GENERAL NEUROLOGY
Management of intracranial hypertension
Updated on 10/05/2024, published on 10/05/2024
- intracranial hypertension (ICH) is a critical condition characterized by elevated intracranial pressure (ICP) above the normal range (commonly used threshold is > 20 mmHg or 27 cm H2O)
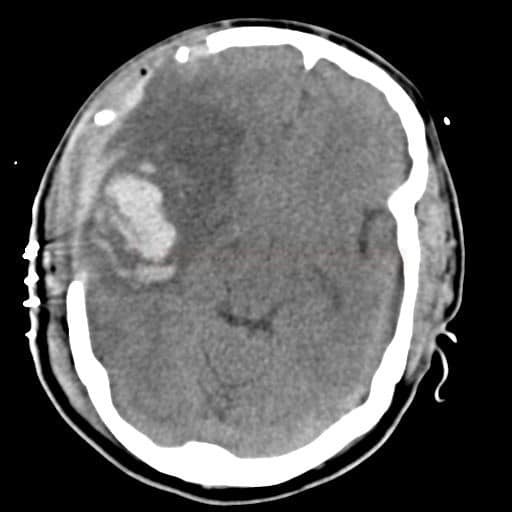
- it results from various etiologies such as traumatic brain injury, stroke, tumors, or hydrocephalus
- prompt recognition and management are essential to prevent irreversible brain damage
- the management aims to:
- reduce the mass effect and ICP, and prevent secondary brain injury from herniation
- maintain adequate cerebral perfusion to avoid worsening of the brain ischemia in stroke patients or causing secondary ischemic damage in TBI, hemorrhage, etc.
- manage factors that contribute to the worsening of intracranial hypotension
- CPP > 60-70 mm Hg
- ICP < 15-20 mm Hg (normal range 0-10 mm Hg)
- SvjO2 > 60%
- tissue pO2 > 25 mmHg (critically low < 10 mmHg)
- SpO2 > 97%
- PaCO2 4.5-5 kPa
- normothermia
Causal therapy
- procedures targeted on pathological conditions directly leading to intracranial hypertension (e.g., evacuation of hematoma, recanalization of thrombosed vessels, treatment of neuroinfection, ventricular drainage in obstructive hydrocephalus, etc.)
General therapy
General therapy focuses on factors that exacerbate raised ICP (hypotension, hypoxia, hypercarbia, hyperthermia, hyperglycemia, etc.) and prevents/treats various complications
- prevent hypoxia and hypercapnia
- target SpO2 > 97%
- target PaCo2 4.5-5.5 kPa (35-40 mmHg)
- avoid hypercapnia-induced vasodilation (it leads to vasodilatation with further progression of intracranial hypertension)
- maintain euvolemia (or mild restriction) and normotension (or mild hypertension)
- MAP > 90 mm Hg, SBP 130-160 mm Hg
- do not administer hypotonic solutions (such as 5% dextrose in water)
- monitor central venous pressure (5-12 cm H2O)
- avoid anti-hypertensive drugs that induce cerebral vasodilatation
- elevate the head of the bed to 30° to enhance venous drainage
- facilitates the outflow of blood from the brain, thereby reducing ICP with a consequent increase in CPP
- avoid external pressure on the neck
- monitor and correct electrolytes
- maintain Na 145-150 mmol/L), serum osmolality > 310 mmol/L
- normoglycemia
- maintain normothermia
- sedation and analgesia – to reduce metabolic demand and agitation
- boluses of short-acting barbiturates (such as propofol) are used to avoid ICP fluctuations during suctioning from airways and other painful procedures
- anti-seizure therapy → see symptomatic seizures
- seizures cause an increase in metabolic level, CBF, and oxygen consumption rise
- prophylactic administration of ASM is generally not recommended
- some centers administer ASMs prophylactically to prevent early seizures, but no statistically significant beneficial effect has been shown to affect the frequency of poststroke (stroke-related) epilepsy
Pharmacotherapy of brain edema
Corticosteroids
- corticosteroids are reserved for vasogenic edema associated with tumors or abscesses
- not recommended for TBI and stroke patients (AHA/ASA 2019 III/A)
- dexamethasone
- DEXAMED (amp/2mL/8mg) IV bolus of 4-8 mg every 6-8 hours
- FORTECORTIN 4mg PO every 6-8 hours
Osmotic therapy
- the aim is to increase the osmolality of the blood and thus create an osmotic gradient between the interstitium and the vascular compartment ⇒ ↓ water volume in brain tissue
- effective in vasogenic and cytotoxic edema
- do not use prophylactically, only in the presence of IC hypertension
- regular monitoring of electrolytes (Na, K, Cl, P, Mg) and osmolarity is required
- administer for the shortest possible time (max effect < 5 days)
