NEUROIMAGING / NEUROSONOLOGY
Transcranial Doppler ultrasound
Updated on 11/11/2023, published on 24/10/2023
Trancranial Doppler ultrasound (TCD/TCCD) is a non-invasive imaging technique helpful in evaluating flow in intracranial vessels → general indications for the examination
Transcranial examination procedure
Methods
- the probe utilizes ultrasound with a frequency of 2-2.5 MHz
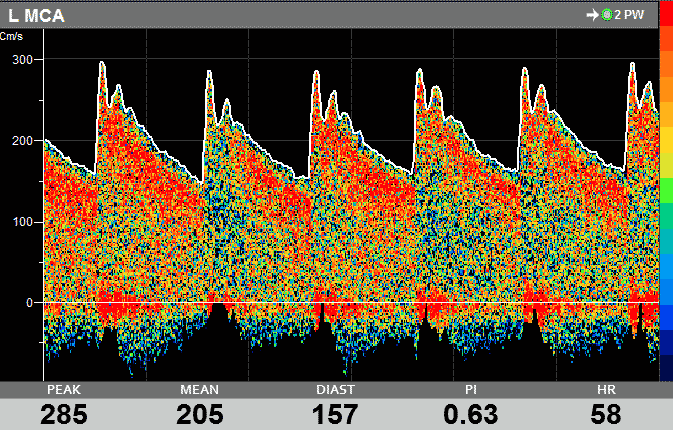
- in pulse-wave (PW) mode, the device registers the frequency shift (∆f) created by the reflection of ultrasound from moving blood particles and converts it into a graphic record and audible sound using FFT transformation
