ISCHEMIC STROKE
Ischemic penumbra
Updated on 24/04/2024, published on 20/06/2023
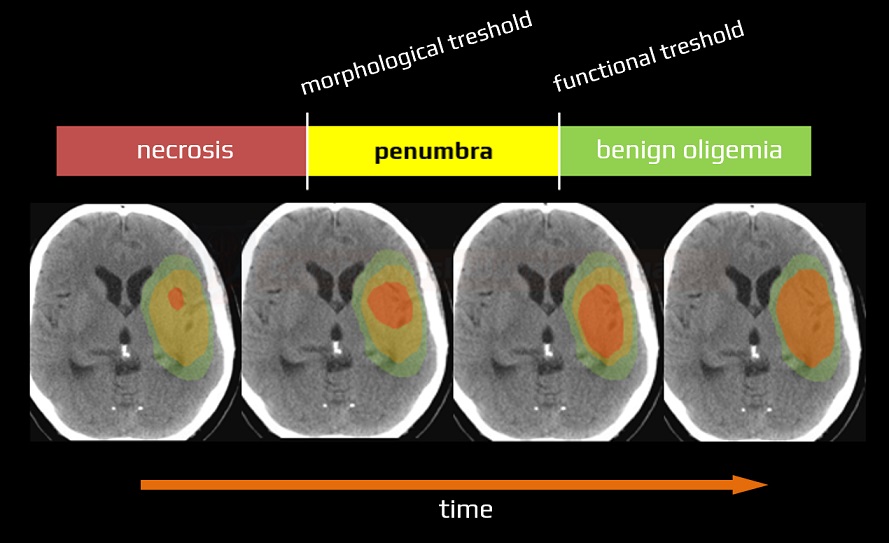
Concept of ischemic penumbra
- the extent of brain damage during a stroke depends on the severity and duration of the cerebral blood flow (CBF) disorder → Regulation of cerebral blood flow
- within the ischemic area, two major zones of injury are identified :
- core
- penumbra
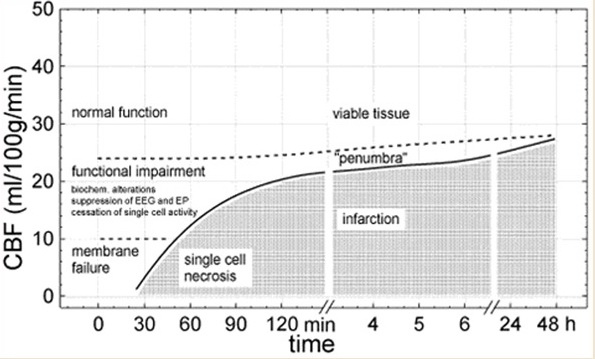
- as blood flow decreases, an initial loss of function occurs while structural integrity remains intact (functional threshold)
- with a further decrease in CBF or prolonged blood flow deficit, irreversible loss of membrane functions and permanent morphologic changes occur (morphologic threshold)
- a decrease in regional flow to < 55 mL / 100g of tissue/minute leads to inhibition of proteosynthesis
- < 35 mL – stimulation of anaerobic glycolysis begins
- < 20 mL – loss of electrical function occurs
- < 10 – 12 mL – necrosis
- neurons in areas where CBF falls below the morphologic threshold (infarct core) represent tissue that is already dead or only viable for a very limited time
- brain tissue with perfusion values between the two thresholds (CBF 12-18 ml/100g/min) is termed the “ischemic penumbra“; this tissue may remain viable for several hours
- without early reperfusion, cells in the penumbra will eventually die, as collateral circulation cannot sustain the neuronal demand for oxygen and glucose indefinitely ⇒ penumbra shrinks with prolonged arterial occlusion
- neurons of the hippocampus, basal ganglia, and some cortical areas are particularly vulnerable
- identifying and quantifying the penumbra can guide clinical decisions, as rescuing neurons in the ischemic penumbra is the primary objective of recanalization therapy