- discontinue gradually (rebound phenomenon)
- alternating administration of Mannitol and NaCl is advantageous
- MANNITOL 15% (250 mL/37.5g)
- initial dose: 1-1.5 g/kg/15min
- subsequently, 0.25-0.5 g/kg over 20-30 minutes every 6-8 hours
- max dose: 2g/kg/day (i.e. 140g in a 70kg person)
- monitor osmolality during therapy (maintain < 320 mOsm/L)
- onset of action: 10-15 min
- routine administration in patients with acute stroke is not recommended
- administer in selected patients with initial large infarction, a decreased level of consciousness, or evidence of a mass effect on imaging (ICP > 20 mm Hg)
- mannitol reduces the amount of water in brain tissue (usually the healthy one) + improves the rheological properties of the blood
- AEs: fluid and electrolyte imbalance hyperosmolarity, cardiopulmonary edema, hypovolemia with hypotension, renal failure ⇒ monitor renal function and fluid balance
NaCl 3% 1.5-2 mL/kg every 4-6 h
NaCl 10% 3.4 mOsm(1ml)/kg in bolus every 4-8 h (via central venous access!)
- usually administered when mannitol fails
- do not administer 10% NaCl into a peripheral vein!
- do not administer to hyponatremic patients
- can preferably be given in hypovolemic patients
- maintain Na/S < 150-160 mmol/l
- monitor acid-base balance (risk of hyperchloremic acidosis)
FUROSEMIDE 40mg IV every 6-8 hours
- loop diuretics reduce CSF production
- increases water output in the distal renal tubules
- co-administration of furosemide and mannitol potentiates each other’s effect; the greatest effect on ICP fall is when furosemide is administered 15 minutes before mannitol; alone, it has minimal effect
Advanced therapy
- uses autoregulatory mechanisms in unaffected areas (vasoconstriction ⇒ ↓ vascular compartment volume)
- however, hypocapnia-induced vasoconstriction can lead to impaired perfusion and worsening ischemia
- should only be used as a short-term solution, e.g., during preparation for decompressive craniectomy, and SvjO2 (> 55%) should be monitored
- PCO2 reduction by 5–10 mmHg can lower ICP by 25–30%; absent response to hyperventilation is an unfavorable prognostic sign
- target pCO2 is typically 30-35mmHg (25-30mmHg may be used for short periods) while maintaining SvjO2 > 55%; hypocapnia should be achieved by higher respiratory rate
- can be used in acute stroke patients (AHA/ASA 2018 IIa/C-EO)
- discontinue the therapy gradually
1 mmHg = 0.13 kPa
30 mmHg = 4 kPa
- recommended for refractory cases, especially in patients with secondary brain injury
- barbiturate coma lowers metabolic demand and leads to vasoconstriction
- monitor for burst suppression patterns during barbiturate coma
- barbiturate coma has significant negative effects on the cardiovascular system (hypotension) and patients must be invasively monitored
- barbiturates are usually not recommended for acute stroke patients (AHA/ASA 2018 III/B-R)
- generally indicated when conventional therapy for intracranial hypertension fails
- most data available for traumatic brain injury and post-resuscitation states (e.g., after ventricular fibrillation, cardiac arrest)
- clearly reduces ICP (evidence I), but the clinical effect is variably assessed
- hypothermia is not proven effective for stroke, and it is not routinely recommended (AHA/ASA 2018 III/B-R)
- hypothermia causes:
- ↓ CMRO2 (approximately 7% per 1°C) ⇒ ↓ CBF and CBV
- stabilization of cell membranes (affecting cytotoxic edema)
- hypothermia is induced locally (ice packs around the head) or systemically with a target temperature of 34–35°C for a minimum of 12–72 hours (post-resuscitation)
- temperatures <34°C increase the risk of adverse effects (arrhythmias, coagulopathies)
- gradual rewarming at 0.1–0.25°C/h after treatment is recommended