- transcranial Doppler sonography (TCD) allows measurement of flow (by obtaining the Doppler waveform) in intracranial arteries
- velocities are calculated from the frequency shift of the reflected ultrasound beam,
- TCD displays no anatomical structures; the examined vessel is determined by the insonation depth and probe position
- correction of the insonation angle is not possible (insonation angle is considered to be 0 grade)
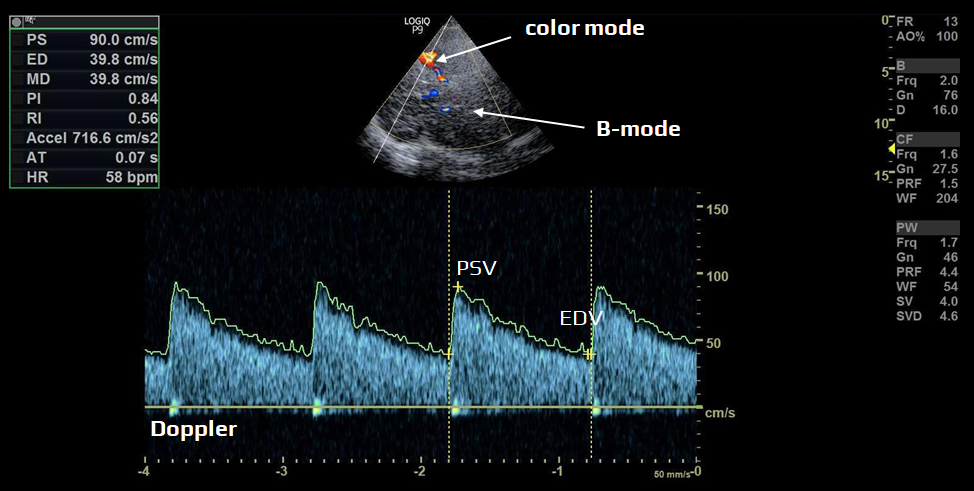
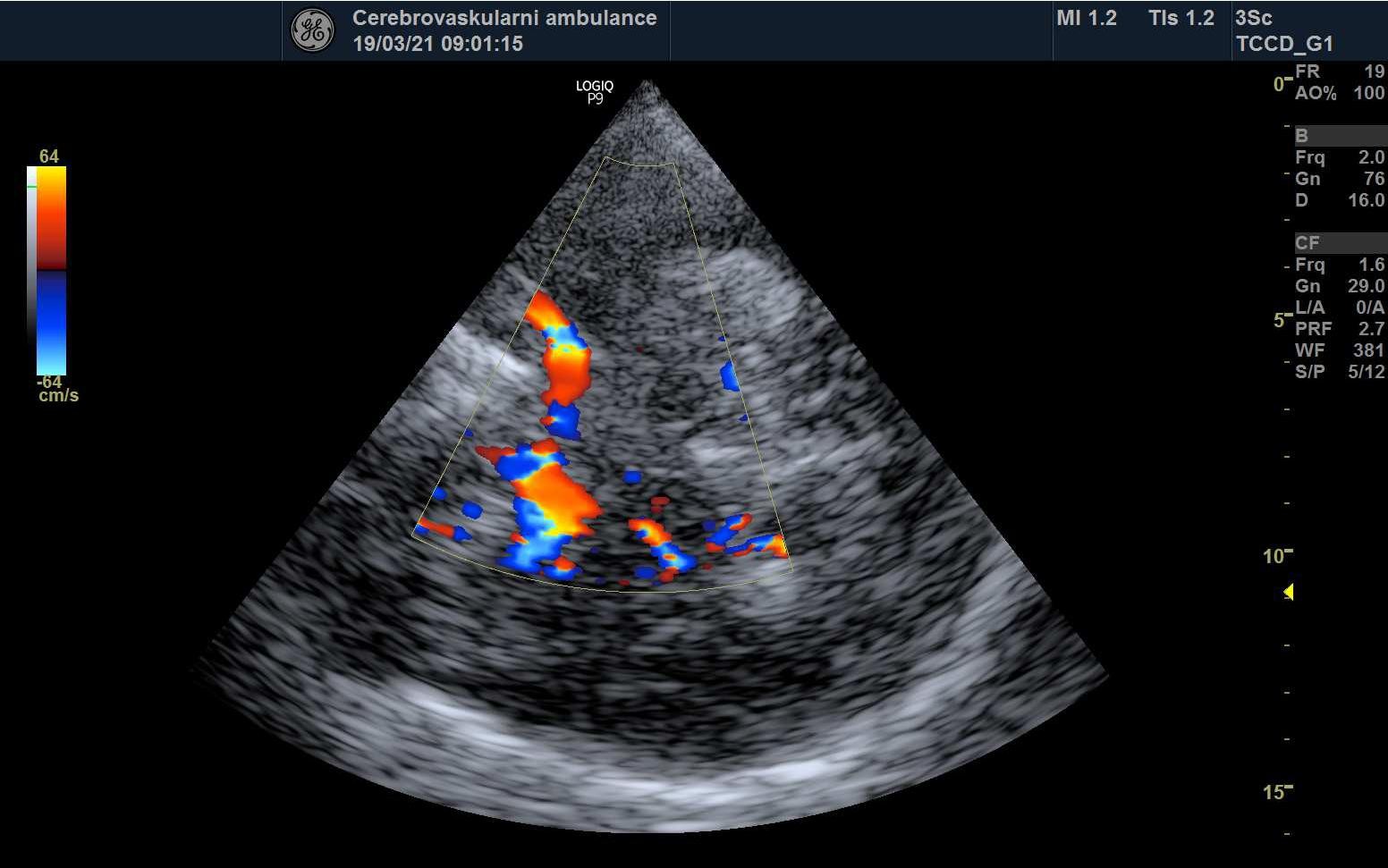
