ISCHEMICKÉ CMP / STROKE MIMICS
Benign paroxysmal positional vertigo (BPPV)
Updated on 26/07/2024, published on 19/03/2024
Definition of vertigo and BPPV
- vertigo is defined as the sensation of spinning in a stationary environment
- this can happen due to inadequate signals from peripheral receptors or misinterpretation of these signals by the vestibular center, or a combination of both
- it is necessary to distinguish vertigo from frequent symptoms of nonvestibular origin (orthostatic hypotension, chronic imbalance due to neuropathy, lacunar state, weakness in hypoglycemia, migraine aura, imbalance due to alcohol or drug abuse, feelings of insecurity when wearing inappropriate glasses, etc.)
- vertigo, usually in combination with other symptoms, can be a sign of posterior circulation stroke; on the other hand, many vertiginous conditions (imbalance) have a nonvascular origin but cause difficulties in the acute phase as they resemble a stroke (stroke mimics)
- benign paroxysmal positional vertigo (BPPV) is a common cause of vertigo in adults and the elderly
- it is characterized by brief recurrent episodes of vertigo and is caused by displaced otoconia (calcium carbonate crystals) within the semicircular canals of the inner ear
- BPPV is triggered by specific changes in head position relative to gravity (when the affected semicircular canal is involved)
- most commonly occurs when getting up or lying down, rolling over in bed, tilting the head back, or bending over
- BPPV may develop after head trauma, viral labyrinthitis, or vascular lesions; no clear cause is identified in up to 50% of cases
- a careful history and clinical examination are important to differentiate positional from spontaneous vertigo
- distinguish persistent vertigo from recurrent attacks
- in elderly patients, it is important to identify concurrent vertiginous conditions (e.g. combination of BPPV and orthostatic dizziness or chronic imbalance due to neuropathy, etc.)
Pathophysiology
- BPPV most commonly occurs when otoconia (calcium carbonate crystals, also known as canaliths) become dislodged from the utricle of the inner ear
- the utricle is a small, fluid-filled structure within the vestibular system responsible for detecting linear acceleration and head position relative to gravity
- dislodged otoconia can migrate into the semicircular canals, particularly the posterior or lateral canals, where they can cause mechanical irritation of receptors with characteristic symptoms of BPPV
- the exact cause of BPPV is not fully understood – hormonal influence, calcium metabolism, or inner ear trauma are considered contributing factors
- there are several theories as to why otoconia become dislodged:
- due to age-related degeneration
- due to head injuries or trauma
- due to inner ear disorders, such as Meniere’s disease
- hormonal influences and calcium metabolism disorders are also discussed
- in most cases, however, the exact cause of otoconia displacement remains unknown, and BPPV may occur spontaneously without a clear precipitating factor
Vestibular apparatus
- the vestibular apparatus is a sensory organ that ensures the balance in space (in synergy with the visual and proprioceptive organs)
- it is located in the inner ear within the petrous temporal bone, which contains a bony labyrinth and a membranous labyrinth
- the bony labyrinth is filled with a fluid known as “perilymph”, which is comparable to cerebrospinal fluid and drains into the subarachnoid space
- suspended within the bony labyrinth is the membranous labyrinth that contains a fluid known as endolymph, unique in composition due to its high potassium ion concentration
- endolymph surrounds the sensory epithelium and interacts with hair cells
- the vestibular apparatus comprises:
- otolith organs utricle and saccule
- sensory neuroepithelium in the utricle and saccule is called the macula
- superior, posterior, and lateral semicircular ducts (canals)
- sensory neuroepithelium in the semicircular ducts is called crista ampullaris
- the semicircular ducts work in pairs to detect head movements (angular acceleration); a turn of the head excites the receptors in one ampulla and inhibits receptors in the ampulla on the other side
- otolith organs utricle and saccule
- macula and crista ampullaris contain specialized mechanoreceptors – hair cells
- neuroepithelium in the ducts respond to angular acceleration
- sensory cells of the macula are irritated by otoliths, providing perception of body position and gravity
- hair cells in the vestibular system are slightly different from those in the auditory system, in that vestibular hair cells have one tallest cilium, called the kinocilium. Bending the stereocilia toward the kinocilium depolarizes the cell and increases afferent activity. Bending the stereocilia away from the kinocilium hyperpolarizes the cell and results in a decrease in afferent activity.
