ISCHEMIC STROKE / CLASSIFICATION
Chinese Ischemic Stroke Subclassification (CISS)
Updated on 05/11/2023, published on 12/04/2022
- classification of an acute ischemic stroke has a significant impact on patient care, secondary stroke prevention, and stroke research
- the most popular and widely used stroke classification system is the TOAST
- other established systems include:
- A–S–C–O classification (Amarenco, 2009)
- SSS-TOAST (Ay, 2005)
- Chinese Ischemic Stroke Subclassification (CISS) attempts to improve TOAST by subclassifying strokes with greater accuracy; CISS has the following notable differences (Gao, 2011) :
- aortic arch atherosclerosis is assigned to LAA
- CISS differentiates underlying mechanisms associated with LAA
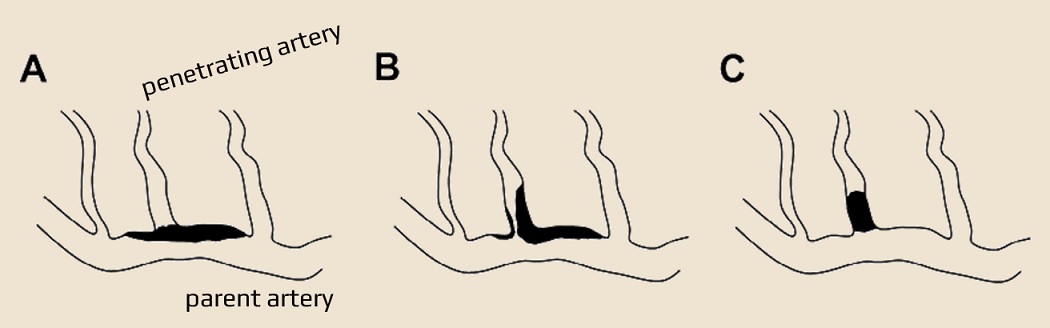
- CISS applies a new concept of penetrating artery disease – atheromatosis at the junction of the parent vessel (branch artery disease) and penetrating arteries vs. fibrohyalinosis
- intracranial atheromatous branch artery disease (BAD) affecting the penetrating arteries is classified as large artery atherosclerosis (LAA)
- new imaging technologies allow visualization of the previously invisible underlying pathologies and ambiguous lesions
Aortic arch atherosclerosis
- (multiple) infarcts, commonly involving bilateral anterior and/or posterior circulation
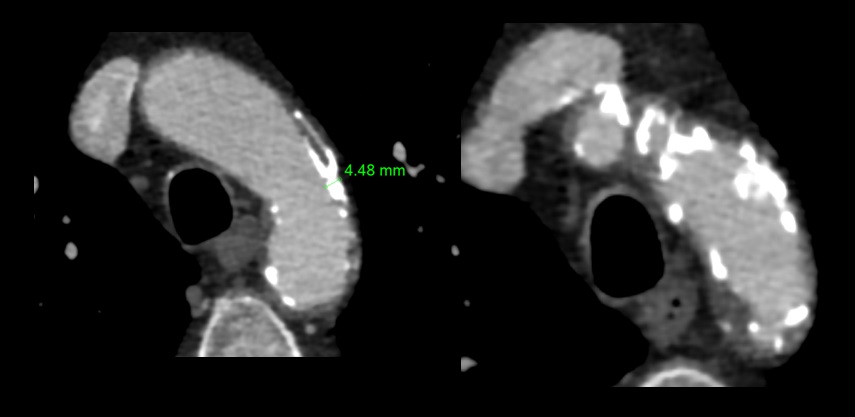
- evidence of significant aortic arch atherosclerosis – aortic plaques >4 mm and/or aortic thrombi (detected by HR-MRI/MRA and/or TEE)
- no evidence of atherosclerosis of relevant intracranial or extracranial large arteries (vulnerable plaques or stenosis ≥50% or occlusion)
- no evidence of a potential cause of cardiogenic stroke (CS) or other etiologies that could cause multifocal acute ischemic lesions
Intra- and extracranial LAA
- any distribution of acute infarction (except isolated stroke in the territory of a penetrating artery), with evidence of atherosclerosis involving intracranial or extracranial large arteries (vulnerable plaque or stenosis ≥50%) supplying the infarct territory
- infarcts in the territory of a penetrating artery may be included if the atherosclerotic plaque is detected in the parent artery (by HR-MRI)
- no evidence of potential cardioembolism or other obvious cause of stroke
The underlying mechanisms of ischemic stroke caused by intra- or extracranial LAA are further defined as:
- artery-to-artery embolism:
- small cortical infarcts or a single territory infarct in the area supplied by the relevant intra-/extracranial artery affected by atherosclerosis
- no border-zone infarct (BZI) associated with this artery
