NEUROIMAGING / NEUROSONOLOGY
Hemodynamics Notes
Updated on 22/05/2024, published on 31/03/2022
- cerebral hemodynamics refers to the principles and mechanisms of blood flow in the brain
- understanding these principles is crucial not only for ultrasound diagnosis but also for managing cerebral disorders, evaluating the impact of certain conditions on cerebral blood flow, and planning interventions to improve or restore cerebral circulation
- Doppler ultrasound is a critical tool for evaluating blood flow velocity and direction as it can provide real-time data on hemodynamics
Blood flow
- hemodynamics = the dynamics of blood flow
- blood flow refers to the movement of blood through the vessels (arteries → arterioles → capillaries → venules → veins)
- blood flow is slowest in the capillaries, allowing sufficient time for the exchange of gases and nutrients
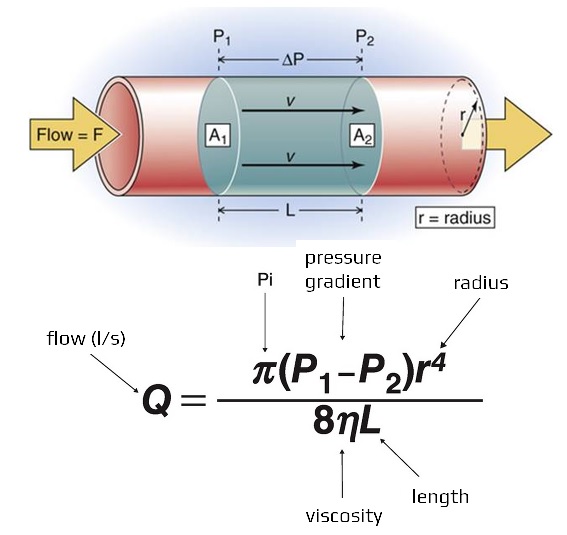
- flow (Q, mL/s) – directly depends on the pressure difference between the two ends of the tube and indirectly on the tube resistance: Q= ΔP/ R
- pressure (P)
- pressure is the force exerted by blood against the walls as it moves through the vessels
- it consists of three components:
- the dynamic component is determined by the cardiac output and peripheral flow resistance
- the hydrostatic component is defined by gravity
- a static component (mean filling pressure) depends on the filling volume and the systemic volume capacity
