ISCHEMIC STROKE / CLASSIFICATION AND ETIOPATHOGENESIS
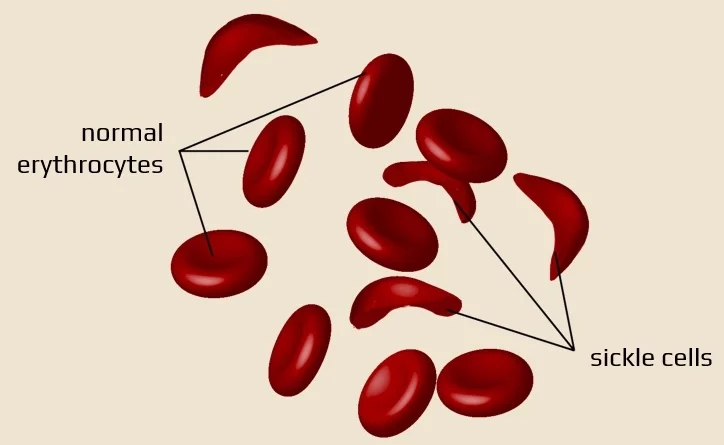
Sickle cell disease
Updated on 11/01/2024, published on 19/12/2021
- sickle cell disease (SCD) is caused by a genetic blood disorder that results in the production of abnormal hemoglobin molecules called hemoglobin S (HbS)
- the sickle-shaped red blood cells are more likely to clump together and block blood vessels
- one of the most serious complications of SCD is stroke (a major cause of death and disability in people with SCD, particularly children and young adults)
- stroke can be prevented with early detection and treatment
Pathophysiology
- sickle cell disease (SCD) is an autosomal recessive (AR) inherited disorder of the group of hemoglobinopathies, which is characterized by a change in the shape of erythrocytes into elongated sickles
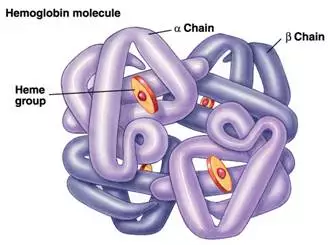
- HbS is caused by the substitution of glutamic acid for valine at the 6th amino acid of the β-globin chain (β6 Glu→Val), caused by a point mutation in the β-globin gene
- if a person carries one healthy gene and one HbS gene (heterozygote), they are carriers who usually have no health issues
- HbS makes up < 50% of the erythrocyte´s hemoglobin (most commonly 40%). The rest is normal hemoglobin (mainly HbA), which protects the individual against sickle cell disease
- a person with two HbS genes (HbSS), called a homozygote, cannot produce normal hemoglobin and develops clinical manifestations of sickle cell anemia
- SCD can also occur in people who have one sickle cell gene and one of the other hemoglobinopathies
- the homozygote´s hemoglobin has different properties ⇒ unoxygenated hemoglobin aggregates, which leads to erythrocytes deformation
- the disease manifestations usually start in childhood (from about one year of age), especially in people from tropical and subtropical areas where malaria is also common
blood stagnation ⇒ hypoxia
aggregation of blood cells in blood vessels ⇒ ischemia and infarcts
increased destruction of blood cells in the spleen ⇒ anemia
- human hemoglobin is a tetramer consisting of 2 pairs of polypeptide (globin) chains ⇒ 2 dimers
- the dimers are formed in definitive erythropoiesis by the combination of one α and one non-α chain (β, γ, or δ)
- each chain surrounds a heme, which is located in a heme pocket
- the heme is a protoporphyrin formed by four pyrrole nuclei (tetrapyrrole)
- in the center of the tetrapyrrole nucleus is a hexavalent and divalent iron ion, which can reversibly bind an oxygen molecule. This allows hemoglobin to perform its primary function – transfer of oxygen from lungs to tissues
- hemoglobinopathies are inherited diseases caused by a defect in the formation of one or more globin chains
- caused by mutations or deletions in the genes encoding the globin chains
- diseases with a defect in the structure of the globin chain
- sickle cell disease (SCD)
- methemoglobinemia
- diseases with defects in globin chain synthesis
- thalassemia
Pathogenesis of stroke in SCD
- large-artery vasculopathy affecting the intracranial segments of the internal carotid artery (ICA) and proximal segment of the middle cerebral artery (MCA) due to intimal hyperplasia caused by repeated traumatic injury, inflammation, and a hypercoagulable state
- progressive involvement of the arteries of the Circle of Willis leads to Moyamoya syndrome, which predisposes to both ischemic stroke and hemorrhage
- silent strokes typically occur in the territory of the penetrating arteries
Clinical presentation
