NEUROIMAGING / NEUROSONOLOGY
Cerebral vasomotor reactivity (CVR) testing
Updated on 07/11/2023, published on 26/10/2023
Definition of cerebral vasomotor reactivity (CVR)
- Cerebral Vasomotor Reactivity (CVR or CVMR) refers to changes in smooth muscle tone in the arterial wall in response to certain vasodilatory stimuli (commonly changes in PaCO2 or pH)
- do not confuse with cerebral autoregulation, which means the ability of cerebral arterioles to maintain a constant cerebral blood flow (CBF) despite fluctuations in systemic blood pressure
- CVR and cerebral autoregulation are two major mechanisms that regulate cerebral blood flow (CBF)
- impaired CVR indicates compromised regulation of cerebral circulation and increased vulnerability of the brain to ischemic events
- the annual risk of ischemic stroke is higher with impaired CVR (13.9% vs. 4.1%) [Silvestrini, 2000]
- impaired CVR is also associated with an increased risk of death; incident stroke does not affect this association, suggesting that lower CVR reflects a generally compromised vascular system [Portegies, 2013]
- in cases of significant extracranial stenosis, CVR testing allows assessment of the collateral circulation status and the risk of hemodynamic failure; demonstration of impaired CVR may support the indication for CEA in asymptomatic individuals
Physiology
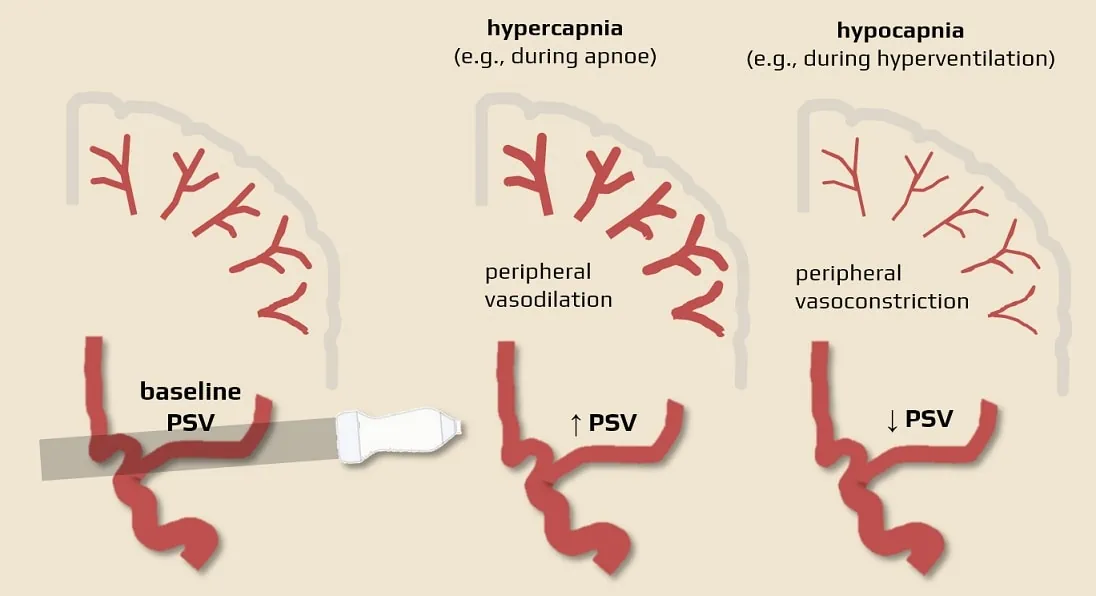
- cerebral blood flow is influenced by PaCO2 and pH
- ↓PaCO2 (e.g. hyperventilation) CBF decreases (vasoconstriction → ↑peripheral resistance → decreased flow in proximal segments, e.g. M1)
- ↑PaCO2 CBF increases (vasodilation → ↓ peripheral resistance → increased flow in proximal segments, e.g. M1)
- when CVR is exhausted, vasodilatation is already maximal, and the decrease in perfusion pressure can no longer be compensated, resulting in an immediate decrease in cerebral blood flow (CBF)
- in general, CVR can be defined as the difference between the cerebral blood flow velocity before and after the use of a vasodilating stimulus
Methods to measure cerebrovascular reserve
- Transcranial Doppler (TCD/TCCD) (Müller, 1995)
- utilizes vasodilatory agents like hypercapnia or IV acetazolamide to stimulate cerebral vasodilation