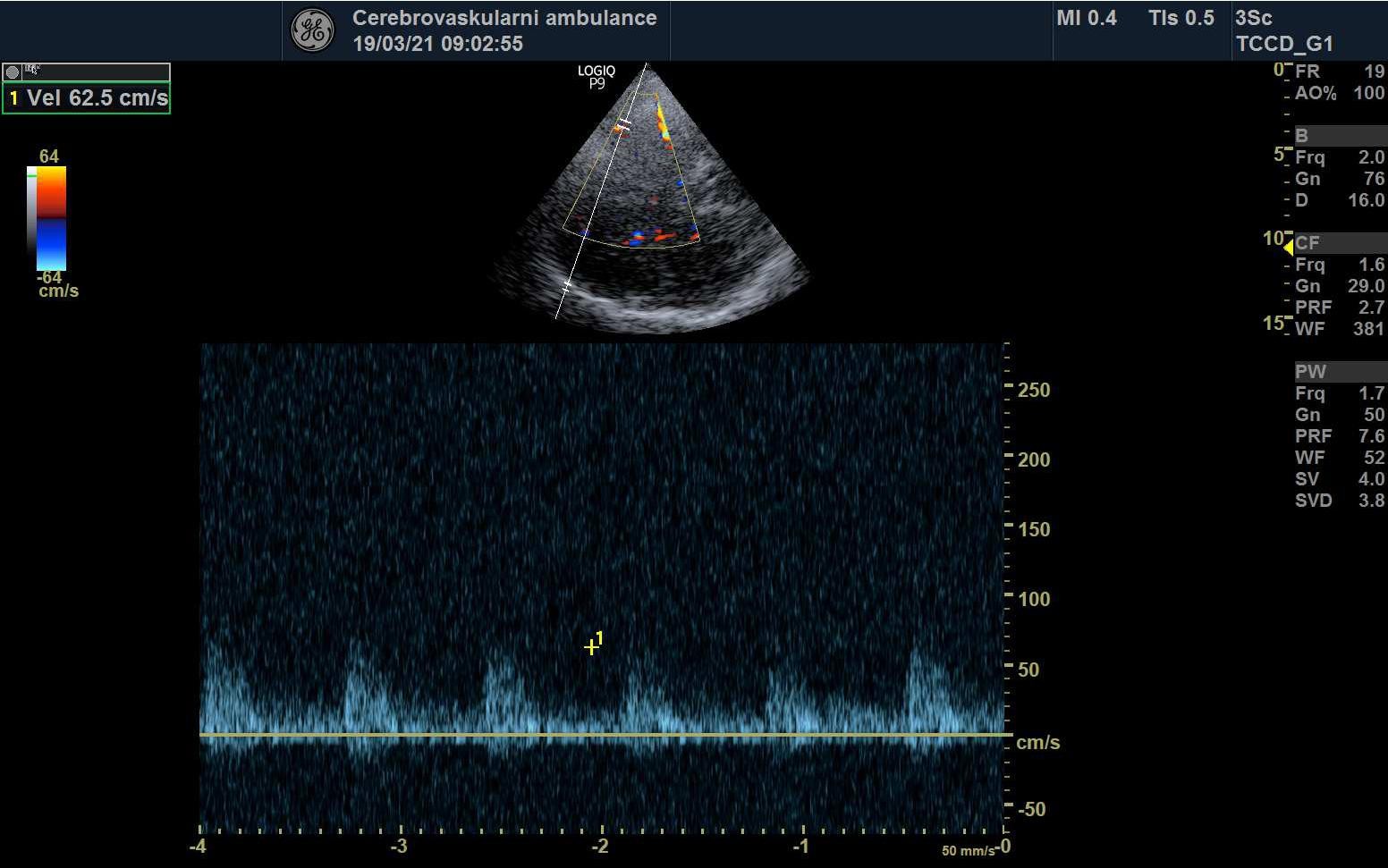
- transcranial color-coded Doppler (TCCD)
- TCCD provides enhanced diagnostic capabilities compared to standard TCD
- in addition to Doppler waveform, TCCD integrates B-mode imaging to visualize anatomical structures, as well as color, energy, or B-flow modes for vessel identification
- sample volume can be thus reliably positioned within the desired arterial segment
- angle-corrected flow velocities can be obtained
- these velocities are up to 30% higher than uncorrected velocities obtained on TCD
