ADDONS / SCALES
NIH Stroke Scale (NIHSS)
Updated on 14/03/2024, published on 27/09/2022
- NIHSS is a standardized neurological scale developed to help physicians objectively quantify stroke severity
- scoring range: 0-42 (with higher scores indicating more severe stroke symptoms)
- scoring rules must be strictly followed to ensure reproducibility
- variants of the NIHSS have been introduced:
- modified NIHSS
- some items are easier to score; data indicate higher reproducibility compared to the original NIHSS
- however, it has not been widely adopted
- some items are easier to score; data indicate higher reproducibility compared to the original NIHSS
- NIHSS-8
- modified NIHSS
Different classifications and tresholds have been reported
- NIHSS < 8 (mild stroke)
- NIHSS 8-15 (moderate stroke)
- NIHSS ≥ 16 (severe stroke)
- NIHSS ≤ 4 (minor stroke)
- even patients with NIHSS 0 may have stroke and not TIA
- NIHSS 5-15 (moderate stroke)
- NIHSS 16-20 (moderate to severe stroke)
- NIHSS 21-42 (severe stroke)
- NIHSS ≤ 5 (minor)
- NIHSS 6–10 (mild)
- NIHSS 11–15 (moderate)
- NIHSS 16–20 (severe)
- NIHSS > 20 (very severe)
- administer the items in the order listed, and do not go back to change scores
- follow the instructions provided for each item
- score based on what the patient actually does, not on what the clinician believes they could or should do
- always assess the first response, not the best one (except for item 9 – Best Language)
- for example, if a patient initially gives an incorrect answer about their age and later corrects themself, the answer should be scored as incorrect
- this is crucial because otherwise, it is not possible to ensure reproducibility
- never assist or coach the patient during the examination (unless the instructions explicitly allow this)
- some items are scored only if present
- for example, ataxia is scored as absent in a plegic patient
- older deficits are also scored, except for sensory impairments
- NIHSS is NOT a guide to select tPA-suitable patients – tPA should be used regardless of severity → see IVT contraindication
- NIHSS indicates stroke severity and has been shown to correlate with infarct size and risk of hemorrhage
- NIHSS of >20 was associated with a 17% rate of intracranial hemorrhage when treated with tPA, compared to a 3% rate in patients with a score of <10 (The NINDS t-PA Stroke Study Group 1997).
- NIHSS may also predict large vessel occlusion (LVO)
- higher NIHSS indicates a higher probability of LVO; although a low NIHSS score does not necessarily exclude it
- some cut-off values for predicting LVO have been reported
- NIHSS scores ≥ 9 within 3 hours after symptom onset and NIHSS scores ≥ 7 within >3 to 6 hours (Heldner, 2013)
- higher NIHSS indicates a higher probability of LVO; although a low NIHSS score does not necessarily exclude it
- baseline NIHSS may predict clinical outcome
- a retrospective review of 1281 ischemic stroke patients found that each 1-point increase in NIHSS reduced the odds of an excellent outcome by 24% at 7 days and 17% at 3 months (Adams 1999).
- patients with moderate (6-13 points) or severe (>14 points) NIHSS scores were 3 times more likely to be placed in a nursing home after discharge and 8 times more likely to require rehabilitation therapy (Rundek 2000).