- the vestibular (Scarpa) ganglion contains thousands of bipolar neurons that receive sensory input from hair cells within the macula and crista ampullaris
- axons from the vestibular ganglion join to become the vestibular nerve, which then joins the cochlear nerve to become cranial nerve VIII (vestibulocochlear nerve)
- signals carried by the vestibulocochlear nerve are then interpreted by the central vestibular system within the brainstem (Deiters’, Schwalbe’s, Bechterev’s, Roller’s nuclei)
- the central vestibular system unites the peripheral signals from both ascending pathways to elicit eye, head, and body motor responses for control of balance and orientation
Clinical Presentation
| Posterior semicircular canal |
- BPPV involving the posterior semicircular canal (PC-BPPV) is one of the most common variants of BPPV
- typically provoked by specific head movements, such as lying down, bending over, etc.
- vertigo occurs with a latency of several seconds, accompanied by rotatory nystagmus (fast component toward the undermost ear) with a vertical (upward) component
- unless the affected person changes position, the seizure subsides within tens of seconds
-
short-term dizziness may be present after turning to the unaffected side
- when the patient is examined in the upright position, the findings are completely normal, including vestibular function
- positional tests such as the Dix-Hallpike maneuver are used to diagnose this condition; the Epley or Semont maneuvers aim to move displaced otoconia out of the affected semicircular canal
- unsteadiness may temporarily persist even after the successful maneuver
| Horizontal (lateral) semicircular canal |
-
the lateral (horizontal) canal is less commonly affected (about 10% of BPPVs)
- LC-BPPV occurs when lying on the affected side or is provoked by turning the head sideways while lying on the back
-
turning the head from side to side (head is 30° inclined forward) provokes horizontal nystagmus, which has a geotropic or ageotropic direction, short latency (< 5 seconds), and a duration of 20-60 s (supine roll test)
- geotropic nystagmus – when the head is turned to either side while lying supine, the nystagmus beats towards the lower ear (ground)
- apogeotropic nystagmus beats away from the ground and is usually associated with cupulolithiasis
-
in contrast to posterior semicircular canal involvement, one-third of patients have caloric hyporeflexia on the affected side
Which is the bad ear?
- when LC-BPPV follows a treatment maneuver for PC-BPPV, the “bad” ear is considered to be the same one with the posterior canal BPPV
- in idiopathic cases with geotropic nystagmus, the “bad” ear is assigned to the side with the stronger nystagmus
- with apogeotropic nystagmus, the bad ear is assigned to the side with the weaker nystagmus (excitation is stronger than inhibition)
| Anterior (superior) semicircular canal |
- the prevalence of AC-BPPV is very low and uncertain (~ 3%)
- the anterior canal is the highest part of the ear, and it is not easy to get debris there (except during yoga or as a consequence of repositioning maneuvers in other canals)
- triggered by head movements, such as looking up or extending the neck
- AC-BPPV is diagnosed by positional down-beating nystagmus in the supine position (with torsional movement beating the downside) and up-beating nystagmus on sitting up (not always present)
- AC-BPPV is more complex than PC-BPPV and includes far more central nervous system conditions (i.e., brain tumors, stroke, Chiari Malformation) as alternative possibilities
| Central positional vertigo |
-
positional nystagmus without vertigo, often without latency, persisting for a long time
-
often purely vertical or beating to the ear above
-
rather mild intensity of vertigo
-
-
truncal ataxia with the inability to walk is common
-
positional nystagmus does not correspond to the plane of the stimulated semicircular canal
-
causes of central positional nystagmus include
-
MS
-
cerebellar and brainstem infarcts, hemorrhages, and tumors
-
Diagnostic evaluation
- the distinction between central and peripheral positional vertigo is essential
- diagnosis is mainly clinical, based on a thorough history and examination of positional tests
- the sensitivity of BPPV tests can be improved by having the patient wear Frenzel goggles
- a basic neurological examination is completely normal
- after performing the positional test, provide postural support until the patient is stable
| Peripheral | Central | |
| appearance | vertical- or horizontal-rotatory | purely vertical |
| latency | a few seconds | 0 |
| duration | resolves quickly (< 1min) | resolves slowly (>1 min) |
| intensity of vertigo | intensive | mild |
| mechanism | detritus in the semicircular canal | central disorder otolith-ocular pathway |
| localization | semicircular canal | brainstem, cerebellum |
| symptoms reoccur in the upright position | yes | no |
Posterior semicircular canal
- the patient is seated lengthwise on the examination table
- the clinician turns the patient’s head 45° toward the affected ear
- while maintaining the head position, guide the patient in a continuous motion from sitting to lying with the head hanging ~ 20 degrees off the table
- hold this position for 30-60 seconds or until nystagmus resolves
- return the patient back into a seated position and allow the patient to recover in the sitting position for 30 seconds
- then repeat the maneuver with the head turned to the opposite side (a 45-degree angle toward the unaffected side)
- guide the patient in one continuous motion from sitting to lying with the head hanging off the table at ~ 20 degrees
- hold this position for 30 to 60 seconds or until nystagmus resolves
- guide the patient back into the baseline sitting position
- do not perform cervical spine hyperextension in patients with cervical spondylosis!
