ISCHEMIC STROKE / ETIOLOGY
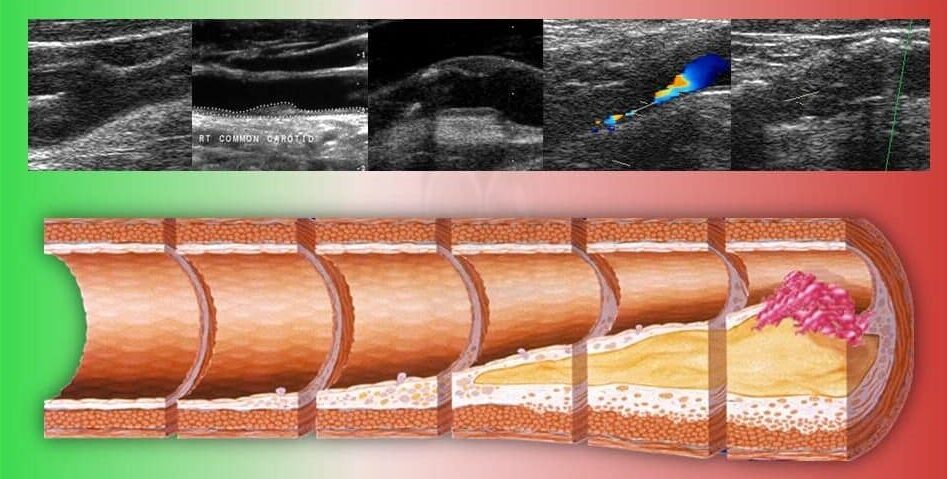
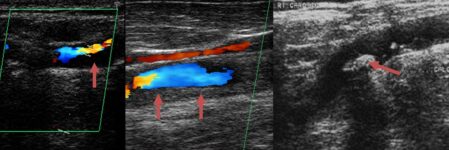
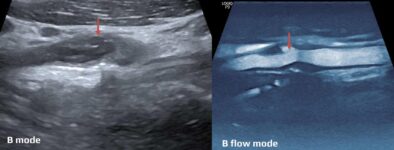
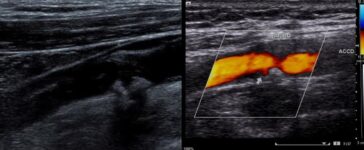
Assessment and classification of atherosclerotic plaques
Updated on 18/11/2023, published on 18/04/2023
Atherosclerosis
- atherosclerosis (AS) is a chronic, progressive systemic disease affecting the arterial wall that is a leading cause of death and disability in developed countries
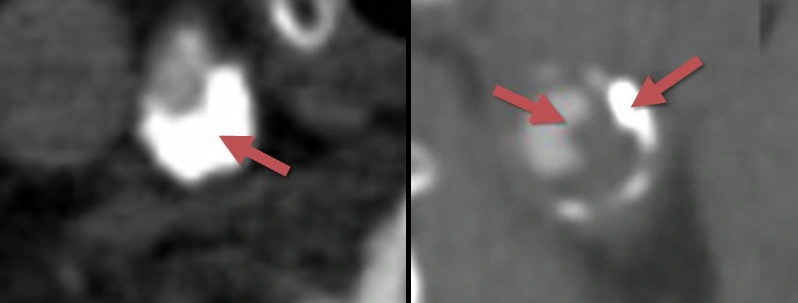
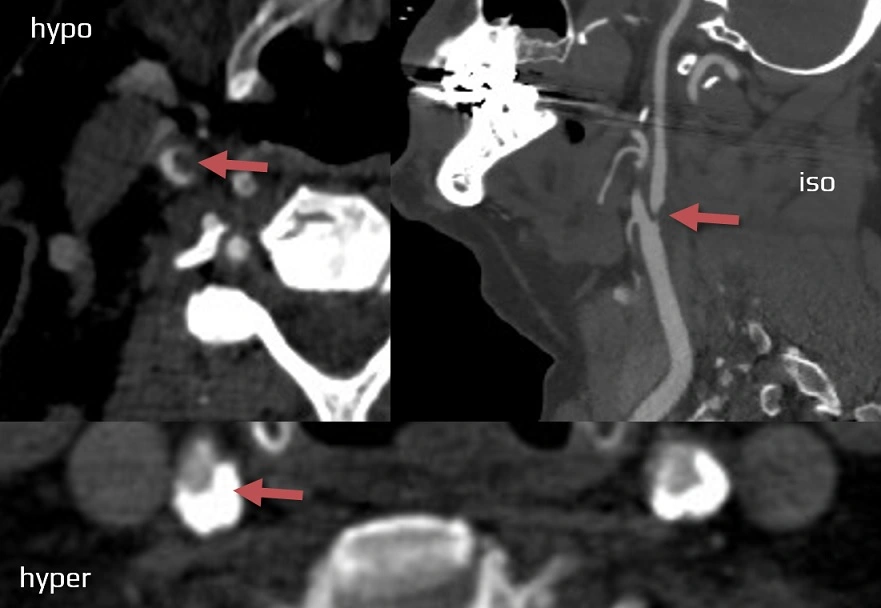
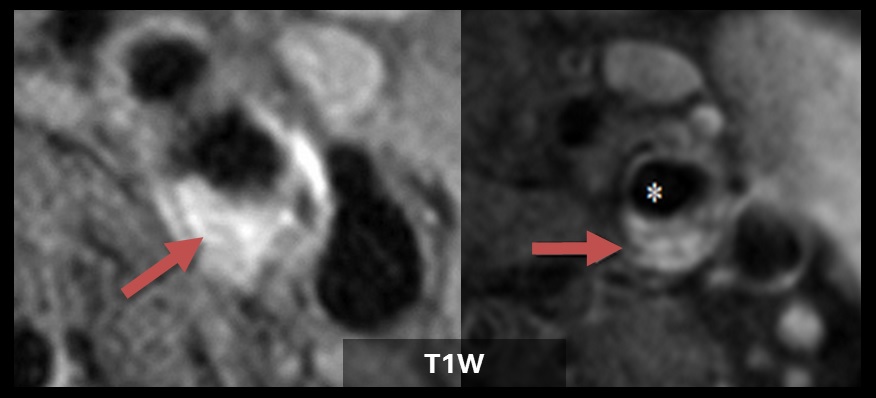
- the disease involves the accumulation of lipids, calcium, and other blood components within the arterial wall
- these lesions, called plaques, can result in arterial stenosis and may be complicated (thrombosis, rupture, etc.)
- plaques are predominantly found in specific segments of large and medium-sized arteries (carotid and coronary arteries, thoracic and abdominal aorta, arteries of the circle of Willis, etc.). Segments with arterial branches have the highest affinity for atherosclerotic changes