- patients with a score of ≤ 4 are highly likely to have favorable clinical outcome irrespective of treatment
|
National Institute of Health Stroke Scale (NIHSS)
|
||
|
1a. Level of Consciousness
|
0 – alert; keenly responsive
1 – not alert; arousable verbally or by minor stimulation to obey, answer, or respond 2 – not alert; requires repeated or strong/painful stimulation to make at least escape movements 3 – coma, reflex postures (reflex), totally unresponsive and areflexic |
|
|
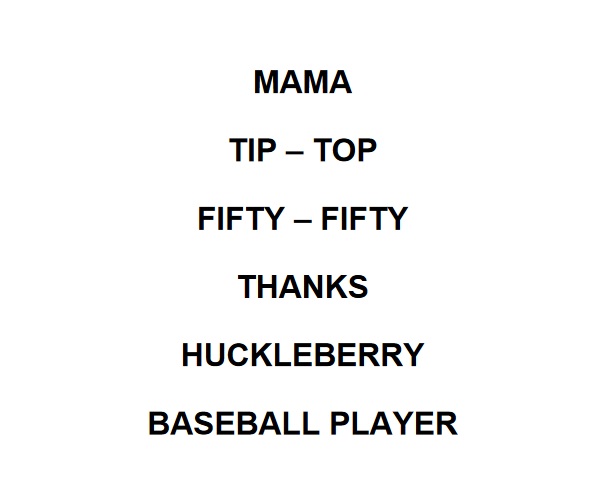
1b. LOC – Answers
|
0 – answers both questions correctly
1 – answers 1 question correctly or severe dysarthria/mechanical or language barrier 2 = answers neither question correctly, aphasia, coma |
|
|
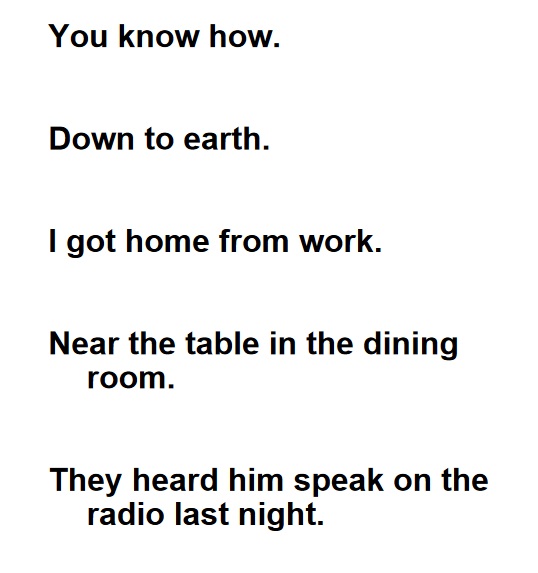
1c. LOC – Tasks
|
0 – performs both tasks correctly
1 – performs one task correctly 2 = performs neither task correctly, coma |
|
|
2. Best gaze
|
0 – normal
1 – isolated peripheral paresis or partial gaze palsy in one or both eyes; can be overcome by the oculocephalic maneuver, no forced deviation or total gaze paresis 2 – forced deviation or total gaze paresis, cannot be overcome by the oculocephalic maneuver |
|
|
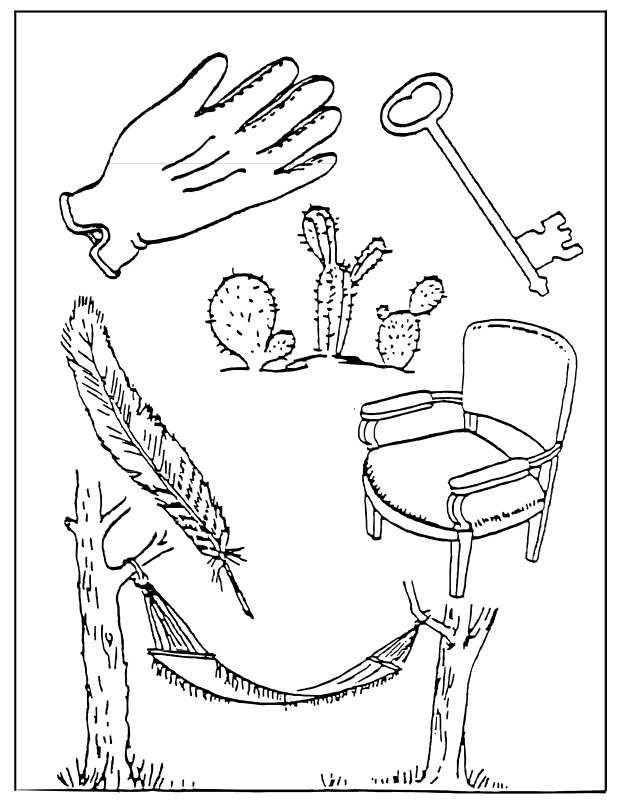
3. Visual fields
|
0 – normal
1 – partial hemianopia or extinction 2 – complete hemianopia 3 – bilateral hemianopia or blindness (including cortical blindness) |
|
|
4. Facial palsy
|
0 – normal
1 – minor paralysis (flattened nasolabial fold, asymmetry on smiling) 2 – partial paralysis (total or near-total paralysis of the lower face) 3 – complete uni- or bilateral paralysis (absence of facial movement in the upper and lower face), coma |
|
5. Motor arm
|
0 – no drift; limb holds 90 (or 45) degrees for 10 seconds
1 – limb drifts down before 10 seconds; does not hit the bed or other support 2 – some effort against gravity; limb fails to reach or maintain (if cued) 90 (or 45) degrees, drifts down to bed 3 – no effort against gravity; arm falls to the bed 4 – no movement UN = amputation or joint fusion, explain |
|
6. Motor leg
|
0 – no drift; leg holds 30-degree position for whole 5 seconds
