IMAGING METHODS
Overview of imaging modalities for an Acute Stroke
Updated on 06/11/2023, published on 14/09/2023
- historically, neuroimaging in patients with acute-onset neurological deficits has been used primarily to exclude hemorrhagic and nonvascular etiologies (e.g., neoplastic, infectious, etc.).
- over time, neuroimaging has become an essential part of acute stroke management and is used to:
- differentiate ischemic stroke from intracerebral hemorrhage and exclude other nonvascular causes (such as tumors, seizure, etc.)
- detect vascular lesions amenable to thrombolysis/embolectomy
- distinguish irreversible infarct from salvageable tissue (assess penumbra and core volumes)
- identify stroke etiology (with implications for stroke prevention)
- detect hemorrhagic stroke and rapidly identify vascular malformations and aneurysms
- non-contrast CT (NCCT) is usually the first-line imaging modality in most centers and is often combined with CTP and CTA
- brain MRI with DWI has the highest sensitivity and specificity and is the best option for diagnosing acute stroke
- superior to NCCT for the early detection of acute ischemic changes (DWI)
- may not be available in all centers and is time-consuming
- valuable in the subacute phase
- digital subtraction angiography (DSA) remains the gold standard for the evaluation of carotid and vertebral arteries, but with the advancement of noninvasive imaging techniques, its main role is in the interventional treatment rather than sole diagnosis
- neurosonology (Doppler ultrasound)
- used mainly in the subacute phase (to assess stenoses, detect reight-left shunts, monitor vasospasms in SAH patients, etc.)
- ultrasound can also be useful in the acute phase for:
- monitoring the occluded vessel during thrombolysis
- detection of occlusion and assessment of intracranial flow (incl. collaterals)
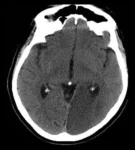
NCCT
- early signs of ischemia (ASPECTS)
- hyperdense sign
- hemorrhagic transformation
- other abnormalities
CT angiography (CTA)
- occlusion of the extra- or intracranial artery?
- thrombus location and extent → Clot Burden Score
- status of collateral circulation
- signs of vasculitis or any specific vasculopathy?
CT perfusion (CTP)
- evaluation of penumbra and core (perfusion mismatch)
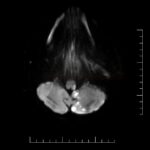
MRI
- ischemia?
- hemorrhagic component or microbleeds?
- edema?
- other pathology? (with negative DWI, consider seizure or neuroinfection)
- if dissection is suspected, add neck MRI (T1, T2 FES sequences)
DWI/ADC
- signs of acute ischemia?
- correlation between DWI and ADC map?
- DWI/FLAIR mismatch?
PWI
- perfusion deficit?
- PWI/DWI mismatch?
MR angiography (MRA)
- occlusion of extra or intracranial artery?
- thrombus location and extent?
- quality of collateral circulation?
- probable etiology?
GRE/SWI
- signs of recent bleeding?
- microbleeds?
- superficial siderosis?
- blooming effect?
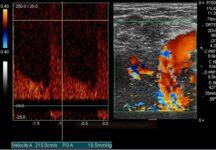
Neurosonology
- detection of extra- and intracranial stenosis/occlusion (acute x chronic)
- assessment of collateral circulation
- monitoring of thrombolysis
- detection of spontaneous embolizations
- right-left shunt (RLS) detection (bubble test)
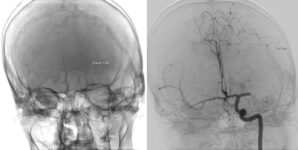
DSA
- detection of stenoses and occlusions + collateral circulation
- endovascular intervention
- diagnosis of vasculitis
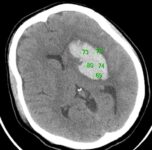
NCCT
- hematoma location and volume (ICH score)
- bleeding in typical x atypical location?
- atypical appearance? (suspicion of secondary bleeding, e.g., into ischemia, tumor, etc.)
- predictors of hematoma expansion? (Island sign, Blend sign, Black hole sign)
- signs of trauma?
- expansive behavior with brainstem compression?
- indication for acute evacuation?
- intraventricular component?
