MEDICATION
Antiplatelet drugs
Updated on 06/07/2024, published on 02/12/2021
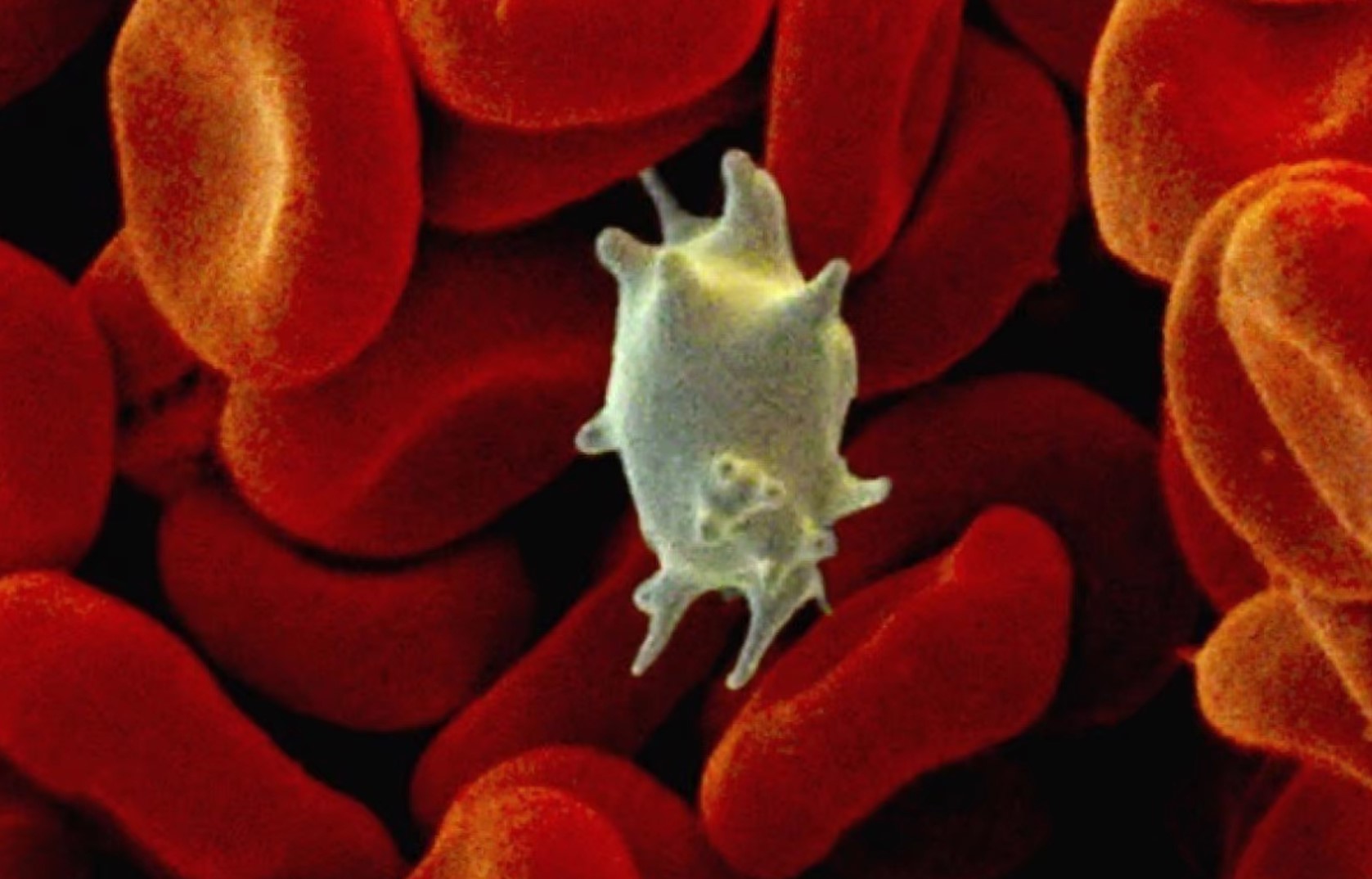
Thrombocytes (platelets)
- platelets are formed in the bone marrow from megakaryocytes. They have a round shape, irregular margins, and lack a nucleus
- typical lifespan ~ 9-12 days
- the normal range of platelet concentration is 150–450 × 109 /L (age and sex independent)
- 2/3 circulate within the bloodstream, while the remaining 1/3 resides in the spleen
- a drop in platelet count below the physiological limit is referred to as thrombocytopenia, whereas an increase is termed thrombocytosis
- platelets contain three types of granules
- alpha granules (containing von Willebrand factor-vWF, platelet factor 4, P-selectin, PDGF, fibrinogen, B-thromboglobulin, factors V and XIII)
- dense (delta) granules (containing ADP, ATP, Ca2+, serotonin)
- gamma granules (containing lysosomal enzymes)
- platelets play a crucial role in the process of atherothrombosis, contributing significantly to ischemic events (including coronary artery disease, cerebrovascular accidents, and peripheral arterial disease)
- long-term exposure to risk factors leads to pathological changes in the arterial wall, with atherosclerotic involvement being the most prominent
- plaque erosion or rupture stimulates platelets to aggregate, leading to thrombus formation
- thrombi can lead to vessel occlusion or serve as a source of embolization to peripheral branches (causing thromboembolism)
- long-term exposure to risk factors leads to pathological changes in the arterial wall, with atherosclerotic involvement being the most prominent
- antiplatelet drugs are an integral part of both primary and secondary cardiovascular prevention strategies
- the traditional designation of antiplatelet drugs as antiaggregants has been abandoned due to factual inaccuracy
- different antiplatelet drugs affect various phases of platelet activation, not limited to aggregation alone
- antiplatelet therapy is not aimed at reducing the number of platelets but rather at influencing their function (i.e., inhibiting any of the phases involved in white clot formation)
| Content available only for logged-in subscribers (registration will be available soon) |
Overview of antiplatelet agents, mechanism of action
- to achieve an effective blockade of primary hemostasis, over 70% of platelets need to be inhibited
- discontinuation of medication after long-term use, especially in secondary prevention, is associated with an increased risk of CV events (at a rate of 1.35% per year). Thus, 1 in 74 patients will have a CV event within a year after discontinuing the medication [Sundström,2017]
- adherence to antiplatelet treatment in the absence of major surgery or bleeding is an important treatment goal
| Content available only for logged-in subscribers (registration will be available soon) |
Inhibitors of cyclooxygenase
Acetylsalicylic acid (ANOPYRIN, GODASAL, STACYL, VASOPIRIN)
|
- aspirin irreversibly blocks the enzyme cyclooxygenase-1 (COX-1) inside platelets
- it represents the cornerstone of antiplatelet therapy, as confirmed by numerous studies.”
- the recommended daily dose is 50 – 325 mg
- higher doses yield no benefit and only increase the risk of side effects
- low doses (30-80 mg) have a cumulative effect, and TXA2 production is maximally reduced on days 4-5