- limitation: an impenetrable temporal bone window (affecting ~ 5-20% of patients)
- a large proportion of these patients can be investigated using contrast agents (ECHOVIST, SONOVUE)
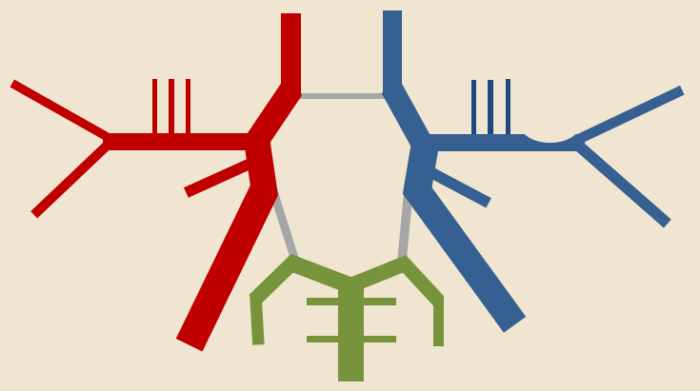
Transcranial windows
TCD/TCCD is typically examined using a high-frequency transducer placed over specific cranial windows (regions where ultrasound imaging can be performed with minimal interference from bone):
- in 5–20% of cases, cranial hyperostosis is the cause of poor insonation window, particularly in the temporal region
- the quality of the bone window is crucial for the sensitivity and specificity of transcranial sonography