- diagnosis is confirmed if the infarcts are multiple or if the single infarct is accompanied by MES on TCD
- however, a single cortical or territory infarct without obtaining MES can also be diagnosed as an artery-to-artery embolism
-
hypoperfusion/impaired emboli clearance
-
infarcts occur in the border zone
-
no acute cortical or territory infarcts related to the diseased artery
-
stenosis of the clinically relevant intracranial or extracranial artery is usually >70%, with or without evidence of hypoperfusion or poor collateral compensation in the related region of perfusion
- perfusion may be compromised by a sudden drop in blood pressure or other systemic hypoperfusion events
-
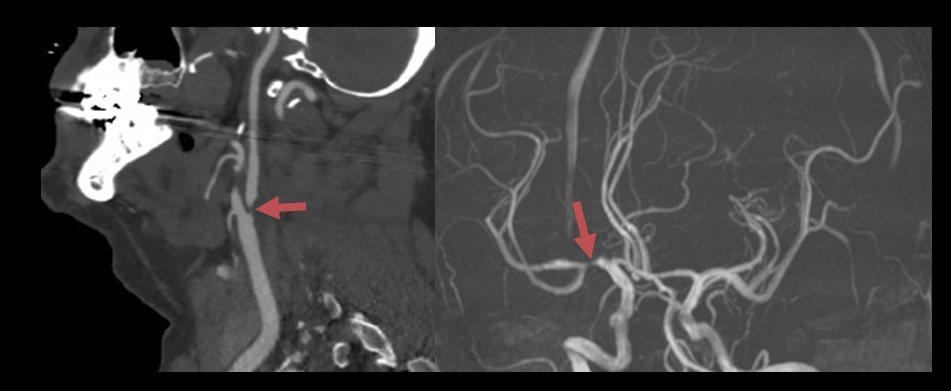
- parent artery plaque or thrombus leading to a stenosis or occlusion at the origin of the penetrating artery (branch artery disease)
- isolated acute infarct in the territory of a penetrating artery, evidence of plaque/any degree of stenosis at the junction of parent and penetrating arteries
-
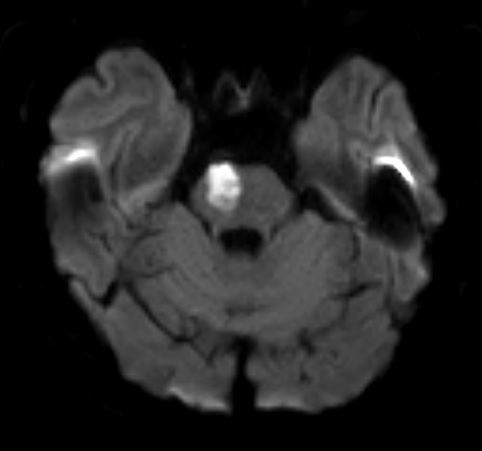
an isolated acute infarct in the basal ganglia, and no other acute infarct in the territory supplied by the ipsilateral MCA
-
an isolated acute infarct in the pons, and no other acute infarct in the territory supplied by the basilar artery
-
- isolated acute infarct in the territory of a penetrating artery, evidence of plaque/any degree of stenosis at the junction of parent and penetrating arteries
-
multiple mechanisms: ≥ 2 of the above underlying mechanisms are present
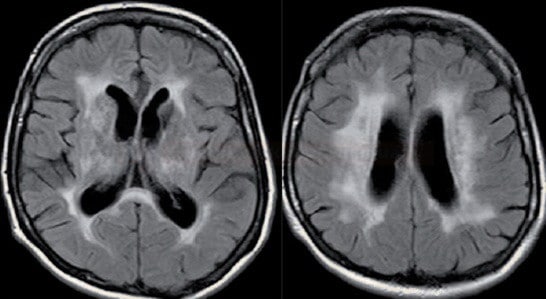
- severe stenosis leads to border zone infarction (BZI) due to hypoperfusion (hemodynamic effect) with/without impaired emboli clearance
- these two mechanisms are difficult to separate
- impaired emboli clearance is likely when TCD detects microembolizations (MES)
- however, the absence of MES does not exclude the presence of an impaired emboli clearance mechanism
Cardioembolic stroke
- multiple infarcts, especially those involving bilateral anterior and/or anterior and posterior circulation (including cortical infarcts), occurring in close temporal relation
- evidence of cardiac disease with embolic potential
- no evidence of atherosclerosis in relevant intracranial or extracranial large arteries (vulnerable plaques or stenosis ≥50% or occlusion)
- no evidence of other etiologies that can cause multifocal acute ischemic infarcts, such as vasculitides, hemostatic disorders, and tumor emboli
- if the possibility of aortic arch atherosclerosis has been excluded, CS is definite. Otherwise, the category should be possible CS
- any documented history of permanent or transient atrial fibrillation/flutter with or without spontaneous echo contrast or left atrial thrombus, sick sinus syndrome
