NEUROIMAGING / MAGNETIC RESONANCE
MR-DWI in the acute stroke diagnosis
Updated on 01/06/2024, published on 24/05/2021
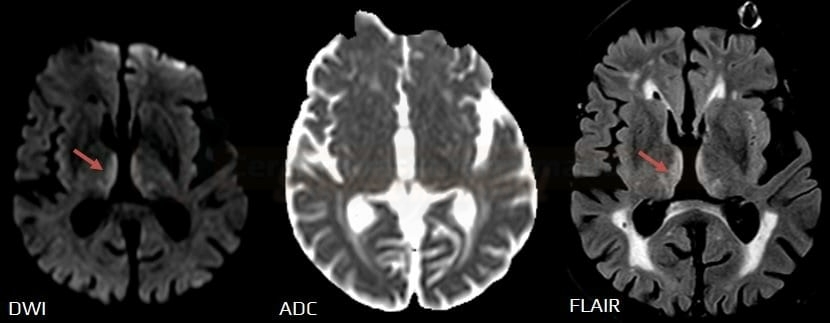
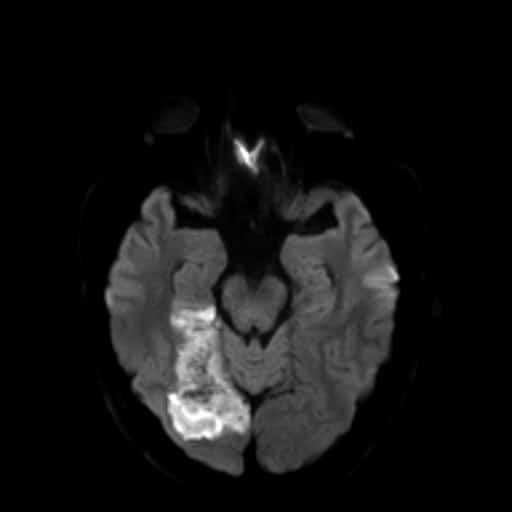
Diffusion-weighted imaging (DWI) is a common MRI sequence used to evaluate acute ischemic stroke. Increased DWI signal in ischemic brain tissue is usually observed within minutes of arterial occlusion.
Technical notes
- ischemia leads to diffusion restriction due to the energetic failure of Na+/K+ membrane pumps, causing water molecules to remain inside the cells
- the intensity of each voxel on the Diffusion-Weighted Imaging (DWI) sequence reflects the degree of water diffusion ⇒ restricted diffusion on DWI serves as a sensitive indicator of acute ischemia
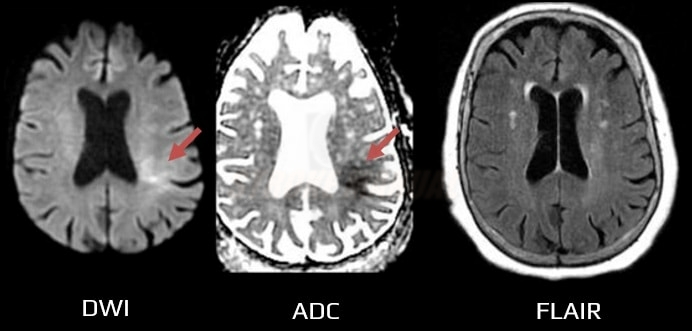
- acute lesions with restricted diffusion are hyperintense on DWI and hypointense on the Apparent Diffusion Coefficient (ADC) map (the lower the value, the greater the restriction)
- CT or conventional MRI sequences (T1, T2) may not reveal the lesion in the first hours after the stroke onset
- acute lesions with restricted diffusion are hyperintense on DWI and hypointense on the Apparent Diffusion Coefficient (ADC) map (the lower the value, the greater the restriction)
- DWI is acquired within 2 minutes and is less susceptible to motion artifacts compared to other sequences
- the diffusion defect is not stroke-specific and has been described in various neurological disorders (refer to the table below)
- always assess all MRI sequences (DWI, ADC map, T1, T2) and exclude artifacts (e.g., T2 shine-through phenomenon)
- when evaluating DWI images, consider the following aspects:
- location and shape of the lesion (does it correspond to a specific vascular territory?)
- is the DWI lesion hyperintense diffusely, centrally, or peripherally?
- does a bright signal on DWI correspond to a dark signal on the ADC map?
- isolated or multifocal lesion? (multiple territories x symmetric or even diffuse involvement?)