| The quality of the temporal bone window can be assessed in five degrees: | |
| absent |
|
| very bad |
|
| bad |
|
| average |
|
| perfect |
|
Examination
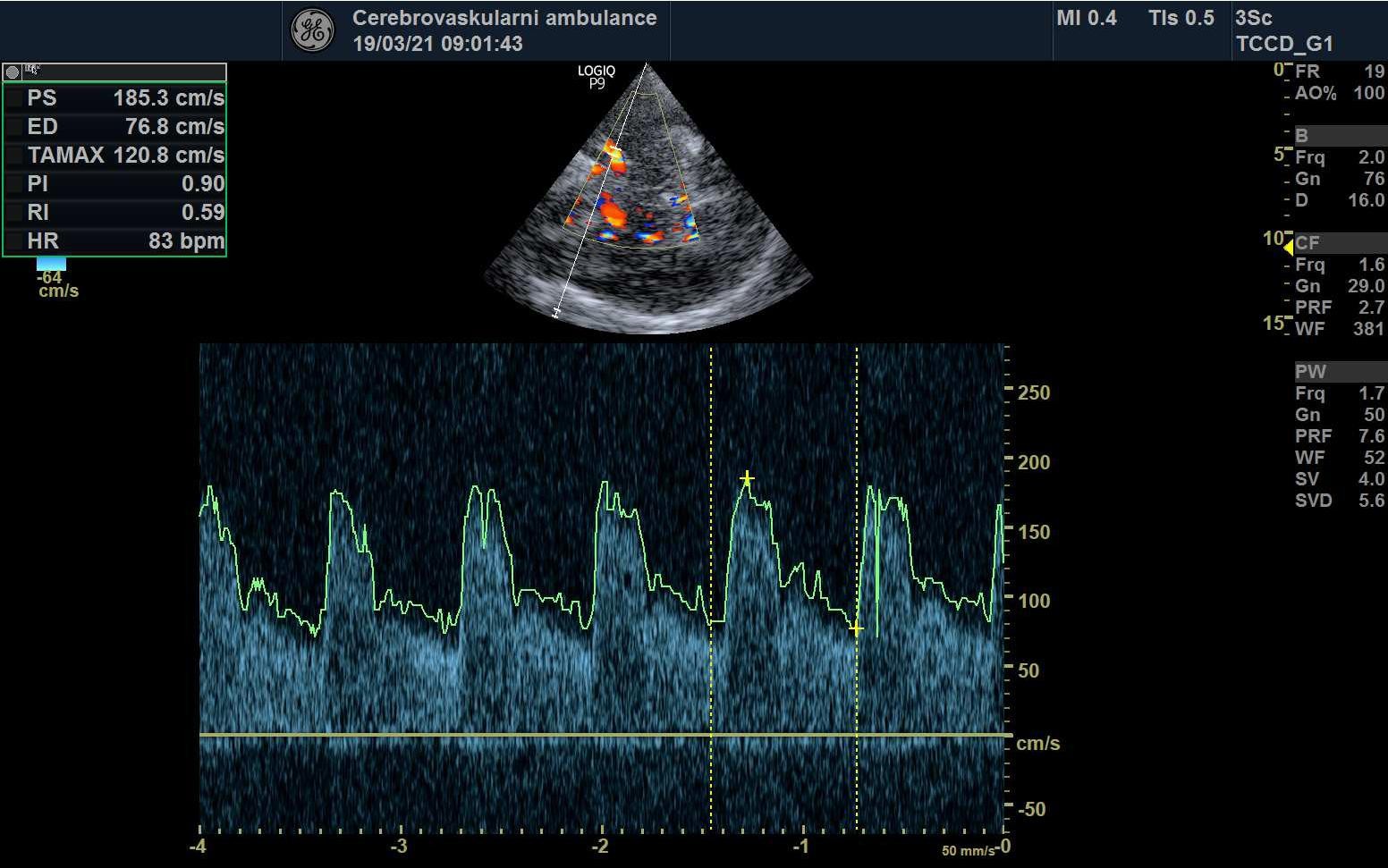
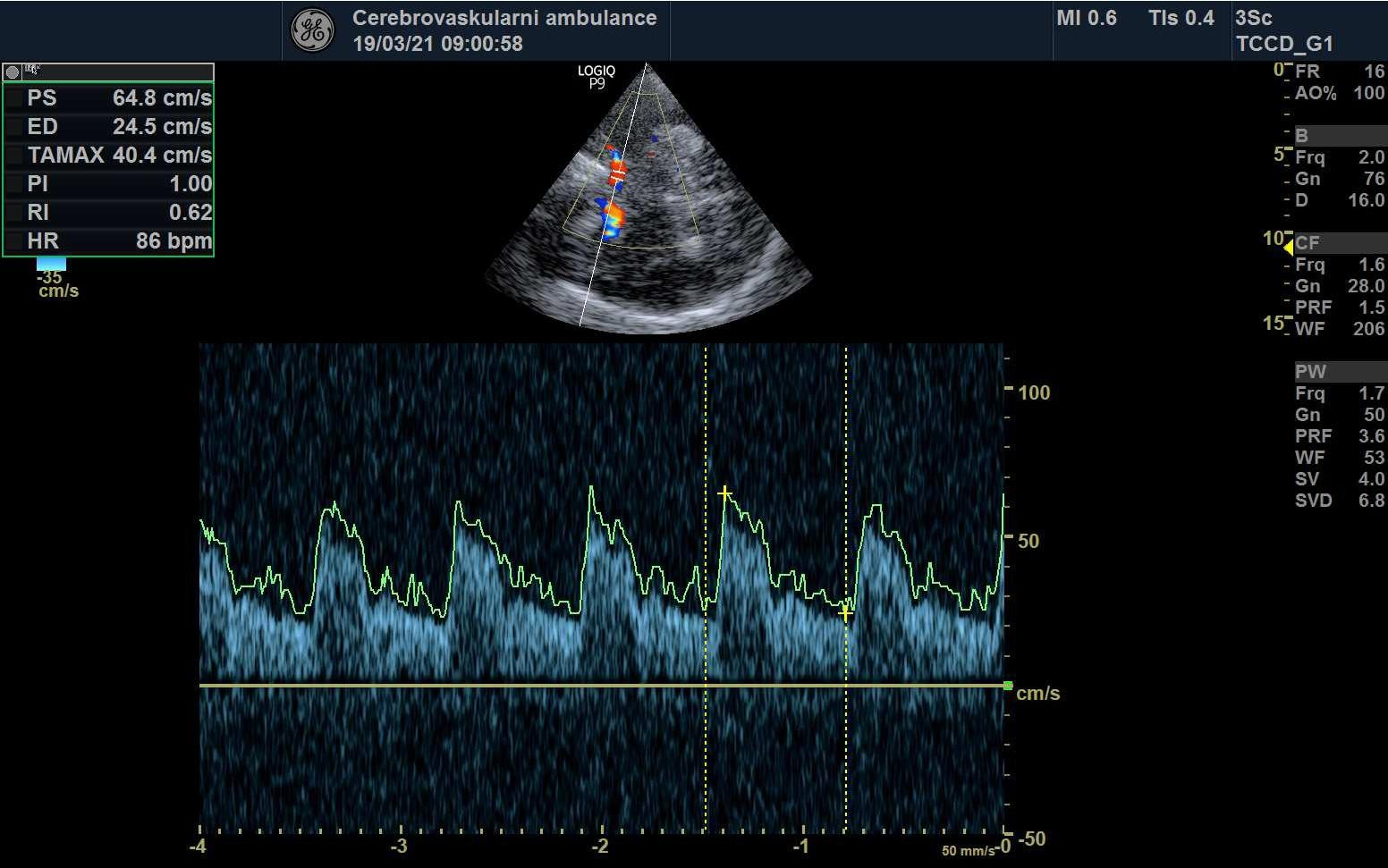
Correct evaluation of the Doppler waveform in the examined arteries is crucial; it is essential to take into account the findings in the extracranial arteries and to consider additional factors (hypotension, significant changes in pCO2, arrhythmias, marked anemia, valvular defects, etc.)
