ADD-ONS / MEDICATION / ANTICOAGULANT THERAPY
Unfractionated Heparin (UFH)
Updated on 21/12/2023, published on 03/02/2022
- native heparin is a polymer with a molecular weight ranging from 3 to 30 kDa; the average molecular weight of most commercial heparin preparations is in the range of 12 to 15 kDa
- low molecular weight heparin (LMWH) ranges from 3 to 6 kDa
- it functions as an anticoagulant, inhibiting the formation and extension of existing blood clots
Pharmacodynamics
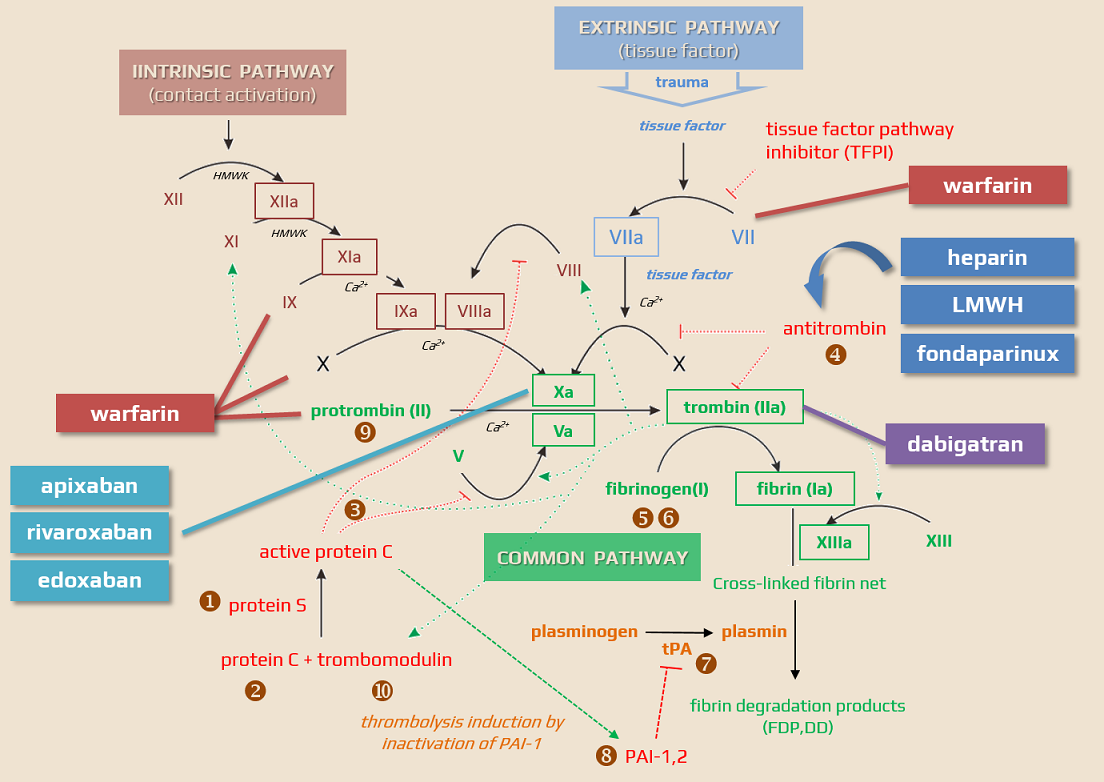
- heparin acts as an anticoagulant by activating antithrombin III (AT III)
- AT III is an α2-globulin synthesized in the liver
- it inhibits thrombin and other factors (IX, X, XI, and XII ), thereby reducing the conversion of fibrinogen to fibrin
- heparin augments AT III activity by about 1,000-fold
- in the absence of AT III, heparin is ineffective and has no fibrinolytic activity
- heparin additionally:
- releases lipoprotein lipase from the endothelium (antilipidemic effect)
- reduces platelet adhesion to the endothelium and the release of platelet-derived growth factor
- has a mild antihistamine effect
Pharmacokinetics
- the onset of the effect:
- IV – immediate
- SC – within 20-30 minutes
- biological half-life is approx. 1-2 hours (longer at higher doses); therefore, continuous infusion is preferable to intermittent IV administration
- after SC administration, peak plasma levels are reached in 2-4 hours
- heparin binds to plasma proteins; some of these proteins (involved in inflammatory or tumor diseases) neutralize its anticoagulant activity
- biotransformation occurs in the liver and reticuloendothelial system (RES)
- heparin is excreted via urine and is not dialyzable
- heparin does not cross the placental barrier and is not excreted into breast milk
Contraindications
- active, uncontrolled bleeding
- conditions with an increased risk of bleeding:
- coagulopathy (incl. liver disease)
- uncontrolled hypertension
- thrombocytopenia
- intracranial hemorrhage
- recent extensive ischemic stroke
- infective endocarditis
- aortic dissection
- recent or active gastrointestinal bleeding
- history of heparin-induced thrombocytopenia (HIT)
- hypersensitivity to heparin or its components
Dosing and monitoring
Miniheparinization (prophylactic dose)