- presence of edema on T2/FLAIR images? – typically observed in the tumors and abscesses
- post-contrast enhancement on T1C+ sequences?
| Adult | Children |
|
DWI in acute stroke
- DWI visualizes impaired (restricted) diffusion of water molecules (or protons) caused by the energetic failure of Na+/K+ membrane pumps
- it is highly sensitive and specific (88-100%) for detecting acute cerebral infarction within minutes of onset, with a maximum of 4-6 hours
- acute ischemia is hyperintense (bright) on DWI (b factor around 1000 s/mm2) and hypointense (dark) on calculated ADC maps
- the extent of the DWI lesion in acute stroke approximately corresponds to the size of the tissue likely to be irreversibly affected
- however, the reversibility of DWI changes (early DWI reversal) following early reperfusion has been repeatedly documented
- however, the reversibility of DWI changes (early DWI reversal) following early reperfusion has been repeatedly documented
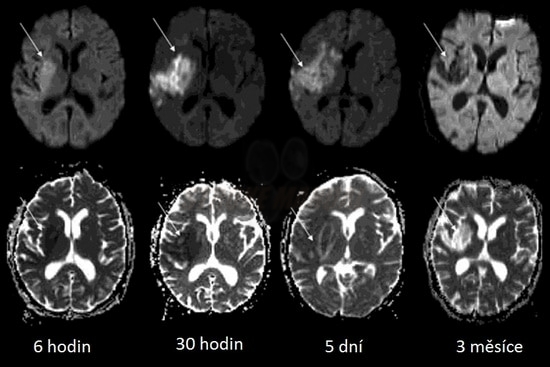
- DWI allows the differentiation of acute, subacute, and chronic lesions
- initially bright DWI signal decreases within a few days to become hypointense in later stages
- low signal on the ADC map increases during the subacute stage, with temporal pseudo-normalization of the ADC map occurring in the second week; in the chronic stage, ADC values remain increased
- initially bright DWI signal decreases within a few days to become hypointense in later stages
- DWI allows for the assessment of ischemic penumbra (demonstrated by DWI/FLAIR or DWI/PWI mismatch)
- DWI changes are not specific to ischemia; they can occur in any transport disorder (e.g., edema). Such changes are often reversible, and lesions are not hypointense on the ADC map (refer to the table above)
| Acute (0-7 days) |
|
| Subacute (7-21 days) |
|
| Chronic ( >3 weeks) |
|
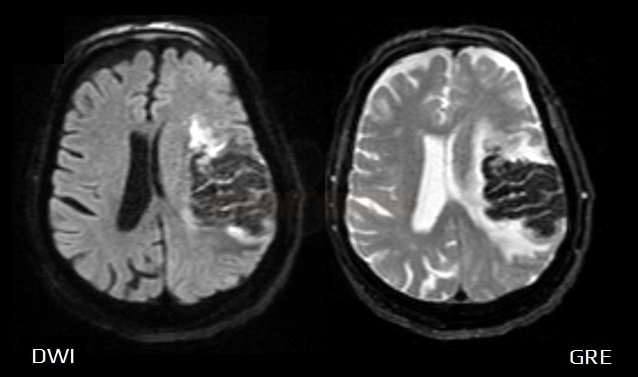
- DWI is inherently T2-weighted; T2 changes may influence the appearance of DWI independent of tissue diffusibility, causing artifacts
- increased T2 signal can lead to T2 shine-through and T2 washout
- decreased T2 signal leads to the T2 blackout phenomenon (hypointense area on DWI)
- e.g., iron deposition, bleeding
- infections (abscess, toxoplasmosis, aspergillosis)
- certain metastases
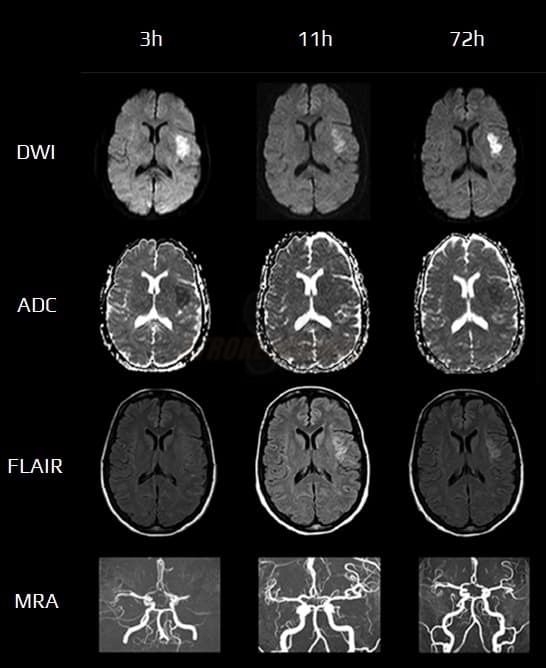
DWI/FLAIR mismatch (DFM)
- a positive DWI with negative findings on FLAIR indicates that the stroke probably occurred within the previous 4.5 hours [Aoki, 2010] [Thomalla, 2009]
- may be useful to guide intravenous thrombolysis (IVT) in patients with stroke of unknown onset or wake-up stroke (WUS)
-
- DWI/FLAIR mismatch is present (DWI positive in <1/3 of the MCA territory, FLAIR still negative)
- n=503 ( 254 tPA vs. 249 placebo), median NIHSS 6
- good outcome 53.3 vs. 41.8 (placebo), median mRS/3m 1 vs. 2
- mortality 4.1% vs. 1.2% (placebo)
- sICH 2% vs. 0.4% (placebo)
- MR WITNESS
- DWI/FLAIR mismatch (DWI positive in <1/3 of the MCA territory, FLAIR either negative or showing only minimal lesion)
- IVT administered within 4.5 hours of symptom onset
