangiectasias
Management
Surgery and radiotherapy
- microsurgical resection
- relatively safe procedure with low morbidity and mortality [Májovský, 2014]
- proven indications:
- refractory epilepsy (up to 90% of patients are seizure-free after the surgery)
- recurrent bleeding
- in infratentorial CMs, surgery is preferred in cerebellar lesions and hemorrhagic lesions localized near the ventricle or cistern [Amato, 2013]
- markers associated with the unfavorable outcomes of surgery: a preoperative motor deficit, recurrent hemorrhage, and large cavernomas crossing the axial midpoint (Li, 2024)
- stereotactic radiosurgery (SRS) may be considered for inoperable lesions [Liščák, 2013] [Liščák, 2000]
- indications and therapy results are controversial
- in contrast to AVMs, the direct effect of therapy is not immediately observable; the long-term clinical course may differ from that of untreated lesions
Conservative therapy and follow-up
- follow-up MRI is recommended every 1-2 years for asymptomatic lesions
- keep blood pressure in the normal range
- beta-blockers may reduce the risk of intracranial hemorrhage or persistent/progressive focal neurological deficit in patients with CCM (Zuurbier, 2022)
| Size (mm) | Points | #hemorrhgaic event (HE) | Points |
| ≤ 10 | 0 | 0 | 0 |
| > 10, ≤ 20 | 1 | 1 | 1 |
| > 20, ≤ 30 | 2 | 0 | 2 |
| > 30 | 3 | ≥ 3 | 3 |
| mRS (0–5) | Points | Age (years) | Points |
| 0 | 0 | > 60 | 0 |
| 1 | 1 | ≤ 60 | 1 |
| 2 | 2 | Crossing midline | Points |
| 3 | 3 | Yes | 0 |
| 4-5 | 4 | No | 1 |
The crossover point between surgery and non-surgery recommendations lay between grades V and VI, while surgical treatment was found in favor at grades VII–X (Yang, 2021)