ISCHEMIC STROKE / ETIOLOGY AND CLASSIFICATION
Cholesterol Embolization Syndrome
Updated on 10/01/2024, published on 13/05/2023
Definition
- cholesterol embolization occurs when small pieces of cholesterol plaque break off from the arterial walls and block small and medium-sized arteries, which can lead to tissue damage
- large arteries, especially the aorta and its branches, are the usual source of emboli in elderly patients with advanced atherosclerosis
- embolization is often associated with intravascular procedures, cardiac surgery, and vascular surgery
- it differs from the more common artery-to-artery thromboembolism, in which thrombi formed on the surface of an atherosclerotic plaque embolize into the peripheral circulation
- symptoms may include skin discoloration, pain, and organ dysfunction
Etiopathogenesis
- atherosclerotic plaques in in mid-size and large arteries (aorta, CCA, ICA, pelvic arteries) → atherosclerotic plaques classification
- plaque formation results from a long-term process of lipid particle deposition in the vessel wall, accompanied by a cellular and inflammatory response
- complex plaques are characterized by a thickness of ≥ 4 mm and an irregular, often exulcerated surface. Blood clots (thrombi) occur on the surface of these lesions to varying degrees and extents, frequently associated with atheroembolism and thromboembolism
- plaque rupture can occur, leading to the release of atheroma masses and cholesterol crystals (spontaneous, traumatic, iatrogenic) and their embolization to peripheral segments
- iatrogenic – during cardiac catheterization, cardiac surgery, angioplasty
- with advancements in catheterization techniques, the incidence of cholesterol embolization is decreasing
- the incidence of cholesterol embolization during renal artery catheterization procedures is reported to be as high as 30%. This condition typically presents as asymptomatic or may involve a transient increase in urea and creatinine levels
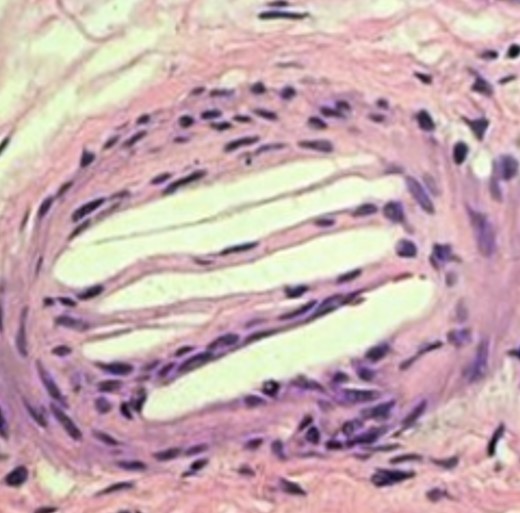
- embolization to small and medium-sized vessels, resulting in their occlusion
- systemic inflammatory response to cholesterol emboli
- may result in local endothelial proliferation with intimal fibrosis, leading to narrowing or permanent occlusion of the affected artery
- organ damage can occur caused by artery occlusion with hypoperfusion and inflammatory response
Clinical presentation
- clinical presentation depends on the extent of the target organ damage
- kidneys, gastrointestinal tract (GIT), brain, skin, and lower limb muscles are the most commonly affected
- brain damage – focal or diffuse embolization, resulting in stroke or encephalopathy
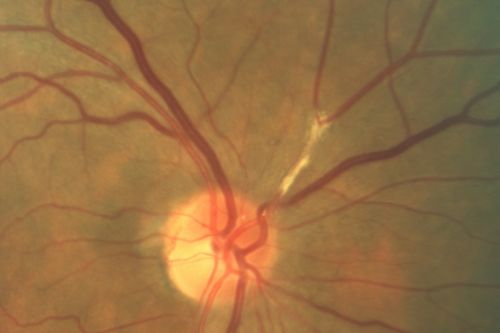
- retinal embolization – amaurosis fugax or permanent retinal damage
- detection of Hollenhorst plaques confirms the diagnosis
- nephropathy – in addition to embolization, contrast-induced nephropathy (CIN) may contribute to renal injury during interventional procedures
- GIT – intestinal ischemia with abdominal pain, bleeding from ulcerations, and mucosal erosions is most common; acute pancreatitis or acalculous necrotizing cholecystitis are less frequent
- skin manifestations – typically affecting the legs, rarely the trunk and upper extremities
- common skin symptoms include livedo reticularis (marbled skin, reddish patches), gangrene, cyanosis, ulcerations, nodules, and purpura
- blue toe syndrome – may also be a manifestation of vasculitis, hypercoagulable and hyperviscosity syndrome, and endocarditis
Diagnostic evaluation
- the clinical manifestation of cholesterol embolization syndrome is nonspecific and consists of a combination of end-organ lesions and a systemic inflammatory response
- cholesterol crystals trigger an inflammatory response (fever, fatigue, anorexia)
- laboratory findings commonly include leukocytosis, anemia, and thrombocytopenia, as well as an increase in ESR and CRP levels
- the syndrome should be considered in elderly patients with documented organ manifestations of advanced atherosclerosis, acute renal injury/hepatitis, hypereosinophilia, and skin manifestations such as livedo reticularis or “blue toe syndrome”. Particularly if they have undergone interventional or surgical procedures on large vessels before clinical presentation
- imaging techniques – enables visualization, quantification, and characterization of atherosclerotic lesions
- CT+CTA / MRI+MRA
- neurosonology
- detects atherosclerotic changes in extra- and intracranial cerebral arteries
- monitoring of spontaneous and provoked embolizations during interventional procedures; method can not distinguish cholesterol microemboli from thrombi
- detects atherosclerotic changes in extra- and intracranial cerebral arteries
- TEE (can assess aortic arch atherosclerosis)
- direct confirmation of atheroma embolization
- skin or renal biopsy with evidence of atheroma emboli
- plaques/crystals in the retina
- Hollenhorst plaque – yellowish, typically located at an arterial bifurcation
- DDx: calcium plaque from cardiac valves, which is whiter than Hollenhorst plaque and usually gets stuck at more proximal retinal arteriolar branch segment
- Hollenhorst plaque – yellowish, typically located at an arterial bifurcation
Management
Treatment of underlying atherosclerosis and prevention of further embolization
- intensive management of vascular risk factors (smoking cessation, dyslipidemia, hypertension, diabetes)
- high-intensity statins are recommended
- antiplatelets (to prevent concurrent thrombosis)
- surgery or endovascular intervention in cases with significant stenosis
Symptomatic therapy and management of organ-specific complications
- address neurological complications such as stroke or encephalopath with standard protocols for stroke management, including thrombolytics if indicated
- the benefit of thrombolysis is questionable, but concomitant thrombolysis-sensitive atherothrombotic embolization cannot be excluded
- wound care and management of skin ulcers and gangrene
- manage intestinal ischemia, bleeding, or other GIT complications with supportive care, blood transfusions, and sometimes surgery when indicated
- monitor renal function closely, and if necessary, consider dialysis for severe cases
- pain management
Prevention
- primary prevention of atherosclerosis in high-risk patients, including controlling risk factors and ensuring proper perioperative care to minimize the risk of embolization during medical procedures