ADDONS / GENERAL NEUROLOGY
Tinnitus
Updated on 15/05/2024, published on 29/02/2024
- tinnitus = perception of sound within the head or ears
- in most cases, subjective tinnitus is characterized by sound perception in the absence of an external auditory stimulus (only audible to the individual experiencing it)
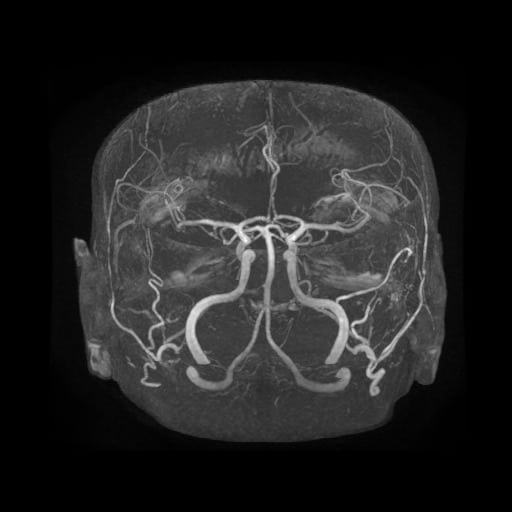
- objective tinnitus tends to occur in vascular pathologies (e.g., AV shunt/stenosis/aneurysm with pulsatile tinnitus) where the murmur can be heard through auscultation of the head
- acute x chronic (> 6 months)
- tinnitus is not a disease per se but a symptom caused by a variety of causes
- it is reported by patients as hissing, buzzing, humming (low or high frequency) and can be of varying intensity
- it is present either constantly or intermittently (e.g., at rest, during physical exertion, due to changes in barometric pressure, etc.)
- patients typically perceive tinnitus in the evening when trying to fall asleep
- it can be localized either directly to the ear (unilaterally or bilaterally), or it may be perceived diffusely in the head
- in some patients, it may be associated with hyperacusis (reduced tolerance to sound)
- chronic severe tinnitus can interfere with sleep and psychological well-being, causing mood changes, anxiety, difficulty concentrating, and insomnia
- tinnitus can be caused by a variety of factors (see below); tinnitus without an identifiable cause is called idiopathic tinnitus
- from a vascular perspective, tinnitus (usually pulsatile) is most commonly caused by DAVF, CC fistula, or, less frequently, as a result of significant arterial stenosis or rare pathologies in the intracranial venous system
Clinical presentation
Tinnitus characteristics
- duration: continuous x intermittent? only at bedtime?
- varying intensity?
- synchronous with a heartbeat (pulsatile tinnitus)?
- lateralization: unilateral x bilateral x diffuse
- dependence on physical activity: yes – no
- any relieving maneuvers? (e.g., external compression on the neck, specific head or body position)
- history of (baro)trauma?
- is the quality of life affected?
- sleep disturbance, anxiety, depression, difficulty concentrating, irritability, and decreased work or social functioning
Associated symptoms
- hearing loss
- conductive – results from obstruction or damage to the outer or middle ear that prevents sound from being conducted to the inner ear. Causes include ear infections, fluid in the middle ear, earwax buildup, perforation of the tympanic membrane, and ossicular chain abnormalities
- sensorineural hearing loss (SNHL) – arises from damage to the inner ear (cochlea) or the auditory nerve, impairing the transmission of auditory signals to the brain. Common causes include aging (presbycusis), noise exposure, ototoxic medications, genetic factors, and various diseases
- mixed hearing loss
- ear pain or fullness
- vertigo
- headaches
- focal neurological signs (incl. cranial neuropathy)
Diagnostic evaluation
The diagnostic evaluation of tinnitus should be individualized based on the patient’s clinical presentation, medical history, and specific concerns, to identify treatable causes and implement appropriate management strategies. Collaboration with otolaryngologists, audiologists, and other healthcare professionals may be necessary for a comprehensive evaluation and management plan.
Personal history
- noise exposure – a history of exposure to loud noises, such as occupational or recreational activities
- medical history – underlying medical conditions that may contribute to tinnitus, such as hypertension, diabetes, cardiovascular disease, neurological disorders, or autoimmune conditions
- medication history – medications, including prescription, over-the-counter, and herbal supplements
- otologic history – any history of ear infections, ear surgery, trauma, or earwax impaction
- psychosocial history – any psychosocial factors that may influence tinnitus perception, such as stress, anxiety, depression, or significant life events
- lifestyle factors – smoking, alcohol consumption, caffeine intake, and recreational drug use may impact tinnitus perception or exacerbate symptoms
Diagnostic methods
- physical examination with particular attention to the head, neck, and ears; assess for signs of ENT conditions, vascular abnormalities, temporomandibular joint dysfunction, and neurological deficits
- examination by an ENT specialist incl. audiological assessment
- tinnitus assessment – specialized techniques to match the pitch and loudness of the patient’s tinnitus
- tinnitus assessment – specialized techniques to match the pitch and loudness of the patient’s tinnitus
- BAEP (abnormal in, e.g., CN VIII neurinoma)
- BAEP stands for Brainstem Auditory Evoked Potentials, also known as Brainstem Auditory Evoked Responses (BAER) or Auditory Brainstem Response (ABR)
- BAEP is a diagnostic test used to assess the function of the auditory pathways from the inner ear to the brainstem
- imaging studies (parenchymal and vascular) using CT or MRI
- DDx – vascular malformation, tumor, or inflammation in the cerebellopontine angle or middle ear
- neurosonology
- auscultation of the head (mainly audible in pulsatile tinnitus caused by AV shunt or stenosis)
- C-spine and temporomandibular joint x-ray
- psychological assessment
Etiology
- idiopathic tinnitus (cause not found despite extensive diagnostic efforts)
- ENT disorders
- external ear canal inflammation, otitis media, cholesteatoma, tympanic membrane perforation
- earwax (cerumen) obstructing the ear canal
- age-related hearing loss associated with tinnitus
- noise-induced hearing damage
- Menier’s disease
- episodes of vertigo, fluctuating hearing loss, ear fullness, and tinnitus
- hearing damage caused by ototoxic drugs (some antibiotics, antidepressants, chemotherapy drugs)
- neurological diseases
- dural AV fistula, carotid-cavernous fistula, arterial stenosis, (pseudo)aneurysm (hearing is not impaired) – usually objective, audible tinnitus
- multiple sclerosis
- head and neck injuries
- acoustic neurinoma, external compression of CN VIII by meningioma, etc.