1 – drift by the end of 5 seconds, but the leg does not hit the bed 2 – some effort against gravity; leg falls to bed by 5 seconds but has some effort against gravity 3 – no effort against gravity; the leg falls to bed immediately, with some movement on the bed 4 – no movement UN = amputation or joint fusion, explain |
|
|
7. Limb ataxia
|
0 – absent or paralyzed/does not understand/coma
1 – present in one limb 2 – present in two limbs UN = Amputation or joint fusion, explain |
|
|
8. Sensory
|
0 – normal
1 – mild-to-moderate sensory loss; pinprick is less sharp/duller, or there is a loss of superficial pain with a pinprick, but the patient is aware of being touched 2 – severe or total sensory loss; the patient is unaware of being touched; coma/unresponsive |
|
|
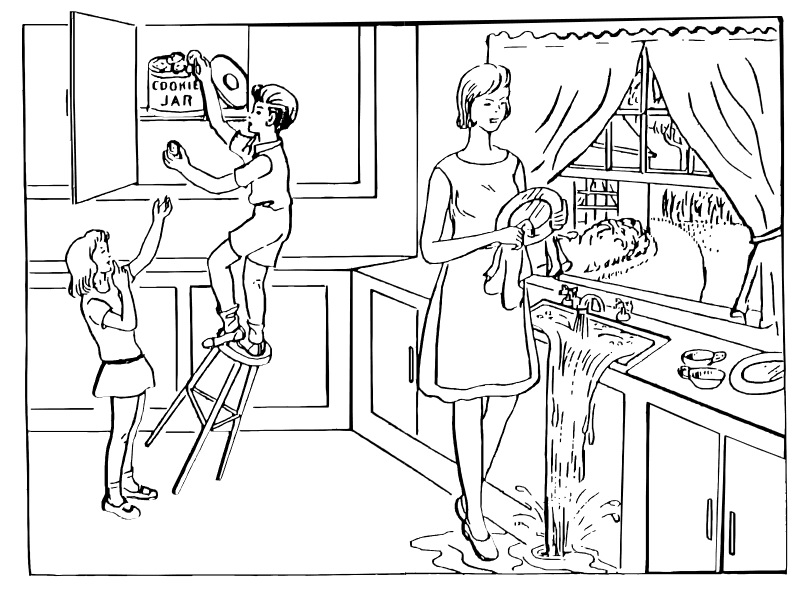
9. Best Langauge
|
0 – no aphasia
1 – mild-to-moderate aphasia; loss of fluency or ability to understand without significant limitation
2 – severe aphasia with fragmentary expression; the great need for inference, questioning, and guessing by the listener; the listener carries the burden of communication
3 – mute, global aphasia – no usable speech or auditory comprehension, coma/unresponsive
|
|
|
10. Dysarthria
|
0 – normal
1 – mild-to-moderate dysarthria; patient slurs at least some words, can be understood with some difficulty
2 – severe dysarthria (unintelligible slurring out of proportion to dysphasia), anarthria, mutism, coma
UN – intubated / other physical barriers – explain
|
|
|
11. Extinction and Inattention (formerly neglect)
|
0 – no abnormality
1 – neglects 1 modality – visual, tactile, auditory, spatial, or personal inattention or extinction to simultaneous bilateral stimulation in one of the sensory modalities 2 – neglects >1 modality, profound hemi-inattention or extinction (fails to recognize own hand or orients to only one side of space), coma |
|
|
Scoring patients in a coma (item 1a = 3)
|
|
|
1a Level of consciousness
1b LOQ questions (answers)
1c LOC questions (tasks)
2 Best gaze
3 Visual fields
4 Facial palsy
5-6 Arm and leg motor drift (left and right)
7 Limb Ataxia
8 Sensory
9 Best language (aphasia)
10 Dysarthria
11 Extinction and Inattention (neglect)
|
3 2 2 test oculocephalic maneuver test blink reflex 3 16 0 2 3 2 2 |