- assess the flow pattern (laminar x turbulent)
- evaluate Peak Systolic Velocity (PSV), End Diastolic Velocity (EDV), Resistance Index (RI), and Pulsatility Index (PI), as well as systolic acceleration (acceleration time)
- compare flow on both sides (unless there is pathology there, too) and between individual arteries
- normal findings
- interhemispheric difference < 20-30%
- PSV: MCA > ACA, ACM > PCA, BA > VA
- cut-offs for normal PSV and EDV (see in the table)
- RI < 0.8 and PI < 1.0
- identify possible steal syndrome
- search for embolic signals (HITS)
- spontaneous
- provoked as part of a bubble test
- asssess cerebral vasomotor reactivity (CVR) in selected cases
- note other waveform alterations
Normal finding
- continuous, laminar flow, no aliasing
- normal systolic acceleration (AT)
- normal PSV/EDV and resistance indices (see table below)
- PSV/EDV ± < 2SD
- PI/RI ± < 1SD
- no HITS, no turbulence or low-frequency murmurs
- normal CVR
- no arrhythmias
| Average velocities in cm/s (with angle correction) +- 1 standard deviation (SD) | ||||
| Artery |
flow velocity and resistance index
|
age | ||
| 20 – 40 years |
40 – 60 years | > 60 years | ||
| MCA |
PSV (cm/s)
|
91 -126 | 84 – 120 | 78 – 109 |
| EDV (cm/s) | 37 – 70 | 35 – 61 | 28 – 48 | |
| RI | 0,48-0,59 | 0,47-0,58 | 0,5-0,65 | |
| ACA | PSV (cm/s) | 67-102 | 62-96 | 49-91 |
| EDV (cm/s) | 31-50 | 30-46 | 25-39 | |
| RI | 0,5-0,59 | 0,48-0,57 | 0,51-0,6 | |
| PCA | PSV (cm/s) | 50-78 | 45-73 | 41-73 |
| EDV (cm/s) |
21-37
|
21-35 | 17-31 | |
| RI | 0,48-0,56 | 0,48-0,56 | 0,49-0,66 | |
