INTRACEREBRAL HEMORRHAGE / VASCULAR MALFORMATIONS
Carotid cavernous fistula (CCF)
Updated on 11/03/2024, published on 01/02/2024
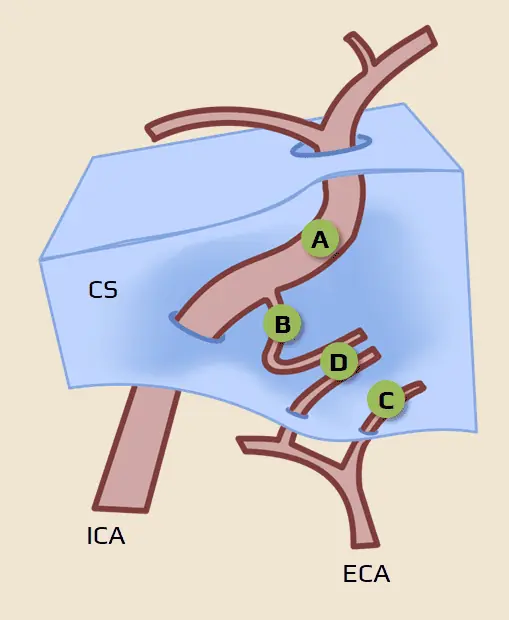
- carotid cavernous fistula is a specific variant of arteriovenous fistula (→ DAVF) – it is defined as a pathological communication between the cavernous sinus (CS) and the internal carotid artery (ICA) or its branches (from either the ICA or the ECA or both)
- CCF can occur spontaneously or as a result of trauma
- the cavernous sinus is a venous plexus that receives drainage from the sphenoparietal sinus, superior ophthalmic vein (SOV), inferior ophthalmic vein (IOV), superior petrosal sinus (SPS), inferior petrosal sinus (IPS), and basilar venous plexus → anatomy of cerebral veins and dural sinuses
Classification
- the Barrow classification is the most widely used system to categorize CCFs
- type A is usually of traumatic etiology with the classic triad of clinical symptoms (tinnitus, pulsatile exophthalmos, and conjunctival chemosis)
- indirect CCFs (C-D) are usually of spontaneous origin with milder clinical presentation
|
Etiology
|
|
|
Hemodynamic classification
|
|
|
Anatomy (type A-D) – the Barrow classification
|
|
Clinical presentation
These symptoms are usually fully expressed in type A, whereas the findings are more subtle in indirect types (often only retrobulbar pain, diffuse headache, or conjunctival hyperemia)
- pulsatile or persistent exophthalmos (proptosis)
- ipsilateral (up to 75%)
- bilateral (up to 1/3 of cases)
- contralateral to CCF
- pulsatile tinnitus (mostly synchronous with the heartbeat) + murmur audible in the forehead, synchronous with a heartbeat and disappearing after compression of the carotid artery
- painful ophthalmoparesis with diplopia (symptoms may fluctuate) [Li, 2019]
- ipsilateral amaurosis
- ipsilateral or bilateral conjunctival chemosis
- dilated subcutaneous periorbital veins
- papilledema
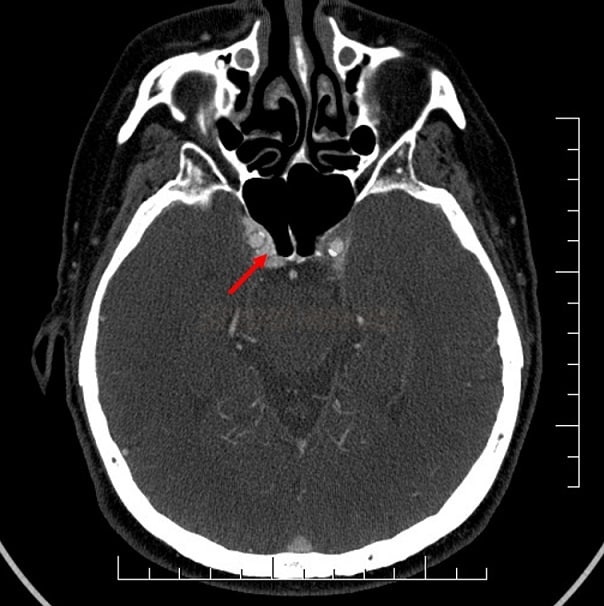
- hemorrhagic complications (2%) – SAH, ICH, epistaxis
Diagnostic evaluation
- brain CT/MRI
- vascular imaging
- ophthalmologic examination
- visual assessment
- fundoscopy – detection of vascular changes (dilated veins with potential hemorrhage) and papilledema
Management
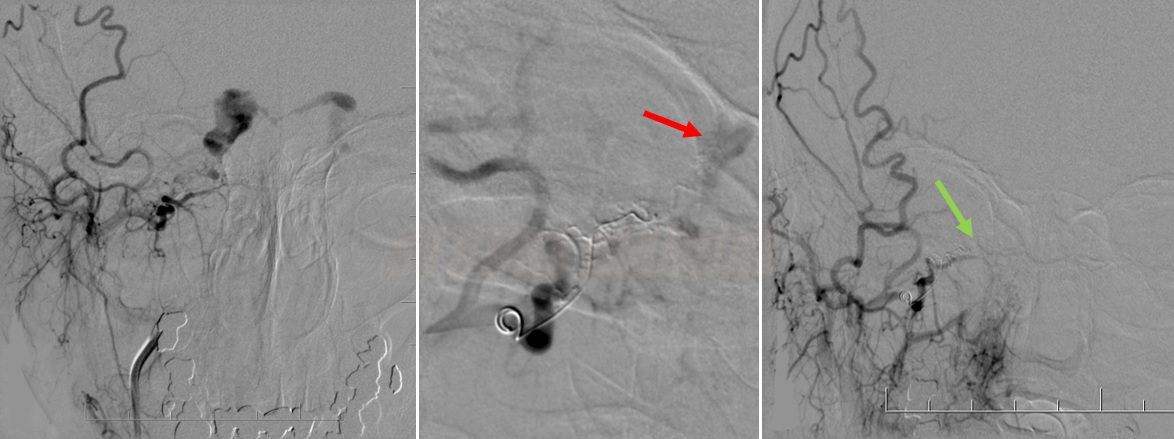
- endovascular embolization techniques (either transarterial or transvenous) are the preferred
- tinnitus typically disappears immediately following a successful procedure
- eye symptoms resolve gradually over weeks to months
Direct fistula (type A)
Endovascular treatment
| Content available only for logged-in subscribers (registration will be available soon) |
Neurosurgery
- open surgery or radiosurgery are used as second-line or adjuvant therapeutic options, typically after the prior failure of endovascular procedures
Indirect fistula (type B-D)
- it is recommended to monitor the patient with low-flow fistulas and mild symptoms, as the spontaneous resolution of symptoms due to fistula thrombosis is not uncommon
- the effect of repeated external carotid compression under ultrasound guidance has been reported [Higashida, 1986] [Goldemund, 2006)
- endovascular treatment is suggested in more severe cases and those with clinical progression (visual deterioration, malignant exophthalmos, and chemosis)
- coiling of the feeding artery
- transvenous cavernous sinus coiling