- blood flows from a high-pressure area to a region with lower pressure
- very little pressure remains when blood leaves the capillaries and enters the venules. Blood flow through the veins is not a direct result of ventricular contraction. Instead, venous return depends on skeletal muscle action, respiratory movements, and constriction of smooth muscle in the venous wall
- resistance (R)
- a force that opposes the flow of a fluid
- flow resistance R= 8 . . L / π.r⁴ directly depends on blood viscosity and artery length; it is also inversely proportional to the fourth power of the artery radius (cross-sectional area) – as vessel diameter decreases, the resistance increases, and blood flow decreases
- = the radius of the pipe (vessel)
- = the viscosity of the fluid
- L = the length of the pipe
- this formula assumes laminar flow, constant viscosity, and a long cylindrical pipe
- pulse = the rhythmic expansion of an artery caused by the ejection of blood from the ventricle. Pulse can be palpated on arteries that are close to the surface
- blood pressure (BP) = pressure in the aorta and its branches
- systolic blood pressure (SBP) is caused by ventricular contraction
- diastolic blood pressure (DBP) occurs during cardiac relaxation
- pulse pressure is the difference between systolic and diastolic blood pressure
- blood pressure is measured with a sphygmomanometer and is recorded as the systolic pressure over the diastolic pressure
- 4 significant factors affect blood pressure:
- cardiac output
- blood volume
- peripheral resistance
- viscosity
- blood pressure is maintained by changes in cardiac output and peripheral resistance. Baroreceptors in the walls of the large arteries in the neck are essential for short-term regulation of blood pressure
Character of the flow
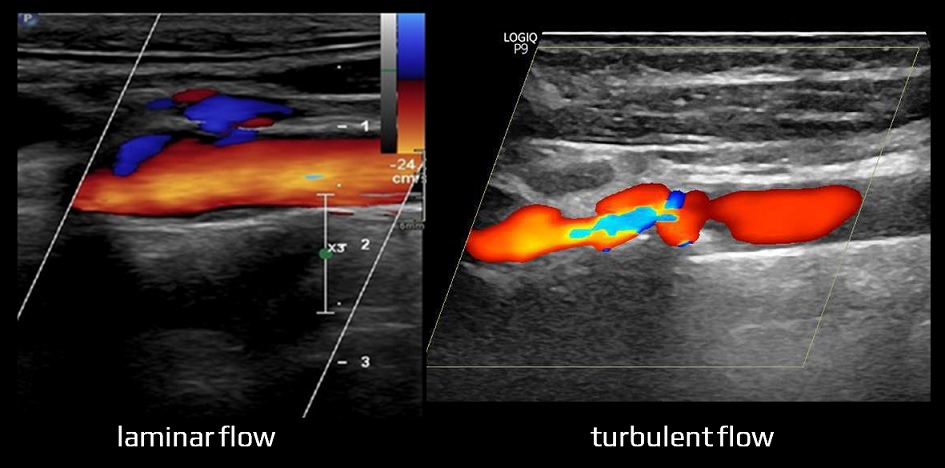
- laminar flow is characterized by the organization of flow in concentric layers (fluid particles move in parallel layers). The individual layers of blood flow move at a constant velocity that increases from the wall to the center of the vessel; the layers do not mix
- turbulent flow – as the blood velocity in the vessel increases or the vessel is constricted, laminar flow is disrupted by turbulence (depicted as aliasing in color mode)
- the propensity for turbulent flow increases in direct proportion to flow velocity (), vessel diameter (d), and blood density (ρ) and is inversely proportional to blood viscosity ()
- fluid particles move in a chaotic and random manner
- occurs at high velocities and is characterized by a high Reynolds number (Re typically > 2000)
- Re= ρ .u .d /
- ρ fluid density
- u = flow velocity
- d = diameter of the vessel
- fluid viscosity
- Poiseuille’s law does not apply to turbulent flow
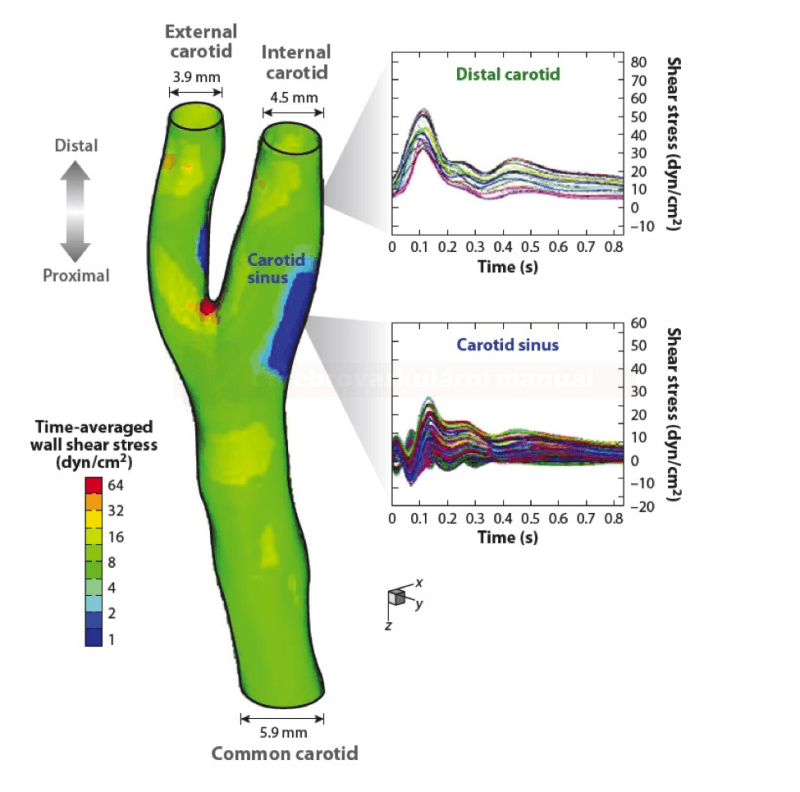
Flow separation
- flow separation occurs at arterial bifurcations, aneurysms, atherosclerotic plaques or stenoses, or at sites of vessel enlargement