- used as both a diagnostic and therapeutic maneuver
- begin with the patient sitting upright on the examination table, facing the examiner
- the patient’s head is quickly turned 45º to the unaffected side (the side without vertigo symptoms)
- the patient is then laid down quickly toward the affected side (the side causing vertigo symptoms), with the head remaining at a 45º angle (the patient’s nose should be pointing upward)
- this will induce dizziness and nystagmus; hold this position for about 3 minutes or until vertigo subsides
- next, the patient is quickly brought up to the opposite side (the unaffected side) while maintaining the same 45º head position (the patient’s nose should be pointing down toward the floor)
- hold this position for another 3 minutes (short-term dizziness and nystagmus may occur)
- finally, return the patient back to the initial upright sitting position
- after performing the maneuver, some instability may be felt (most often with a pullback); these symptoms resolve within 30 minutes
- it is recommended to sleep in a semi-seated position for 24 hours after the maneuver
- it is necessary to repeat the maneuver several times over the next few days if BPPV symptoms persist
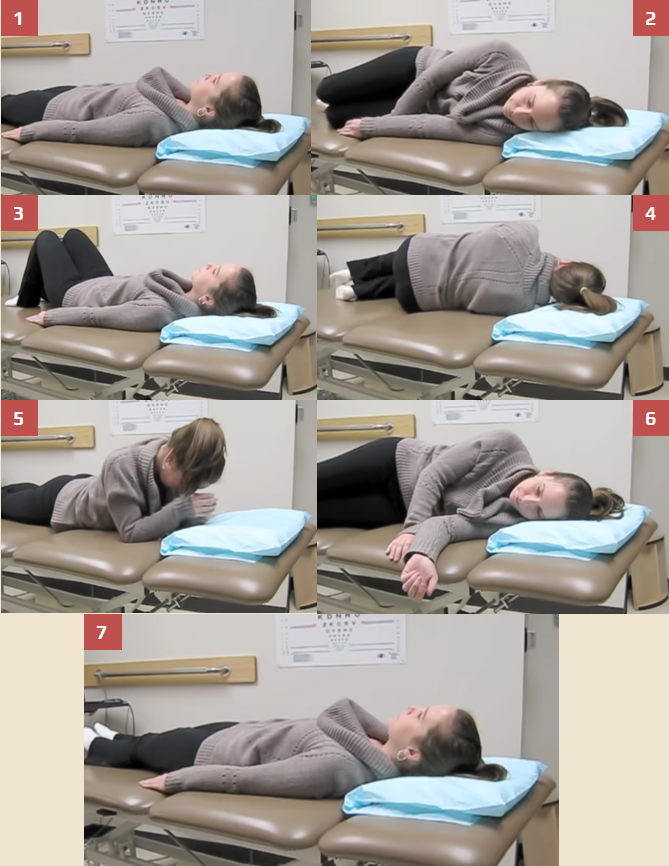
- the patient is sitting lengthwise on the examination table
- while sitting, turn the patient’s head 45º to the affected side
- while maintaining the 45º head position, guide the patient in a continuous motion from sitting to lying with the head hanging off the table at approximately 20º (provide cervical support during this procedure)
- hold this position for 30-60 seconds
- maintain the 20º head extension and rotate the patient’s head 90º toward the unaffected side so that the patient’s head is approximately 45º toward the unaffected side
- hold this position for 30-60 seconds
- while still maintaining the 45º head position, guide the patient into a side-lying position on the shoulder of the unaffected side (the patient’s nose points toward the floor)
- hold this position for 30-60 seconds.
