NEUROIMAGING / NEUROSONOLOGY
Neurosonology and the brain death diagnosis
Updated on 02/02/2024, published on 29/11/2021
Introduction
- brain death and cerebral circulatory arrest (CCA) are not identical conditions
- brain death is a clinical diagnosis characterized by the irreversible loss of all brain functions, including those of the brainstem
- several mechanisms lead to brain death: increase in intracranial pressure (ICP), subsequent loss of cerebral autoregulation, ↓ cerebral blood flow, and ultimately, cerebral circulatory arrest
- there may be a delay of several hours between the onset of circulatory arrest and clinically detectable loss of brain function
- brain death is a clinical diagnosis characterized by the irreversible loss of all brain functions, including those of the brainstem
- TCD/TCCD is a non-invasive bedside technique that allows for monitoring or frequent checks in neurocritically ill patients
- a decrease in intracerebral flow can be detected, progressing to cerebral circulatory arrest
Intracranial flow patterns
- the increase of intracranial pressure (ICP) and subsequent decrease of cerebral perfusion pressure (CPP) result in progressive changes in the waveform of the Doppler spectra → Hemodynamics notes
decrease of flow velocities
↓
increase of pulsatile and resistance indexes (resistant flow)
PI and RI rise since ICP > 15 mm Hg
rough ICP formula = (10.927* PI) -1.284 [Brandi, 2010]
PI >3 = CBF < 20% of normal values
↓
a gradual decrease of end-diastolic velocity (EDV) down to 0 cm/s (ICP = diastolic blood pressure)
there is no circulatory arrest at this stage as the brain is still perfused during systole
biphasic, reverberating flow
net flow = anterograde-retrograde component of Vmean is < 4 cm/s (some report < 10 cm/s), the cerebral perfusion has ceased
↓
systolic spikes
flow with very short duration during systole, PSV < 50 cm/s, duration < 200 msec, no hemodynamic significance
↓
absent flow
may serve as a sign of brain circulatory arrest if the examiner has previously documented intracranial flow, thus ruling out a poor insonation window
Examination procedure
- the examination should be performed by a trained physician experienced in ultrasound technique and familiar with the pathophysiology of brain death
- a 2MHz diagnostic probe is used
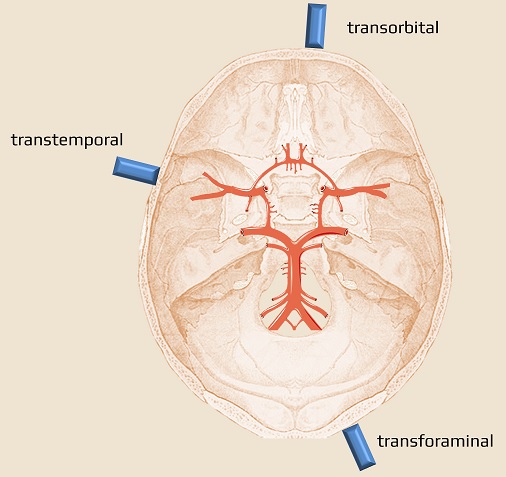
- basic approaches include:
- transtemporal window
- transforaminal window (via the foramen magnum)
- transorbital window
- proof of cerebral circulation arrest – requires registration of typical flow patterns (either oscillations or systolic spikes) in multiple intracranial arteries (MCA, ACA, PCA, terminal ICA, VA, and BA) is required – at least in the MCA bilaterally and in the basilar artery
- evaluation of the ICA alone is not appropriate (possible shunt to ECA without brain perfusion may occur) (Freitas, 2003)
- assessment of the BA is essential to avoid false-positive results
- a pathological flow pattern can also be detected in the extracranial arteries (CCA, ICA, VA) or the ophthalmic artery (Blanco, 2020)
- proof of the irreversibility of cerebral circulatory arrest:
- an examination showing the aforementioned flow pattern ≥ 30 minutes OR
- repeated examinations separated by intervals of ≥ 30 minutes
- transitory patterns compatible with cerebral circulatory arrest have been described in patients with SAH rebleeding and after cardiac arrest; a 30-minute interval is sufficient to confirm the irreversibility of the pattern
- transitory patterns compatible with cerebral circulatory arrest have been described in patients with SAH rebleeding and after cardiac arrest; a 30-minute interval is sufficient to confirm the irreversibility of the pattern
- an examination showing the aforementioned flow pattern ≥ 30 minutes OR
MAP (Mean Arterial Pressure) should be > 60 mmHg and systolic BP > 90 mmHg during the whole ultrasound examination
Poor acoustic window
- use ultrasound contrast agents (up to 98% of patients can be examined this way)
- use a different approach (incomplete examination should not be used as a confirmatory test of circulatory arrest)
- transorbital (detect flow in the carotid siphon)
- extracranial examination (indirect proof of circulatory arrest)
Skull defects
- patients with clinical brain death who have undergone large craniectomy or have skull fractures, persistent diastolic flow may be observed (similar to what occurs in children less than 1 year of age in whom the fontanelles are still open)
- in such cases, other diagnostic modalities like cerebral angiography or radionuclide imaging may be necessary to confirm the diagnosis of brain death