- TCD/TCCD measures blood flow velocity changes in response to these stimuli
- acetazolamide-challenged methods
- Positron Emission Tomography (PET)
- provides high-resolution images and quantitative assessment of CVR
- Arterial Spin Labeling (ASL) MRI (Zhao, 2022)
- Single-photon emission Computed Tomography (SPECT)
- lower resolution and less quantitative compared to PET
- Blood Oxygen Level Dependent (BOLD) MRI
- CT/MR perfusion (Kim, 2010)
- Positron Emission Tomography (PET)
Ultrasound Evaluation of CVR
- measurement usually uses a transcranial ultrasound (TCD/TCCD) along with vasodilatory stimuli such as hypercapnia or acetazolamide
- breath-holding and apnea/hyperventilation tests seem to be practical for rough assessing cerebral hemodynamics
- the disadvantage of this method is that patients may not be able to tolerate breath-holding long enough to achieve hypercapnia
- acetazolamide injection and CO2 inhalation test with capnometry are more accurate
- patients should be examined in a comfortable supine position in a quiet room with standard room temperature
Breath-holding index (BHI)
- the Breath-Holding Test is a simple method to measure CVR (noninvasive, well tolerated, reproducible)
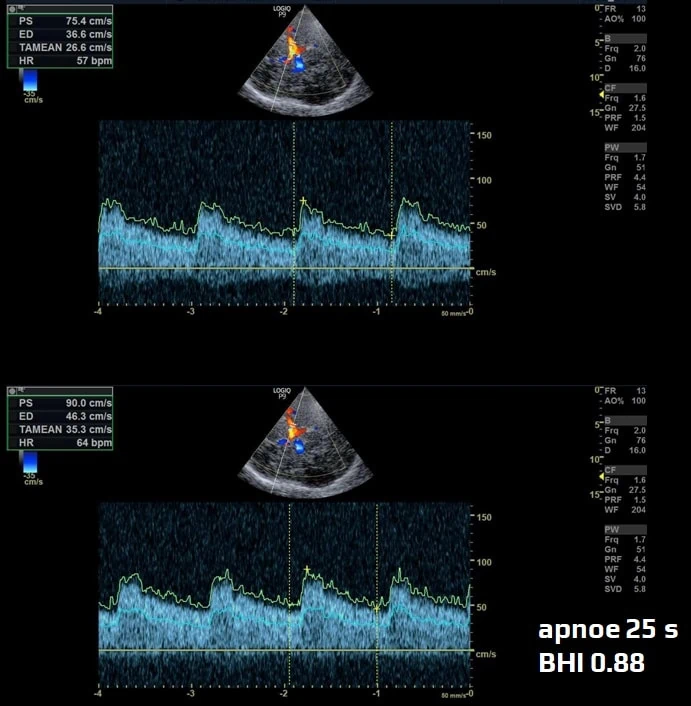
- baseline velocity (V1) is measured in the M1 segment of the MCA or BA
- then the patient holds their breath as long as possible without taking a deep breath (t – time of apnea in seconds)
- measure the velocity at the end of apnea (V2 – if hypercapnia is achieved, peripheral vasodilation with increased flow in the M1 segment of the MCA occurs)
- determine the BHI using the following formula:
- 0.7-1.8
- 1.2 ± 0.6 (Widder, 2014)
- most commonly 1.03-1.65 (Zavoreo 2003)
- 1.45 ± 0.50 ; PIV (percentage increase in flow velocity) values being 31.6 +/- 12.3% (
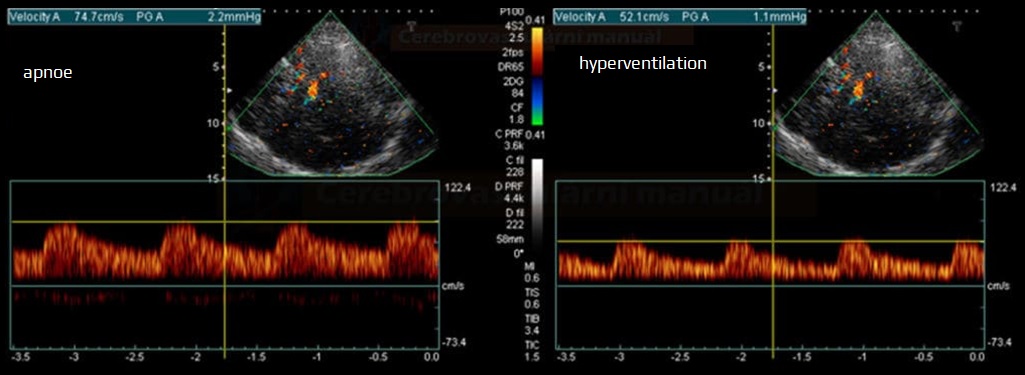
Apnoe/hyperventilation (BH/HV) test
- designed to evaluate cerebral autoregulatory function by inducing both hypo- and hypercapnia
-
Vbaseline
-
V1 – PSV after 10-20s of breath-holding (↑ PSV in proximal MCA due to peripheral vasodilation)
-
V2 – PSV after 40s moderate hyperventilation (↓ PSV)