- guide the patient back into a sitting position, making sure the patient’s head remains at the 45º angle
Lateral (horizontal) semicircular canal
- the individual is in the supine position with their cervical spine flexed to about 30 degrees with their head in a neutral, centered position (Hwu, 2022)
- then rotate the individual’s head 90 degrees toward the affected side and hold for 30 seconds after the nystagmus and vertigo symptoms have ceased (the affected ear is down)
- the head is then returned back to a neutral position (30s)
- then turn the head 90 degrees away from the affected side (30s) (affected ear is up)
- then rotate the whole body and end up lying on your stomach and then sit up
- if nystagmus and vertigo symptoms persist, multiple BBQ rolls may be required
Procedure for geotropic horizontal canal BPPV (the fast phase of the nystagmus beats towards the ground)
- before starting the procedure, ascertain whether the patient has any current or past neck or spine injuries!
- the patient is sitting on the edge of the examination table, facing the examiner
- with a rapid motion, guide the patient into a side-lying position toward the unaffected side; the head should remain in a neutral position initially
- while the patient is lying on his side, turn the patient’s head 45 degrees downward (nose down)
- hold this position for 2-3 minutes.
- finally, the patient is returned to the upright sitting position
Procedure for ageotropic horizontal canal BPPV ((the fast phase of the nystagmus beats upward)
- with a rapid motion, guide the patient into a side-lying position toward the affected side; the head should remain in a neutral position initially
- after the patient is in the side-lying position, the head is turned 45 degrees upward (nose up) for approximately 2-3 minutes
- finally, the patient is returned to the upright sitting position
- the patient is sitting length-wise on the examination table
- guide the patient into a supine position with their head elevated by 30 degrees
- turn the patient´s head 90 degrees to one side; if the patient does not have enough cervical flexibility to provide maximum otoconia displacement, have them roll onto their shoulder)
- observe whether nystagmus is present and make note of the severity and the direction
- guide the patient back into a neutral, supine position
- turn the patient’s head 90 degrees to the opposite side (or roll onto the shoulder)
- again observe for nystagmus and assess its severity and direction
- guide the patient back into the baseline supine position
- geotropic nystagmus ( beating towards the ground) is more common and typically responds well to repositioning maneuvers like the Gufoni or the Lempert (barbecue) maneuver
Anterior (superior) semicircular canal
- begin with the patient sitting on the examination table, facing the examiner, with the patient’s head turned at a 45º angle away from the affected side
- quickly guide the patient into a side-lying position toward the affected ear (patient’s nose should be pointing upward)
- hold this position for 2-3 minutes
- while maintaining the 45º head position, guide the patient in a continuous motion from side-lying on the affected side to side-lying on the unaffected side (the patient’s nose points toward the floor)
- hold this position for 3-5 minutes
- guide the patient back to the original sitting position, facing the examiner
- one begins with head up, then flips to upside down, comes back up into a push-up position with the head turned laterally (45 deg towards the bad ear), and then back to sitting upright
Differential diagnosis
Therapy
- repositioning maneuvers (as described above) can help reduce the duration of BPPV attacks and sometimes provide immediate relief
- maneuvers aim to relocate the displaced otoconia out of the semicircular canals back into the utricle, where they no longer cause symptoms
- positioning maneuvers should be repeated as long as the patient experiences symptoms
- after the maneuver, it is necessary to sleep with the head elevated(~ 20-30°)
- when maneuvers are repeated, their success rate is high
- pretreatment with intravenous antiemetics may be necessary in some cases
- BPPV typically does not respond to antivertiginous drugs
Prognosis
- ~ 10-20% of patients experience a worsening of symptoms within 1-2 weeks of treatment, ~ 50% of patients have a relapse
- patients should be educated and instructed on how to perform repositioning maneuvers themselves to treat future episodes
- in most cases, BPPV symptoms improve spontaneously within a few weeks
- for severe cases of BPPV that do not respond to repositioning maneuvers, surgery may be recommended