| VA | PSV (cm/s) | 46-76 | 38-74 | 38-62 |
| EDV (cm/s) | 23-43 |
18-40
|
14-29 | |
|
RI
|
0,44-0,57 | 0,44-0,57 | 0,48-0,63 | |
| BA | PSV (cm/s) | 48-80 | 49-82 | 37-65 |
| EDV (cm/s) | 26-43 | 19-40 | 13-25 | |
|
RI
|
0,46-0,56 | 0,46-0,56 | 0,5-0,62 | |
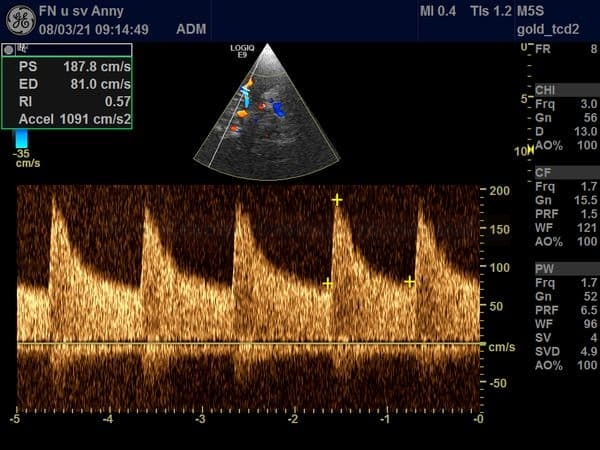
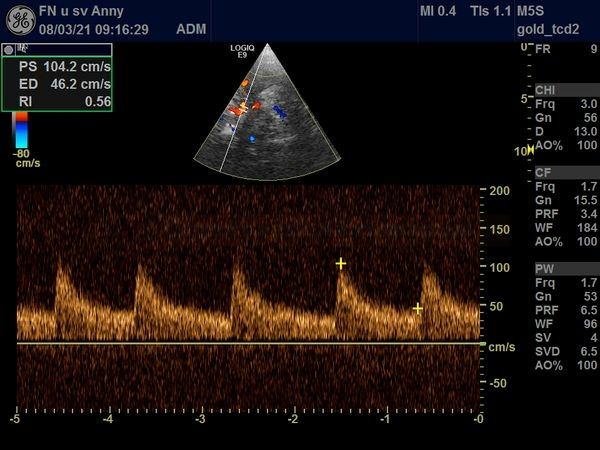
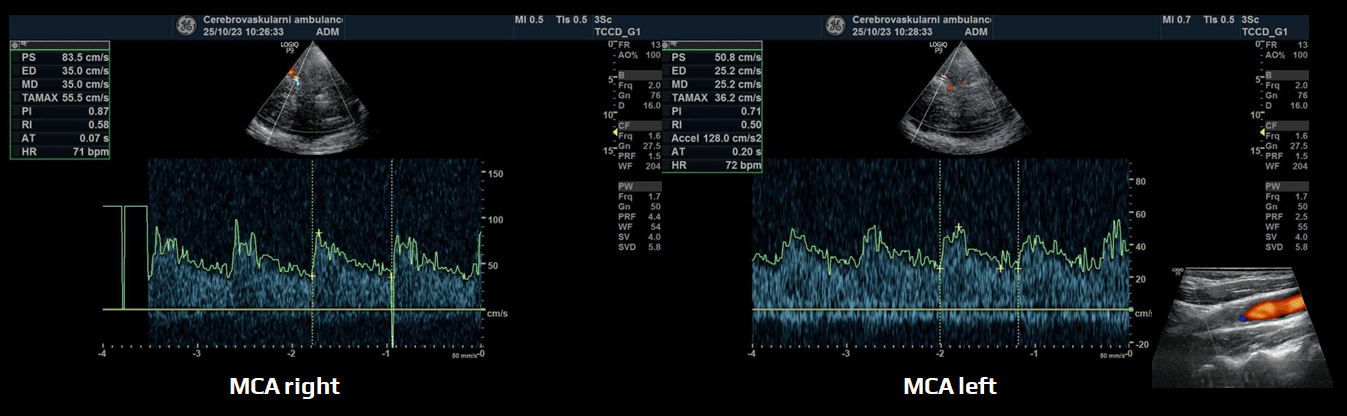
Assessment of arterial stenosis
- a multiparametric evaluation is necessary; an isolated PSV obtained from the stenotic segment is not sufficient
- prestenotic segment: a resistant (↑PI and RI) and decreased flow
- stenotic segment:
- poststenotic segment: decreased PSV, systolic acceleration, PI, and RI
| PSV ratio (stenosis / pre- or poststenotic segment) |
Stenosis (%) |
|
| mild stenosis | 1.3-2 | < 50% |
| moderate stenosis | 2-3 | 50-70% |
| severe stenosis | > 3 | > 70% |
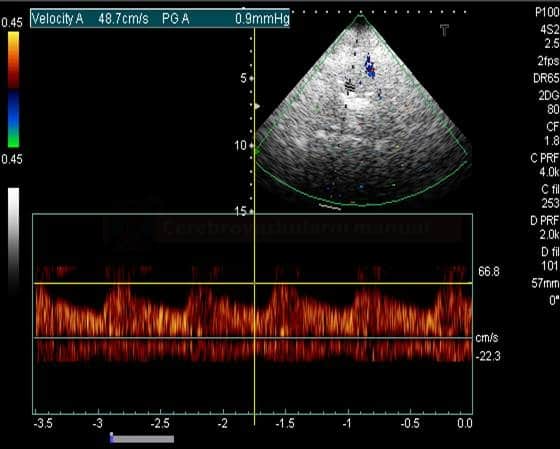
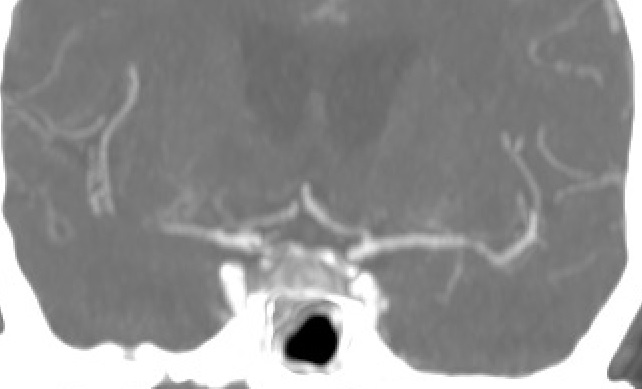
STENOSIS IN M2 SEGMENT OF THE MCA
STENOSIS IN THE M1 SEGMENT OF THE MIDDLE CEREBRAL ARTERY
Assessment of arterial occlusion
- transcranial Doppler (TCD or TCCD) is an ideal noninvasive, real-time bedside tool for the evaluation of cerebral vessels, particularly in the setting of an acute stroke
- strong correlation exists between TCCD and CTA
- an abnormal TCD/TCCD study, defined as either no or asymmetrical MCA flow, is associated with poor outcome
- direct signs of occlusion:
- indirect signs:
- assessment of basilar artery occlusion (BAO), especially of its distal segment, may be challenging
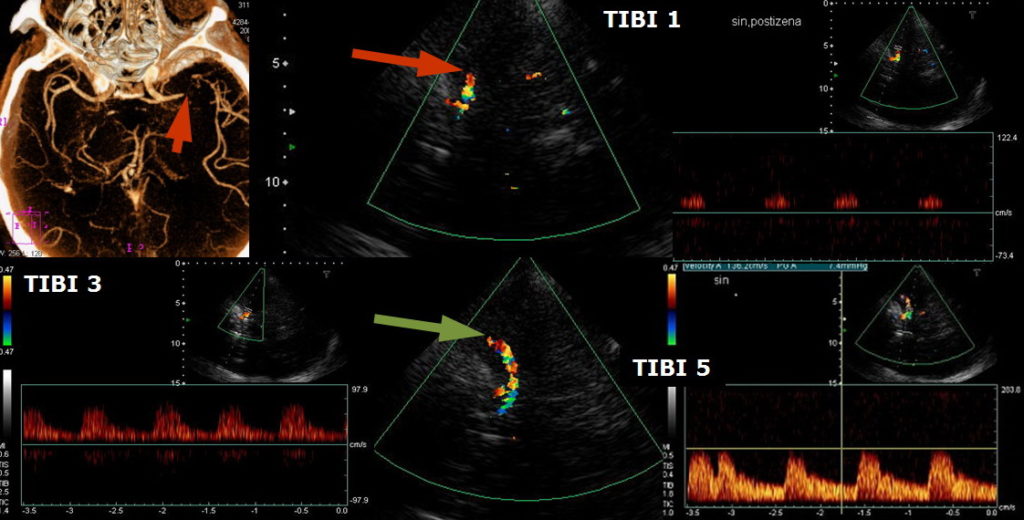