- prosthetic heart valve
- myocardial infarction within the past 4 weeks
- left atrial/ventricular mural thrombus or left ventricular aneurysm
- dilated cardiomyopathy
- ejection fraction <35%
- endocarditis
- intracardiac mass
- PFO plus in situ thrombosis, PFO plus concomitant PE or DVT prior to stroke
Penetrating artery disease
- acute isolated infarct in the clinically relevant territory of one penetrating artery
- such an infarct may be caused by atherosclerosis at the junction of the parent (Branch Artery Disease classified as AA), atherosclerosis of the proximal segment of the penetrating artery, or lipohyalinotic degeneration of the arterioles (arteriolopathy)
- atherosclerotic lesions and fibrohyalinosis usually coexist – it is difficult or even impossible to distinguish between the two (both clinically and radiologically)
- high-resolution MRI (not used as a standard imaging technique) can detect atherosclerotic lesions in proximal segments of penetrating arteries ⇒ lacunar infarcts are not equivalent to intrinsic small vessel disease (fibrohyalinosis)
- atherosclerotic lesions and fibrohyalinosis usually coexist – it is difficult or even impossible to distinguish between the two (both clinically and radiologically)
- no evidence of atherosclerotic plaque (detected by HR-MRI) or stenosis in the parent artery
- with evidence of vulnerable plaques or stenosis ≥50% in the ipsilateral proximal intracranial or extracranial large arteries, the isolated penetrating infarct is classified as undetermined etiology – multiple etiology
- with evidence of cardiac disease with potential for embolization, the isolated penetrating infarct is classified as UE (multiple etiology)
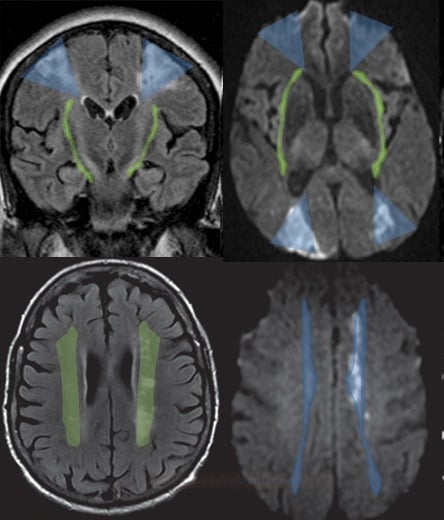
- chronic penetrating artery disease leads to leukoaraiosis (→ Binswanger´s disease)
- inherited cerebral microangiopathies (CADASIL, CARASIL, etc.) are classified as TOAST 4
Other etiology
- evidence of other specific diseases (e.g., vascular-related disease, infectious or inherited disease, hematologic disorder, vasculitis) that are relevant to the index stroke and that can be demonstrated by blood tests, cerebrospinal fluid (CSF) tests, and vascular imaging (see TOAST 4)
- the possibility of LAA or CS has been excluded
Undetermined etiology
- multiple: evidence of ≥ 1 potential cause; it is difficult to determine which was the relevant cause of the index stroke
- unknown: no evidence of any specific potential etiology that is clinically relevant to the index stroke
- inadequate evaluation: routine evaluation not completed, leaving etiology undetermined