- an antiplatelet effect (COX1 inhibition) can be achieved with a dose as low as 30 mg; higher doses are needed to inhibit COX2 (anti-inflammatory and analgesic effect)
- platelets cannot synthesize COX, so the drug’s effect lasts for the platelet lifetime (8-11 days)
- platelet activation can continue through other pathways
- the antiplatelet effect of aspirin varies among patients; its mediated inhibition of platelet aggregation is affected by inter- and intra-individual variability. Some patients are aspirin-resistant or develop this resistance during treatment (up to 40%)
- the most common side effects:
- GI bleeding (up to 55% higher than placebo); PPIs are recommended (there is a fixed combination of ASA+ omeprazole – YOSPRALA → see here
- risk factors: peptic ulcer with or without a history of bleeding, concomitant anticoagulation, or dual antiplatelet therapy (DAPT), age > 60 years, history of corticosteroid use, dyspepsia or gastroesophageal reflux
- risk factors: peptic ulcer with or without a history of bleeding, concomitant anticoagulation, or dual antiplatelet therapy (DAPT), age > 60 years, history of corticosteroid use, dyspepsia or gastroesophageal reflux
- increased risk of intracerebral hemorrhage, especially with dual antiplatelet therapy and when other factors are combined
- in the WARSS trial, the risk of major bleeding with ASA use was about 1.5%/year (with warfarin with INR 1.4-2.8) was 2.22%/year – HR 1.45, p=0.1)
- according to a study of nearly 186,000 patients on ASA (compared to the same number of patients without ASA), ASA use was associated with a 55% increase in the risk of ICH, which is more than initially expected. The median follow-up time was 5.7 years. The incidence of major bleeding was 5.58/1000 patients/year (ASA) vs. 3.6 (no ASA) – IRR 1.55 [JAMA 2012]
- GI bleeding (up to 55% higher than placebo); PPIs are recommended (there is a fixed combination of ASA+ omeprazole – YOSPRALA → see here
Aspirin + dipyridamole (AGGRENOX)
|
- the combination of aspirin 50 mg + controlled-release dipyridamole 200mg (ASA+DP), given twice daily, is more effective than ASA alone (annual risk reduction – ARR of 1.5%)
- ESPS2 (The European Stroke Prevention Study, 1996) reported an absolute annual risk reduction of 1.5% for ASA+DP compared to ASA alone (NNT/year 66)
- ESPRIT (European/Australasian Stroke Prevention in Reversible Ischaemia Trial, 2005) demonstrated an annual absolute risk reduction of 1% for ASA+DP vs. ASA
- headaches are a common problem with ASA+DP (especially when starting treatment)
Indobufen (IBUSTRIN)
|
- indications: cerebrovascular and cardiac ischemic disease, peripheral vascular disease of atherosclerotic nature, venous thrombosis, disorders of fat metabolism, and diabetes
- dose: 2 x 200 mg, dose reduction is necessary based on creatinine clearance):
- CrCl > 70 mL/min … 200 mg twice daily
- CrCl 30-80 mL/min … 100 mg twice daily
- CrCl <30 mL/min … 100 mg once daily
- indobufen is not mentioned in the AHA/ASA guidelines
- AEs: bleeding, GI difficulties, headache, impaired renal function, decrease in leukocytes and platelets
Inhibitors of P2Y receptors
Clopidogrel (TROMBEX, ZYLLT, EGITROMB)
|
| Content available only for logged-in subscribers (registration will be available soon) |
Ticlopidin (APO-TIC, TAGREN)
|
- a membrane ADP receptors-blocker
- recommended dose: 2 x 250 mg
- the onset of action of ticlopidine is gradual (within 6 h), reaching a maximum effect in ~ 6 days and persisting for 4-10 days after discontinuation