- babies usually have no particular symptoms after birth
- the first symptoms rarely appear until around the first year of life, when hemoglobin S forms in their bodies
- early symptoms include pain and swelling in the arms and legs
- manifestations of sickle cell disease are variable
- ranging from mild discomfort to severe complications
- homozygotes tend to have worse symptoms, while heterozygotes are perfectly fine until their oxygen levels drop; this can be caused, for example, by dehydration, intense physical exertion, or staying at high altitudes
- symptoms (both acute and chronic) resulting from ischemia – sickle-shaped erythrocytes block the arterioles
- ischemic stroke (typically seen in children, with a radiologic appearance resembling moyamoya) with possible secondary hemorrhages
- pulmonary microinfarcts
- muscle pain
- bone necrosis
- papillary renal necrosis with hematuria, microalbuminuria, and proteinuria worsening with age and often leading to uremia
- skin ulceration, etc.
- hemolytic anemia with increased reticulocyte count
- vaso-occlusive sickle cell crises
- sudden attacks of severe, prolonged bone and muscle pain provoked by, e.g., exposure to high altitude, impaired lung function, increased metabolic activity, and dehydration
- individual crises usually resolve within a few days or even weeks, and their frequency varies from once a year to daily
- dysfunctional spleen (autosplenectomy) – consequence of infarcts and infections → more here
- acute worsening of anemia (pallor, fatigue, dizziness)
- infectious diseases (especially pneumonia, etc.)
- painful enlargement of the spleen
- liver enlargement and icterus
- gall bladder stones
- tibial ulcers
- retinopathy
- priapism
- development of bone deformities
- pulmonary hypertension
- heart failure
Diagnostic evaluation
| Content available only for logged-in subscribers (registration will be available soon) |
Management
Specific therapy
- the therapy aims to relieve the patient’s pain while at the same time minimizing the risk of organ damage
- if a circulatory event occurs, increased fluid intake + analgesics or opioids are recommended
- blood transfusion is indicated in cases of severe circulatory compromise (STOP and SIT trials)
- transfusion is recommended in ischemic stroke patients with a target HbS reduction of < 30% of total Hb; this results in a significant reduction in stroke recurrence (AHA/ASA 2021 1/B-R)
- transfusion also affects cholestasis, which can be severe
- hydroxyurea may be given to patients with a history of stroke who cannot receive transfusions (SWITCH trial) (AHA/ASA 2021 2a/B-R)
- increases gene expression of HbF (fetal hemoglobin – α2γ2), which does not contain defective β-subunits
- allogeneic hematopoietic stem cell transplantation (HSCT)
- may be considered for patients with severe SCD who are refractory to other treatments or who have organ damage due to the disease
- gene therapy (lentiviral vector)
- preventive measures
- patients should avoid infections and stay at high altitudes (erythrocytes can become sickle-shaped due to hypoxemia)
- administration of folic acid may be beneficial in preventing anemia
- patients should start treatment of any infection as soon as possible to prevent complications
Secondary stroke prevention
- no data from randomized trials are available on antithrombotic therapy in secondary prevention of stroke in patients with SCD
- caution is advised due to the increased risk of bleeding
- antithrombotic drugs are recommended in patients with SCD who have comorbidities, such as atherosclerosis or dissection