-
normal finding: change of V1/V2 against baseline >15-30% (values vary in the literature)
|
CVR
|
|
| preserved | normal reaction |
| decreased | absent reaction to hypercapnia |
| exhausted | absent reaction to both hypo- and hypercapnia |
| paradoxical reaction | reduced flow during hypercapnia (due to the steal phenomenon) |
Acetazolamide test
- acetazolamide is used as a vasodilator stimulant
- reversible inhibitor of the enzyme carbonic anhydrase
- increases CBF by dilating the arterioles; metabolic changes induced by acetazolamide include increased extracellular pCO2 and decreased extracellular pH
- baseline velocity is obtained, commonly in the proximal MCA (V1)
- IV injection of acetazolamide is administered to induce cerebral vasodilation, typically at a dose of 15-20 mg/kg
- post-administration velocities (typically after 10-20 minutes) (V2)
- CVR is calculated as the percentage change in flow velocity between baseline and peak velocity after acetazolamide administration
- increase of > 20-40% is generally considered normal CVR
- increase of < 20% suggests impaired CVR
FAQs
- CVR refers to changes in smooth muscle tone in the arterial wall in response to vasodilatory agents (pH or PaCO2)
- yes, CVR and CBF are directly related; reduced CVR generally implies the compromised ability to increase CBF
- reduced CVR may indicate compromised cerebral blood flow regulation and elevated risk of ischemic events
- CVR is often reduced post-stroke, increasing the vulnerability to further ischemic injury
- CVR serves as an important prognostic marker in various cerebrovascular diseases, including chronic steno-occlusive disorders and stroke. Reduced CVR often indicates impaired autoregulatory capacity, signifying an increased risk for ischemic events
- age, systemic blood pressure, medications, underlying cerebrovascular pathology (significant stenosis)
- CVR is typically assessed using transcranial Doppler ultrasound, PET, SPECT, or special MRI sequences (ASL, BOLD), after exposure to a vasodilatory agent
- CVR assessment is not yet routine but is increasingly used in specialized centers for evaluating cerebrovascular pathology