- while the exact cause is unknown, numerous vascular risk factors contribute to the disease
- the disease involves the accumulation of lipids, calcium, and other blood components within the arterial wall
- plaques may either be asymptomatic or may cause cardiovascular events (such as coronary artery disease, stroke, peripheral artery disease, etc.) due to:
- progressive narrowing to complete arterial occlusion (symptoms vary depending on the quality of the collateral circulation)
- artery to artery embolisms
- combination of both mechanisms (embolism occurring at the time of ICA occlusion)
- atherosclerosis generally begins in young adulthood and progresses with age; the rate of progression is individual, but nearly everyone is affected to some degree by the age of 65
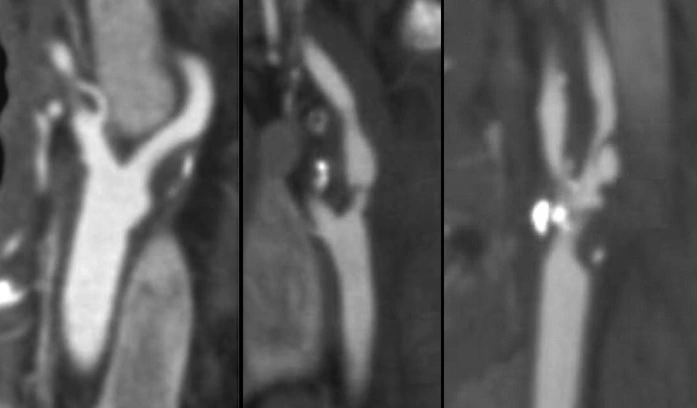
- modern imaging techniques allow a qualitative assessment of atherosclerotic plaque beyond mere measurement of the stenosis grade
- the first stage of atherosclerosis in the carotid arteries, detectable by sonography or MRI, is an increase in the intima-media thickness (IMT) (classified as a type 3 lesion according to AHA)