- complications? (hydrocephalus, midline shift, etc.)
CT angiography (CTA)
- source of bleeding?
- markers of ongoing bleeding? (Spot sign, Leakage sign)
MRI
- signal characteristics vary based on the age of the hematoma and the stage of hemoglobin breakdown
- oxyhemoglobin
- deoxyhemoglobin
- Intracellular methemoglobin
- extracellular methemoglobin
DWI/ADC
- hyperintense in the superacute hematoma
- it is difficult to reliably distinguish the hemorrhagic infarction from primary intracerebral hemorrhage
- additional DWI lesion(s) may indicate ischemia with secondary hemorrhage
MR angiography (MRA)
- source of bleeding?
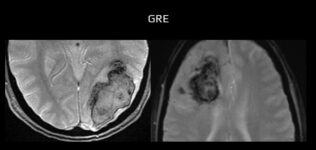
GRE/SWI
- sensitive to acute and chronic bleeding
- microbleeds?
- older lobar hematomas? (amyloid angiopathy)
- superficial siderosis?
- in the hyperacute phase, there may only be a dark rim if not enough deoxyhemoglobin is present
DSA
- detection of the source of bleeding (replaced by CTA during the initial examination)
- indications:
- age < 50 years in any location of ICH
- atypical location or appearance of the hematoma
- typical location without a history of hypertension
- isolated intraventricular hemorrhage
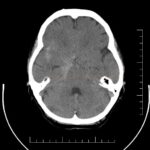
NCCT
- assess Fisher scale
- signs of trauma?
- evolving hydrocephalus?
- associated ICH or IVH?
- non-traumatic cortical SAH?
- secondary ischemia (DID)?
- benign perimesencephalic SAH?
CT angiography (CTA)
- source of bleeding?
- vasospasms?
CT perfusion (CTP)
- severe hypoperfusion due to vasospasms (with ↑risk of DID)?
MRI
- non-traumatic superficial cortical SAH?
- thrombosed aneurysm?
MR angiography
- source of bleeding (aneurysm, malformation?)
GRE/SWI
- older bleedings in different locations?
- superficial siderosis?
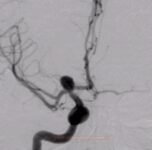
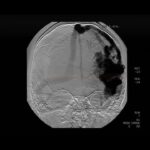
DSA
- source of the bleeding?
- vasospasms?
- lesion treatable with an endovascular procedure?
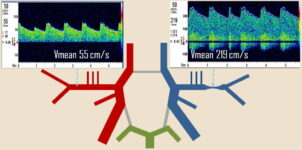
TCD/TCCD
- detection and monitoring of vasospasms
- collateral circulation
- vasomotor reactivity
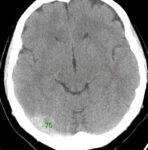
NCCT
- atypical location and shape of ischemia, with possible hemorrhagic component
- significant edema on baseline imaging
- presence of dense sign (> 70 HU) or cord sign in venous sinuses
CT venography (CTV)
- detect sinus thrombosis and its extent
- note collateral circulation with congestion of cortical veins (dilatation, tortuous passage
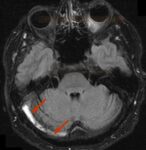
MRI
- ischemia in atypical localization, often with hemorrhagic infarction (FLAIR)
- absence of flow void (normally the sinus is hypointense) < 24h or > 3 days
- thrombus in the acute stage can be mistaken for normal flow void (T1 and T2 hypointense within first 3 days)
- from day 4, the thrombus should be already hyperintense in T1 and T2 images
MR venography (MRV)
- extent of the thrombosis; beware of confusion with hypoplasia (hypoplasia or congenital vascular anomalies can mimic thrombotic events)
- collateral circulation with cortical vein congestion (dilatation, tortuous course)
GRE/SWI
- hypointense thrombus in the lumen of the sinus
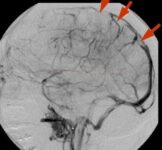
DSA
- reserved for interventional procedures
- , specific finding is the “stop sign” (sudden termination of a sinus or vein) + collateral circulation with cortical veins congestion (dilatation, tortuous course)