- in the carotid bulb, the turbulent flow is physiological – there is an increased Reynolds number (> 2000)
- these zones predispose to early remodeling of the vessel wall and atherosclerotic changes (due to the altered shear stress) [Cunningham, 2005]
Waveform
- several factors influence the character of the flow:
- heart ejection fraction (EF)
- flow volume and pressure
- resistance and geometry of the vascular system
- vessel wall elasticity
- blood viscosity
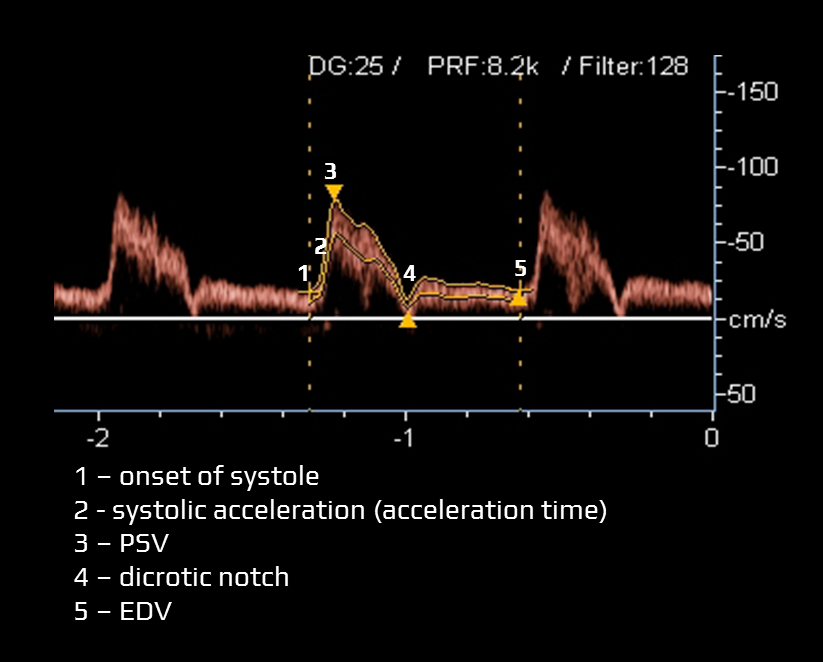
- the Doppler waveform refers to the morphology of pulsatile blood flow on spectral Doppler ultrasound
- typical items assessed within the Doppler waveform:
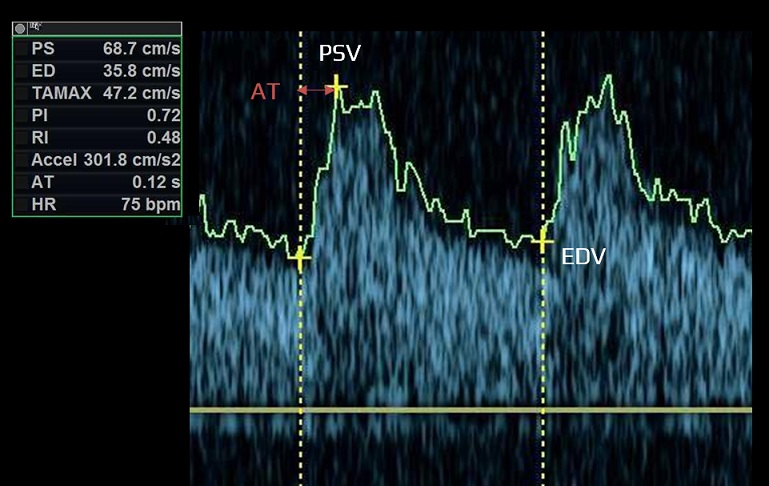
- acceleration time (systolic acceleration)
- time required for blood flow to reach peak velocity from the onset of systole (measured in milliseconds)
- a prolonged acceleration time may indicate proximal arterial stenosis/occlusion, stenosis of the aortic valve, or impaired cardiac contractile force
- peak systolic velocity (PSV) – the highest flow velocity during systole
- dicrotic notch
- a slight, downward deflection observed after the peak systolic velocity. This notch corresponds to aortic valve closure and the beginning of diastole in the cardiac cycle
- a prominent dicrotic notch may be indicative of increased peripheral resistance, commonly observed in conditions such as hypertension
