ISCHEMIC STROKE / STROKE MIMICS
Transient global amnesia (TGA)
Updated on 11/03/2024, published on 24/03/2021
- transient global amnesia (TGA) is a sudden, temporary (lasting < 24h) episode of memory loss with the absence of other neurological signs that can’t be attributed to more common neurological conditions, such as epilepsy or stroke
- TGA is mostly non-recurrent
- can be triggered by intense emotional experiences
- annual incidence ~ 5–11 per 100,000 people in the general population, with a higher prevalence in individuals over 50 years of age
- TGA is considered a benign disorder; recurrences are relatively uncommon (12–19%), and it is not associated with an increased risk of stroke [Mangla, 2013]
Clinical presentation
- sudden onset of memory loss, verified by a witness, duration < 24 h (mostly 3-6 h, rarely > 12h), usually with the gradual return of memory
- anterograde amnesia
- inability to form new memories and to recall recent past events
- a common feature includes repetitive questioning, typically asking the same questions (“How did we get here?”, “What am I doing here?”)
- inability to form new memories and to recall recent past events
- retrograde amnesia
- inability to recall events that immediately preceded the memory loss
- anterograde amnesia
- retention of personal identity despite memory loss
- normal cognition, such as the ability to recognize and name familiar objects and follow simple directions
- the patient may be slightly restless and anxious, but adequately given the situation
- absence of focal neurological deficits (hemiparesis, involuntary movements, problems with speech, apraxia, etc.)
- no evidence of seizures during the amnestic episode and no history of active epilepsy
Hodges and Warlow diagnostic criteria for Transient Global Amnesia
- the attacks must be witnessed
- anterograde amnesia must occur during an attack
- cognitive impairment should be limited to amnesia
- no clouding of consciousness or loss of personal identity
- no focal neurological signs/symptoms
- no epileptic features
- the attack must resolve within < 24h
- no recent head injury or active epilepsy
Etiology
- transient global amnesia is associated with dysfunction in the medial part of the temporal lobes, particularly the hippocampus, is observed
- the exact etiology and etiopathogenesis have not yet been clearly elucidated
- spreading depression or transient vasospasms are considered
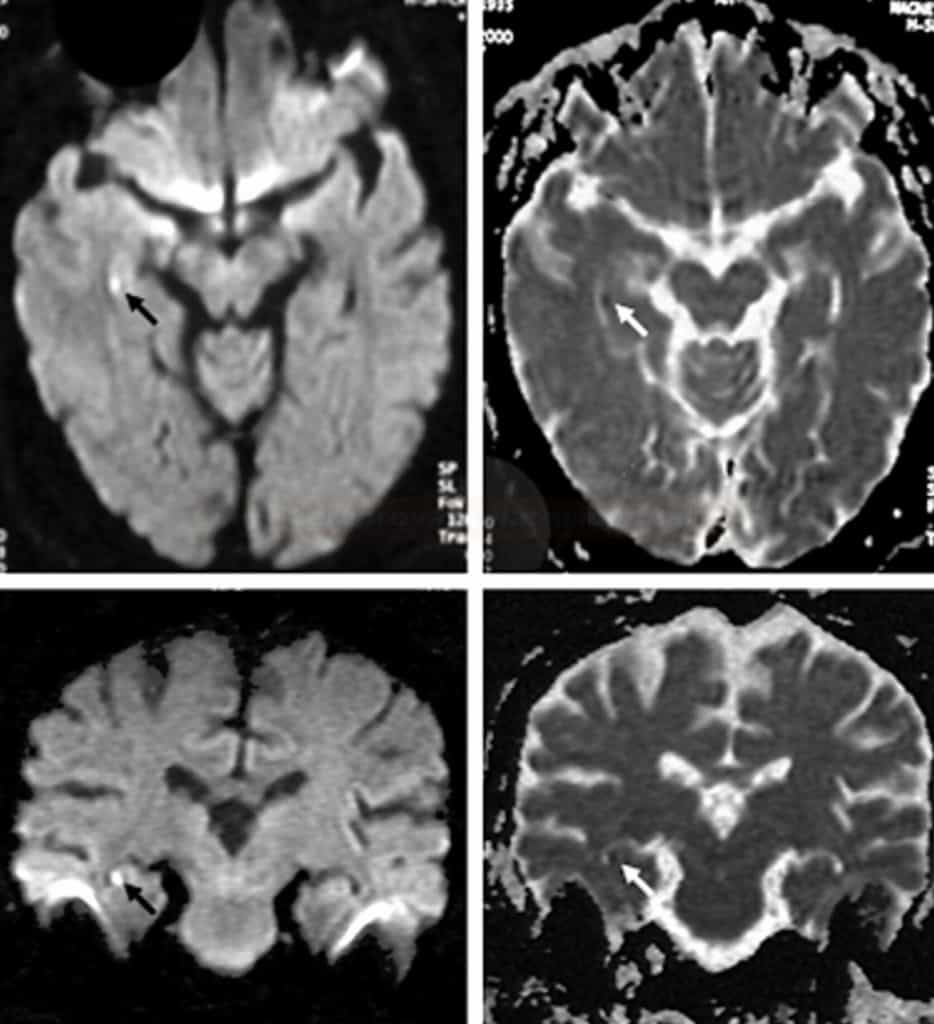
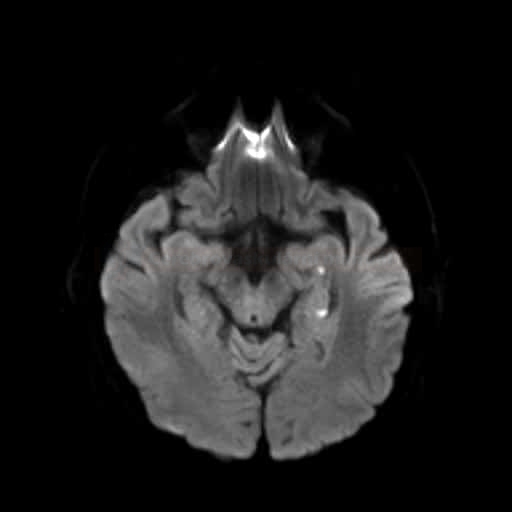
- inconsistent MR DWI findings highlight ambiguities regarding the etiology – some DWI studies yield negative results, while others show images resembling stroke [Bartsch, 2007]
- punctuate hyperintensity on DWI, hypointense on ADC map with normalization of ADC signal occurring within ten days
- however, it remains unclear whether these patients do not actually have TGA syndrome
- it is necessary to exclude TGA syndrome (stroke/TIA, epileptic seizure or nonconvulsive status epilepticus, and metabolic disorders)
Diagnostic evaluation
Differential diagnosis
- exclusion of TGA syndrome (stroke, epilepsy, and other stroke mimics)
- TGA is not associated with an increased risk of ischemic stroke [Mangla, 2013]
| Content available only for logged-in subscribers (registration will be available soon) |
Management
- no specific treatment is needed for true TGA
- supportive care includes ensuring patient safety, keeping the patient calm, and monitoring their vital signs
- treatment of TGA syndrome depends on its etiology (antiseizure medications, antiplatelet therapy, lifestyle modifications, etc.)
Follow-up
- patients who experience TGA should have temporary check-ups with a neurologist or general practitioner to monitor their condition