TIBI (Thrombolysis in Brain Ischemia)
- the TIBI classification was developed to grade residual flow
- it correlates with initial stroke severity, clinical recovery, and mortality in acute stroke patients
- no improvement in the residual flow correlates with the absence of early clinical recovery and increased mortality (Demchuk, 2012)
- no improvement in the residual flow correlates with the absence of early clinical recovery and increased mortality (Demchuk, 2012)
According to [Demchuk, 2001]
| Recanalization assessment [Clotbust, 2007] |
|
| Complete recanalization | TIBI 4-5 |
| Parcial recanalization | increase of TIBI by ≥1 grade (but not to 4 or 5) |
| Reocclusion | decrease of TIBI by ≤1 grade |
COGIF
Differentiation of TIBI grades 1-3 (minimal flow, blunted flow, dampened flow) may be difficult. The flow patterns of these grades not only reflect partial M1 recanalization but also the hemodynamic situation in other segments. The COGIF scoring system was designed to more clearly follow the recanalization process; it is exclusively based on known hemodynamic changes of the Doppler spectrum. The time course of grades during the serial examination must be encoded.
| Recanalization assessment | |
| Complete recanalization |
COGIF 4 |
| Partial recanalization |
improvement by ≥1 grade (but not to 4) |
| No change |
baseline COGIF grade persists |
| Worsening | decrease by ≥1 grade |
Transcranial findings in extracranial stenosis/occlusion
- ↓PSV and EDV
- ↓ PI, RI
- decreased systolic acceleration
- development of collateral circulation
- impaired cerebral vasomotor reactivity (CVR)