- conversely, a blunted or absent dicrotic notch may indicate low systemic vascular resistance and may be seen in conditions like sepsis
- end-diastolic velocity (EDV)
- EDV is the velocity at the end of diastole; it is influenced by peripheral resistance (including distal stenosis)
- mean velocity (Vmean) is calculated
- resistance index and pulsatility index can be calculated from the above-stated values
- acceleration time (systolic acceleration)
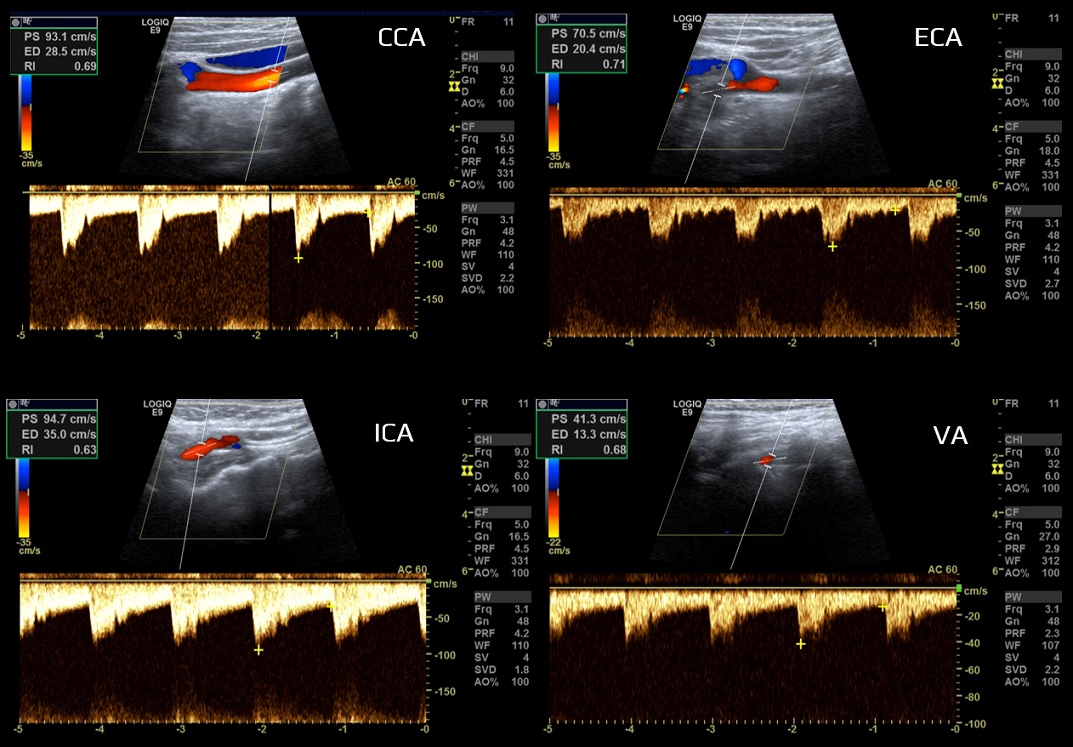
- vessels are classified according to the peripheral resistance
- high-resistance limb type (typically the ECA)
- low-resistance parenchymal type (typically the ICA, VA)
- the CCA waveform has an intermediate profile under physiological conditions because it depends on peripheral resistance in both intracranial (brain) and extracranial regions (skin, muscles)
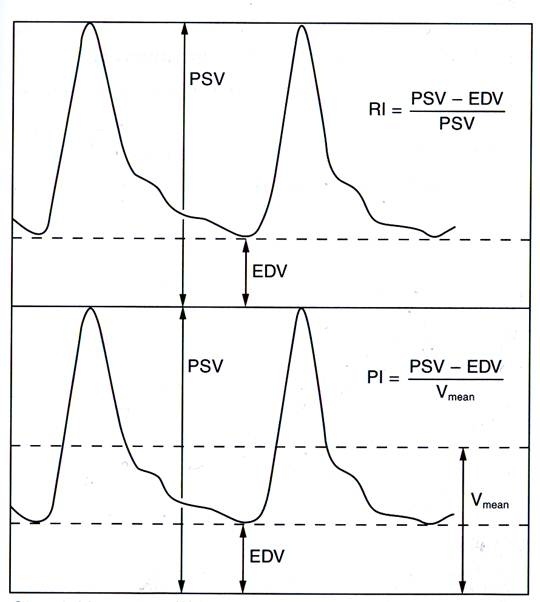
Resistance and pulsatility index
- Resistance Index (RI) and Pulsatility Index (PI) are calculated as follows:
- RI = (PSV-EDV) / PSV
- PI = (PSV-EDV) / Vmean
- Vmean = 1/3 (PSV-EDV) + EDV
- these indices are calculated automatically by the ultrasound device as a time-weighted average of systolic and diastolic flow rates
- the resistance index (RI) considers only two points on the Doppler velocity curve (PSV, EDV)
- PI is more comprehensive for assessing peripheral vascular wall resistance, as it incorporates the mean velocity throughout the entire cardiac cycle, in addition to PSV and EDV