- neurovascular conflict
- glomus tumors (tympanicum or jugulare)
- others
- psychiatric illnesses
- Lyme borreliosis
- cervical spine disorders
- temporomandibular joint dysfunction (physiotherapy may help)
- due to referred muscle tension affecting the ear structures
| Causes of pulsatile tinnitus |
|
- analgesics (aspirin, non-steroidal antirheumatic drugs) – cochlear toxicity manifested by tinnitus and hearing loss
- antibiotics (aminoglycosides, chloramphenicol, erythromycin, tetracycline)
- gentamicin and other aminoglycosides (tobramycin, amikacin) irreversibly damage the hair cells of the labyrinth. Vestibular toxicity, especially with gentamicin or streptomycin, may precede cochlear damage or nephrotoxicity.
- vestibular and auditory lesions are irreversible
- gentamicin and other aminoglycosides (tobramycin, amikacin) irreversibly damage the hair cells of the labyrinth. Vestibular toxicity, especially with gentamicin or streptomycin, may precede cochlear damage or nephrotoxicity.
- chemotherapeutics and antiviral agents (bleomycin, interferon, cisplatin, methotrexate)
- cisplatin toxicity may cause high-frequency sensorineural hearing loss and tinnitus and may also cause vestibulopathy; vestibular or auditory lesion is irreversible
- diuretics (furosemide) – cochlear toxicity, manifesting as tinnitus and hearing loss
- others
- chloroquine
- quinine
- psychedelic substances
- industrial solvents – may cause bilateral vestibular disorder (benzene, toluene, xylene, aniline)
- tinnitus is a fairly common condition experienced by many pregnant women
- the exact reasons why tinnitus occurs during pregnancy aren’t fully understood; various factors are likely involved:
- hormonal changes
- increased blood volume and hypertension
- in some cases, tinnitus during pregnancy may be an early sign of gestational hypertension or preeclampsia
- anemia
- changes in earwax production
- pre-existing ear conditions such as otosclerosis or Meniere’s disease can be aggravated during pregnancy
Management
- therapy is often individualized based on the patient’s specific needs and may involve a multidisciplinary approach (otolaryngologists, audiologists, psychologists, and other healthcare professionals)
- the goal of treatment is to eliminate the tinnitus (by causal therapy if possible) or to help patients alleviate the symptoms and improve their quality of life
Causal therapy
- treatment of ENT diseases
- surgery of neurinoma n.VIII
- DAVF or CCF embolization
- management of temporomandibular joint dysfunction, etc.
Symptomatic therapy
Symptomatic therapy aims to alleviate the symptoms of tinnitus and improve the patient’s quality of life
- hearing aids
- for patients with coexisting hearing loss
- hearing aids can help improve overall hearing function and reduce the perception of tinnitus by amplifying external sounds
- amplification of environmental sounds can also make tinnitus less noticeable
- sound therapy
- external sound generator (tinnitus masker) – sends specially tuned sounds to mask or distract from the perception of tinnitus
- can be worn as a hearing aid
- Tinnitus Retraining Therapy (TRT)
- patients learn to consciously “ignore” the disturbing sounds (through habituation)
- TRT focuses on changing the patient’s response to tinnitus rather than eliminating the sound itself
- cognitive behavioral therapy (CBT)
- helps patients reframe negative thoughts and emotions associated with tinnitus and develop coping strategies to manage distress
- CBT techniques may include relaxation techniques, stress management, and cognitive restructuring
- lifestyle modifications
- regular exercise, proper diet
- adequate sleep
- avoidance of excessive noise, salt, caffeine, and nicotine
- medication (there is no specific medication approved for the treatment of tinnitus)
- antidepressants
- anxiolytics
- hypnotics
- vitamin B complex and substances that improve microcirculation (vasodilators, ginkgo biloba) – especially for acute tinnitus
- alternative therapies
- acupuncture, hypnosis, biofeedback, or herbal supplements – the effectiveness of these approaches is limited