- the efficacy of ticlopidine has been demonstrated in the CATS and TASS trials
- the CATS (Canadian American Ticlopidine Study) demonstrated a 6.5% absolute risk reduction in cerebral infarction over 2 years compared to placebo (10.1% vs. 16.7%), with NNT/year of 30
- the TASS ( Ticlopidine Aspirin Stroke Study) study published in 1993 showed a 2.6% reduction in the absolute risk of fatal and non-fatal MI with ticlopidine compared to ASA (11.2 vs. 13.8%). The mean follow-up time was 2.3 years, with an NNT/year of 90.
- ticlopidine also has a lower resistance incidence compared to clopidogrel
- adverse events: neutropenia (severe in approximately 1% of cases), skin rash, and diarrhea (severe in 2% of patients); all reversible
- perform regular blood count checks during the first 3 months of treatment (first month each week, and subsequently every 14 days)
- ticlopidine has been largely replaced by clopidogrel in clinical practice
Prasugrel (EFIENT)
|
| Content available only for logged-in subscribers (registration will be available soon) |
Ticagrelor (BRILIQUE)
|
- a direct, reversible inhibitor of membrane ADP receptors (P2Y12)
- reversible – inhibition lasts as long as ticagrelor or its active metabolite circulates in the plasma
- direct – no need for bioactivation, ticagrelor provides a critical proportion of the pharmacodynamic effect
- because of its rapid binding (4 min) and rapid dissociation (10 min), ticagrelor’s effect directly depends on sufficient plasma concentration and rapidly dissipates after falling below therapeutic levels
- it is convenient when the antiplatelet effect needs to be discontinued
- when the dosing interval is prolonged, platelets regenerate, and the antithrombotic effect diminishes
- it is convenient when the antiplatelet effect needs to be discontinued
- at a dose of 2 x 90 mg daily, inhibition of >90% of platelets for 24 hours has been documented
- there is a faster onset of action and higher efficacy compared to clopidogrel
- a lower risk of resistance was reported – in a subgroup of patients with low CYP2C19 activity and high glycoprotein P activity who have a low treatment response to clopidogrel, the full effect of ticagrelor is maintained
- the drug should be avoided during pregnancy and lactation
- the recommended dose: 180 mg bolus initially, then 2 x 90 mg/d (the THALES and SOCRATES neurological studies used the combination of ticagrelor + 100 mg ASA)
- THALES trial showed the effect of dual antiplatelet therapy ticagrelor + ASA vs. ASA in patients with NIHSS 0-5; the benefit was also in NIHSS 4-5 (moderate stroke) group [Wang, 2021]
- adverse events:
- the overall incidence of major bleeding is the same as with CLP, with a somewhat higher proportion of fatal ICH [Wallentin, 2009]
- the most common AE is a higher incidence of asymptomatic atrioventricular blocks similar to all reversible P2Y12 receptor blockers (elinogrel, ticagrelor, cangrelor)
- ticagrelor is not recommended for patients with bradycardia, sick sinus syndrome, or AV block
- ticagrelor inhibits cellular adenosine uptake, which can lead to effects like the sensation of dyspnea
- creatinine levels and uric acid levels may increase
- a total of 11,016 patients underwent randomization (5523 in the ticagrelor–aspirin group and 5493 in the aspirin group)
- these patients had experienced TIA or mild stroke (NIHSS score ≤5) of noncardioembolic etiology and were not undergoing IVT or endovascular treatment