Hemodynamic changes in vascular pathologies and anatomical variants
Variants of normal artery course
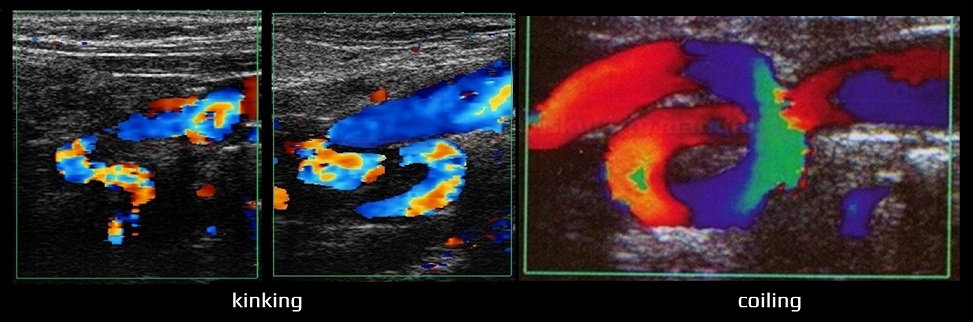
- tortuosity, kinking, and coiling
- in such abnormalities, the maximum flow within the bend is shifted towards the outer wall
- turbulence may occur, potentially leading to a risk of false stenosis detection
Stenosis
- hemodynamic consequences of stenosis:
- primary (accelerated, turbulent flow in the stenotic segment)
- secondary (reduced flow in the pre-and poststenotic segments)
- tertiary (collateral circulation)
- primary (accelerated, turbulent flow in the stenotic segment)
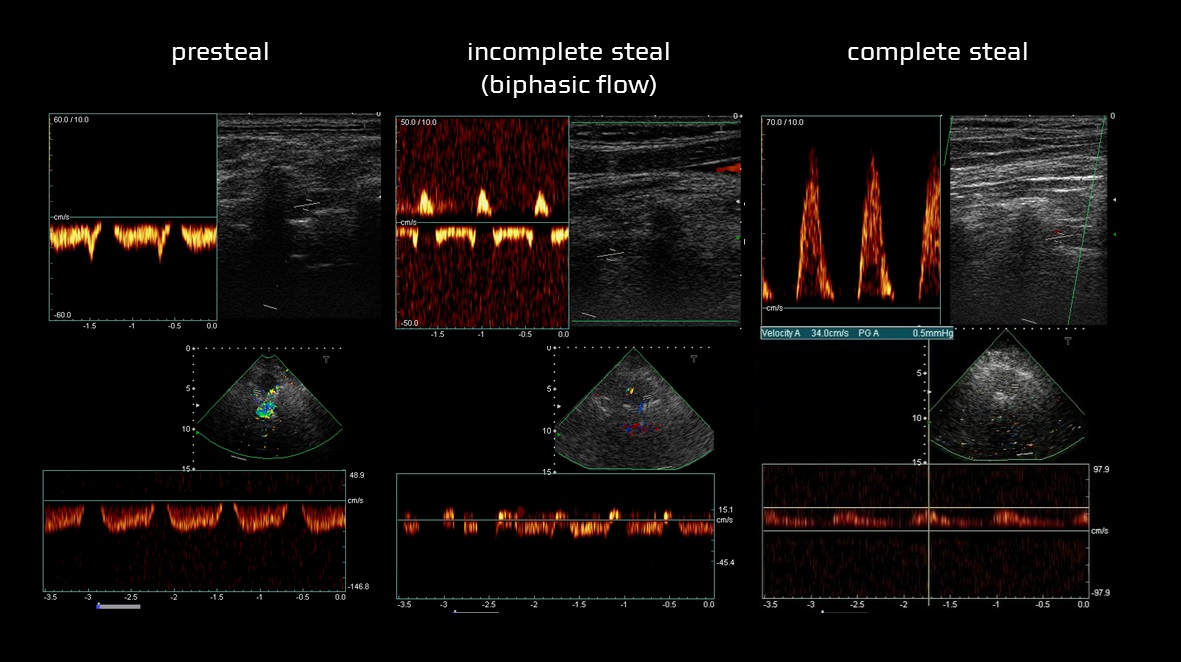
Steal phenomenon
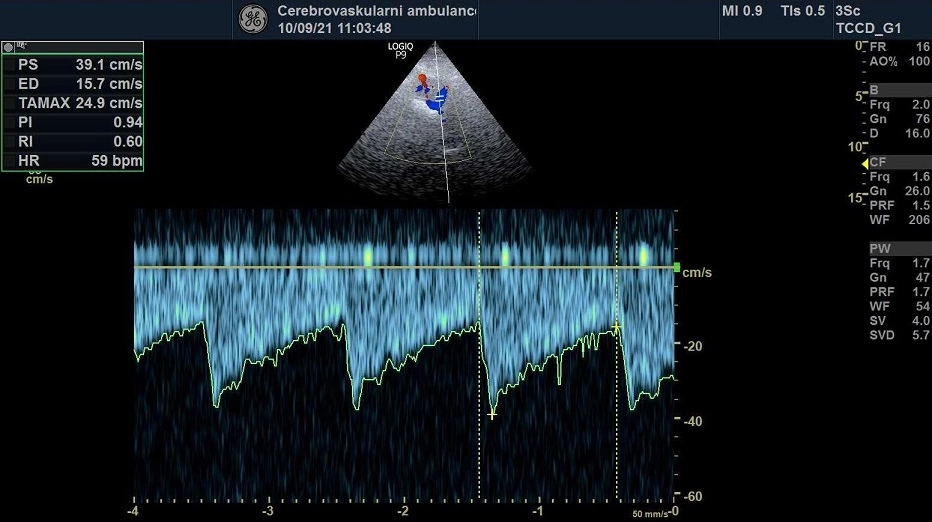
- steal syndrome is a condition where blood flow is diverted due to collateral circulation or the presence of a high-flow vascular malformation
- in subclavian steal syndrome, altered (typically retrograde or alternating) blood flow occurs in the vertebral artery (VA) or the internal thoracic artery, resulting from proximal stenosis or occlusion of the subclavian artery (SA) or brachiocephalic trunk (BCT)
- Doppler ultrasound is commonly used to diagnose and grade the severity of subclavian steal
- grade 0: normal antegrade flow in the vertebral artery
- grade I: reduced antegrade flow with no retrograde flow
- grade II: intermittent retrograde flow (alternating), especially during arm exercise
- grade III: continuous retrograde flow at rest