ISCHEMIC STROKE / CLASSIFICATION
SSS-TOAST CLASSIFICATION OF ISCHEMIC STROKE
Updated on 25/04/2024, published on 26/09/2022
- the SSS-TOAST classification is an evidence-based classification algorithm that reflects advances in stroke imaging and epidemiology [Ay, 2005]
- based on specific clinical and imaging criteria, each TOAST subtype is further categorized into one of three subcategories: “certain,” “probable,” or “possible.”
- this new algorithm refines the determination of the most likely etiology, particularly when multiple competing mechanisms are present
- an automated web-based version of the SSS-TOAST, known as the Causative Classification System (CCS), was developed to facilitate its use in multicenter settings (Ay, 2007)
- CCS enables fast analysis of patient data with excellent intra- and inter-examiner reliability
- particularly valuable in situations where precise classification is critical (such as in clinical trials)
- the text highlighted in purple was not included in the original SSS-TOAST publication in 2005
SSS-TOAST 1 – Large Artery Atherosclerosis (LAA) |
SSS-TOAST 3 – Small-artery occlusion |
SSS-TOAST 4 – Other causes |
SSS-TOAST 5 – Undetermined causes |
- cryptogenic embolism → ESUS criteria
- vascular imaging indicative of an embolic origin:
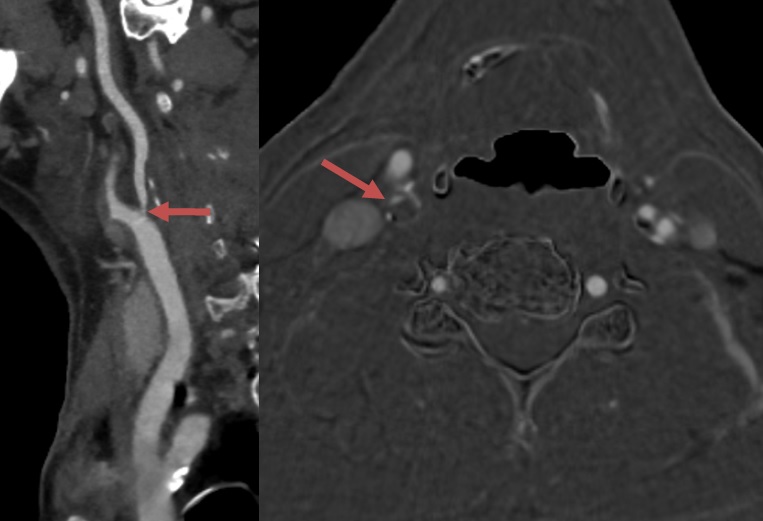
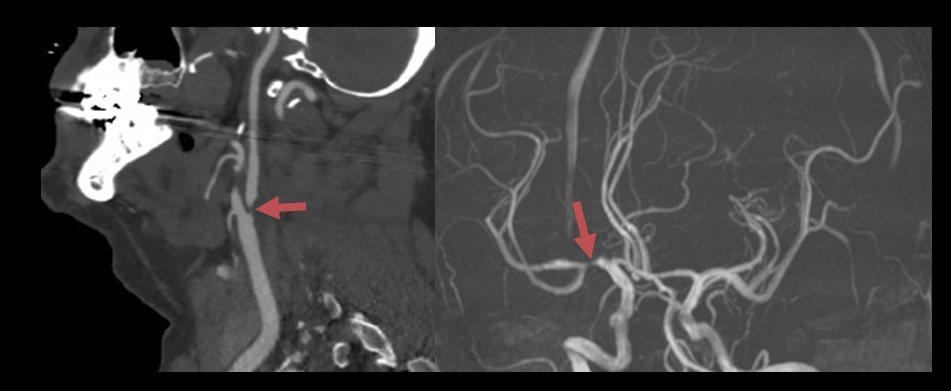
- abrupt absence of contrast, consistent with a blood clot, within otherwise angiographically normal-appearing intracranial arteries
- complete recanalization of the previously occluded artery
- multiple acute infarcts occurring in a close temporal relationship without apparent abnormalities in the relevant arteries
- vascular imaging indicative of an embolic origin:
- other cryptogenic strokes – those not meeting the criteria for cryptogenic embolism
- incomplete evaluation – the absence of essential diagnostic tests required to determine the underlying cause
- unclassified – the presence of >1 evident mechanism; either there is probable evidence for each, or no single cause can be reliably established