- (1 amp=25000 IU/5ml) 5000 IU SC every 8-12 hours
- no significant differences in the incidence of pulmonary embolism or deep vein thrombosis (DVT) were observed between the two types of heparin dosing (Reynolds, 2019)
- in VTE prophylaxis, heparin has been replaced by LMWHs
- occurrence of HIT is lower in patients receiving LMWH compared to UFH (Junqueira, 2017)
Full dose heparin (therapeutic dose)
- check AT III, APTT, INR, and complete blood count (CBC) before initiating therapy
- dilute (4 mL/20,000 IU) + 16 mL of NS (1mL = 1000 IU)
- numerous concentrations are available and used; caution is required to avoid dosing errors
- if starting with a bolus, administer 50-80 IU/kg IV bolus with a maximum dose of 5000 IU
- the effects of heparin are measured via partial thromboplastin time (aPTT), which measures the time of plasma clotting; target aPTT range: 65-105 s (1.5-2.5)
- after IV bolus, proceed with continuous IV heparin infusion:
| weight (kg) | continuous infusion (IU/h) |
mL/h |
| < 50 | 500 | 0.5 |
| 50-59 | 600 | 0,6 |
| 60-69 | 700 | 0.7 |
| 70-79 | 800 | 0.8 |
| 80-89 | 900 | 0.9 |
| 90-99 | 1000 | 1.0 |
| 100-109 | 1100 | 1.1 |
| 110-119 | 1200 | 1.2 |
| > 119 | 1400 | 1.4 |
- check aPTT 6 hours after starting the therapy
- based on the results, adjust the dosage accordingly:
| aPTT (s) | stop infusion | dose change (IU/h) | check aPTT | |
| < 40 | – | + 250 IU/h | + 0.25 mL/h | in 6h |
| 40-49 | – | + 150 IU/h | + 0.15 mL/h | in 6 h |
| 50-59 | – | + 100 IU/h | + 0.1 mL/h | in 6 h |
| 60-90 | – | – | – | – next day morning |
| 91-100 | – | – 100 IU/h | – 0.1 mL/h | in 6 h |
| 101-120 | – | – 150 IU/h | – 0.15 mL/h | in 6 h |
| > 120 | for 60 min | – 250 IU/h | – 0.25 mL/h | in 6 h |
- after achieving therapeutic levels, check APTT every 12h
- avoid intramuscular injections during heparinization!
Adverse events
- bleeding complications → neutralizing the effect of heparin
- heparin-induced thrombocytopenia (HIT)
- osteoporosis (long-term, high-dose treatment)
- allergic reactions
- hyperkalemia, hyperaldosteronism
- injection site ulcer (following deep SC injections)
- elevated liver aminotransferases
- delayed transient alopecia
- rebound hyperlipidemia upon heparin discontinuation
- vasospastic reactions (including episodes of painful, ischemic, and cyanosed limbs)