- n = 80, sICH 1.25% (as defined by ECASS III)
DWI/PWI mismatch
- Perfusion-weighted imaging (PWI) quantifies the concentration of gadolinium as it passes through the cerebral microcirculation
- colored maps are generated representing MTT, TTP, CBF, and CBV; these values are relative to the contralateral (healthy) side
- noninvasive techniques using Blood Oxygen Level-Dependent (BOLD) or Arterial Spin Labeling (ASL) are much less commonly used
- colored maps are generated representing MTT, TTP, CBF, and CBV; these values are relative to the contralateral (healthy) side
- the ischemic penumbra is characterized by the perfusion-diffusion (PWI-DWI) mismatch
- the DWI lesion represents the ischemic core; the remainder of the PWI lesion (with a TTP delay > 4s) is a probable penumbra (more likely a combination of penumbra and benign oligemia)
- the core may expand to reach the size of the baseline PWI lesion unless early reperfusion is achieved
- DWI lesions may exhibit some degree of reversibility (normalization x pseudonormalization)
- major recanalization trials using advanced imaging have used CT perfusion; no such robust data are available for DWI/PWI mismatch yet
ADC pseudonormalization
| Content available only for logged-in subscribers (registration will be available soon) |
Early DWI reversal
- the phenomenon occurs in the early phase of stroke, specifically during successful reperfusion within 3-6 hours after stroke onset [Pham, 2015]
- true regression is relatively rare; more commonly observed are DWI pseudonormalization (fluctuation) or partial regression
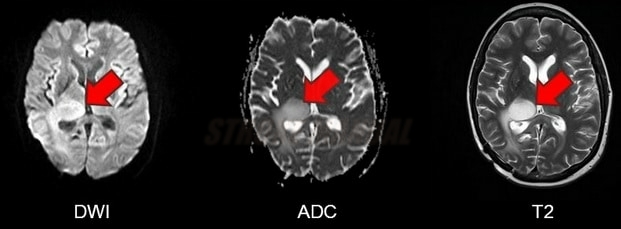
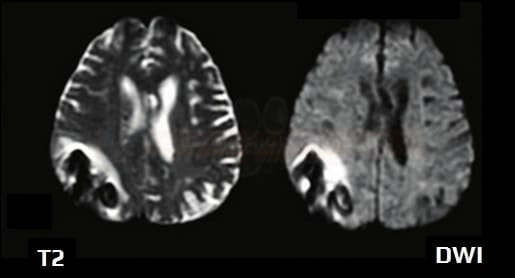
T2 shine-through
- falsely increased signal on DWI, that is not attributable to diffusion restriction but rather to the shining through of the T2 prolongation (commonly observed in subacute to chronic infarction)
- T2 and ADC maps should be evaluated simultaneously
- ADC is decreased in acute ischemia
- ADC is either normal or increased in T2 shine-through
T2 washout
- present in the subacute phase of ischemic stroke (between days 10-15) or in tumors accompanied by collateral vasogenic edema [Hiwatashi, 2003]
- normal-appearing DWI (b = 1000) despite abnormal ADC maps
- prolonged (hyperintense) T2, causing T2 shine through, is counterbalanced by higher ADC values ⇒ normal-appearing DWI [Casey, 2001]
- DDx:
- early DWI reversal – typically appears 3-6 hours post-stroke
- ADC pseudonormalization – occurs around day 7 post-stroke
- beyond stroke, the T2-washout phenomenon can also be observed in Posterior reversible encephalopathy syndrome (PRES)
- isointense lesions result from a balance of T2 effects and increased water diffusibility (Provenzale, 2001)
T2 blackout
- the actual DWI signal (determined by ADC values) is reduced due to the presence of a low (hypointense) T2 signal ⇒ DWI appears hypointense (dark)
- the T2 blackout phenomenon is present in conditions such as hematomas, degenerative diseases with iron accumulation, etc.
- T2 blackout is mainly caused by susceptibility effects