- the treatment regimens: ASA+ticagrelor (loading dose 180 mg, then 2x 90 mg daily) vs. ASA alone (loading 300 mg, then 100 mg/d)
- a primary-outcome event (stroke or death) within 30 days: 303 (5.5% ASA+ticagrelor) vs. 362 (6.6% – aspirin group)
- severe bleeding: 28 (0.5%) vs 7 (0.1% aspirin group)
- the risk of the composite of stroke or death within 30 days was lower with ticagrelor–aspirin than with aspirin alone, but the incidence of disability did not differ significantly between the two groups [Johnston, 2020]
- this effect was also observed in patients with NIHSS 4-5 (moderate stroke) [Wang, 2021]
- sub-analysis showed higher efficacy in patients with ipsilateral atherosclerotic involvement (stenosis ≥ 30%) [Amarenco, 2020]
- primary endpoint at 30 days: in the presence of stenosis 8.1% (ticagrelor+ASA) vs. 10.9% (ASA), NNT 34, for patients without stenosis 4.8% vs. 5.4%
- in patients with recent stroke/TIA, the trial did not demonstrate superior efficacy of ticagrelor over ASA → see here
- the initial bolus consisted of ASA 300/ticagrelor 180 mg, followed by ASA 100mg/ticagrelor 2x90mg
- primary endpoint: ticagrelor 442/ 6589 patients (6.7%), ASA 497/ 6610 (7.5%), hazard ratio 0.89)
- main secondary endpoint – ischemic stroke – 5.8% (ticagrelor) vs 6.7% (ASA), hazard ratio, 0.87)
- no benefit of ticagrelor was demonstrated in patients who were already taking ASA before the qualifying stroke
- according to subanalysis, ticagrelor appears to be more effective than ASA in the subgroup of patients with atherosclerotic stenosis ≥ 50% (6.7 vs. 9.6%) [Amarenco, 2017]
- according to the PRINCE trial, the combination of ASA + ticagrelor appears to be better than ASA + CLP (as indicated by laboratory resistance tests)
- fewer laboratory-detected resistances were observed (12.5% vs. 29.7%), and in patients with dysfunctional CYP2C19 alleles, the difference was even more significant (10.8% vs. 35.4%
- phase III trial should assess the clinical significance
Elinogrel
|
- non-thienopyridine reversible ADP P2Y12 receptor blocker
- the advantage is the possibility of parenteral administration ensuring a rapid onset and short duration of action [Angiolillo, 2012]
- available in peroral and parenteral forms
- used exclusively in cardiology thus far
Cangrelor (KENGREXAL)
|
- a non-thienopyridine ADP P2Y12 receptor antagonist with direct and reversible action
- it has the advantage of a rapid onset of action (within minutes) but has a short half-life (5 minutes); therefore, continuous parenteral administration is required, and use is limited to the bridging treatment of ACS
- pre-treatment platelet aggregation levels are achieved within 30–60 minutes
Others
Cilostazol
|
- acts through selective inhibition of phosphodiesterase (PDE) type III ⇒ increases the cyclic adenosine monophosphate (AMP) levels in platelets
- although it has an antiplatelet effect, it is usually administered in combination with aspirin or clopidogrel in patients with intermittent claudication due to PAD
- cilostazol 100 mg twice daily reduced the risk of serious vascular events and the risk of recurrent ischemic stroke (Gotoh, 2000)
- in Asian countries, cilostazol has been used in addition to dual antiplatelet therapy in patients receiving coronary stents and as an alternative to aspirin in patients with ischemic stroke (↓ risk of bleeding)
- common side effects: headache, palpitations and diarrhea