| core | penumbra | normal tissue |
|
|
CBF mL/100g/min
|
< 12
|
12-18
|
> 18
|
|
EEG
|
0
|
reduced
|
normal
|
|
SSEP
|
0
|
reduced
|
preserved
|
|
histology
|
infarction
|
normal |
normal
|
|
membrane potential
|
0
|
0 (reversible)
loss of neuron function |
normal
|
|
vitality
|
no
|
preserved
|
normal
|
Penumbra detection
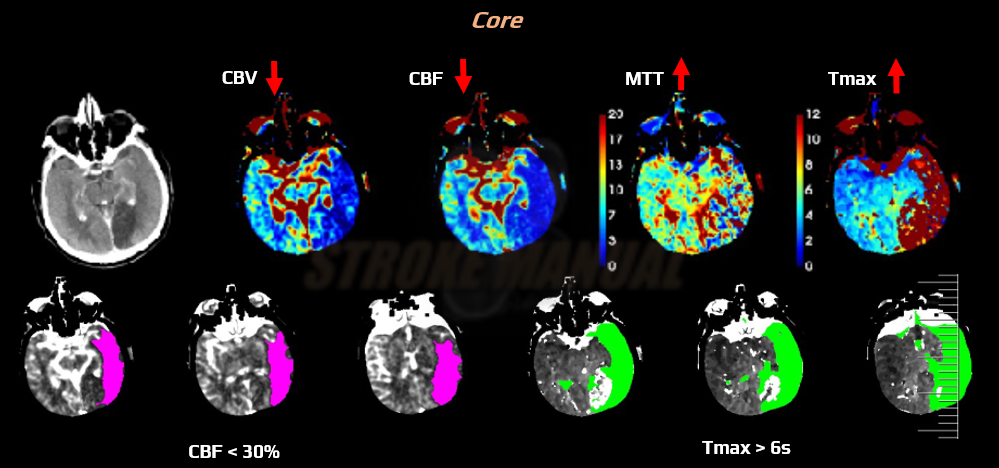
CT perfusion (CTP)
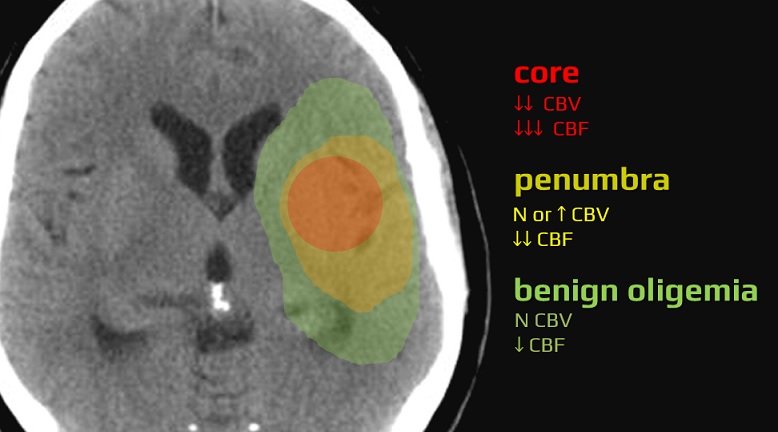
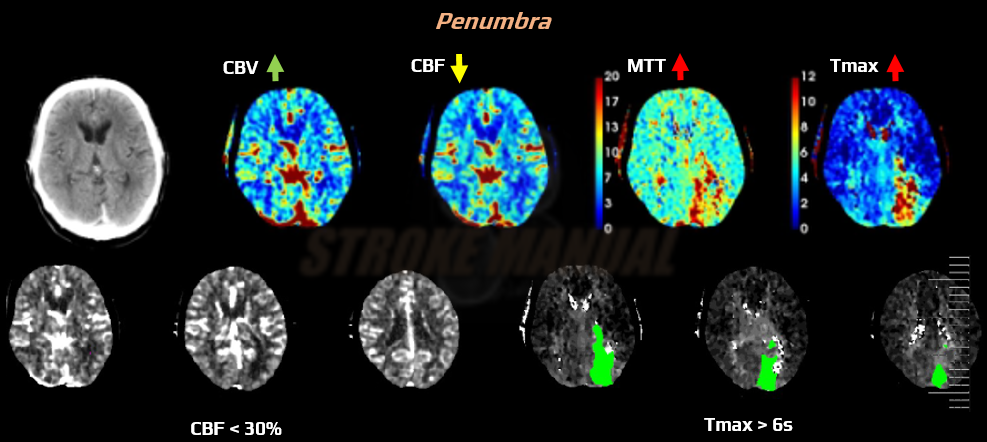
- CT perfusion (CTP) can help differentiate between irreversible ischemia (core) and ischemic penumbra (viable tissue with reduced perfusion), as well as benign oligemia
- software packages use various combinations of parameters to define core and penumbra
- a common definition of penumbra:
- hypoperfused brain at risk of progression to infarction, yet salvageable
- increased T-max >6 seconds, or mean transit time (MTT) or time to peak (TTP) > 145% of the healthy hemisphere
- moderate decrease of cerebral blood flow (CBF); > 30% compared to the contralateral (normal) side
- normal or ↑ cerebral blood volume (CBV) – due to autoregulation
- a common definition of core:
|
CBV
|
CBF
|
MTT
|
|
|
ischemic core
|
↓↓
|
↓↓↓
(< 30%) |
↑↑
|
|
penumbra
|
N or ↑
|
↓↓
(> 30%) |
↑↑
|
|
benign oligemia
|
N or ↑
|
↓
|
↑ or ↑↑
|
|
chronic, compensated occlusion/stenosis
|
N
|
N
|
↑ or ↑↑
|
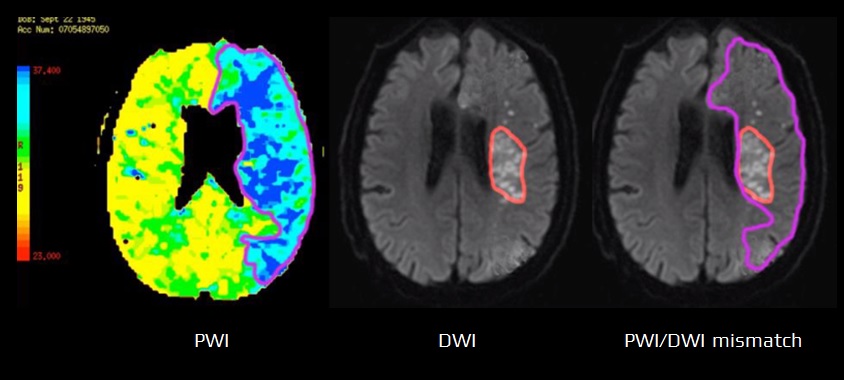
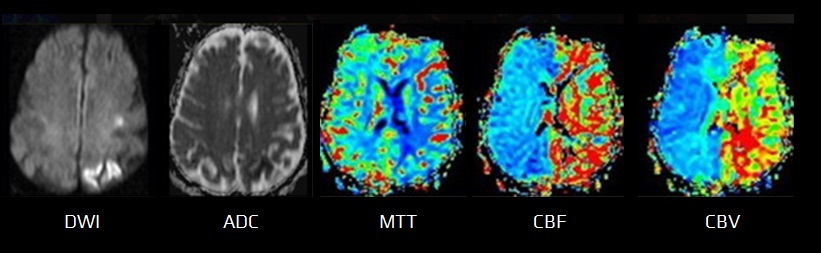
MR perfusion (PWI)
- MR perfusion imaging (PWI) uses the “first-pass bolus” technique, utilizing intravenous gadolinium
- the same parameters as with CTP can be obtained (CBV, CBF, MTT, TTP)
- tissue with reduced blood flow (indicated by a prolonged MTT) encompasses:
- infarct (core)
- penumbra
- benign oligemia regions
- infarct (core)
- the ischemic core closely correlates with restricted diffusion lesion (DWI lesion) and is characterized by decreased CBF and CBV
- the difference between the tissue volume showing a perfusion deficit (on PWI) and the tissue volume already infarcted (on DWI) is termed the PWI/DWI mismatch
- PWI/DWI mismatch represents the ischemic penumbra
FAQs
- the ischemic penumbra refers to brain tissue that is hypoperfused due to an ischemic stroke but remains potentially salvageable if blood flow is restored promptly
- penumbra is typically identified using imaging techniques such as CT perfusion or MRI diffusion and perfusion studies
- these techniques help to differentiate the penumbra from the infarct core by showing areas of reduced blood flow that have not yet been irreversibly damaged
- reperfusion therapies such as intravenous thrombolysis (using alteplase or tenecteplase) and mechanical thrombectomy (endovascular removal of the clot)
- these treatments aim to restore blood flow to the penumbra as quickly as possible
- the survival time of the ischemic penumbra can vary significantly among individuals, generally ranging from tens of minutes to several hours post-stroke
- the exact duration depends on various factors, including the severity of the blood flow reduction and the presence of collateral blood vessels
- it depends on how quickly reperfusion therapy is administered and reperfusion established
- early and effective treatment increases the likelihood of saving most, if not all, of the penumbral tissue
- if the ischemic penumbra is not treated promptly, it is likely to undergo irreversible damage and become part of the infarcted core