ISCHEMIC STROKE / VASCULITIS
Takayasu arteritis
Updated on 29/01/2024, published on 24/05/2023
Etiology
- Takayasu arteritis, also known as “pulseless disease, is a rare inflammatory disease primarily affecting the aorta and its major branches
- predominantly occurs in young oriental women (female-to-male ratio 8:1)
- etiology is unknown, but cell-mediated immune mechanisms are involved
- histology is similar to temporal (giant cell) arteritis
- inflammation begins with adventitial mononuclear infiltration
- later, mononuclear inflammation of the media may occur, accompanied by granulomatous changes
- onset typically in the first 3 decades of life
- timely recognition and appropriate management are essential for improving patient outcomes in Takayasu arteritis cases
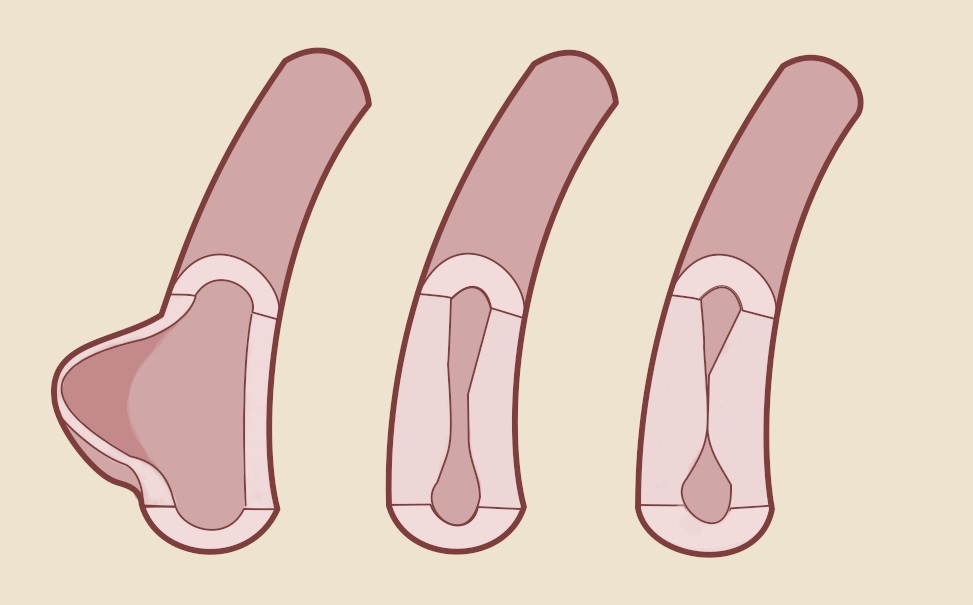
- inflammation leads to irregular thickening of the affected artery, which may result in:
- concentric stenosis or occlusion (initially with granulomatous changes of the media and adventitia, later involving intimal hyperplasia)
- thrombosis
- aneurysm formation (∼ 30% of patients)
Clinical presentation
Systemic symptoms
- most common in the early stages
- fatigue, fever, weight loss, night sweats, myalgia, and/or arthralgia
- many patients may present only with focal symptoms due to hypoperfusion of the affected organ or limb
CNS involvement
- symptoms of decreased cerebral perfusion
- dizziness and syncope (> 50%)
- subclavian steal syndrome
- ischemic stroke
- visual disturbances (visual field defects, amaurosis, retinal hemorrhages)
- intracerebral hemorrhage (most commonly due to aneurysm rupture)
Involvement of the heart and other arteries
- secondary renovascular hypertension
- involvement of limb arteries
- the diagnostic hallmark is a weakened pulse (“pulseless disease“); most patients have an absent pulse in at least one limb
- decreased blood pressure in one or both arms
- blood pressure difference > 20mm Hg between the left and right arm or between the arm and leg on the same side
- murmurs are often audible over the subclavian arteries (in the supraclavicular fossa), brachial arteries, carotid arteries, abdominal aorta, or femoral arteries
- limb claudication
- Takayasu arteritis is a chronic disease in which collateral circulation usually develops; ischemic ulcerations or gangrene are uncommon
- signs of aortic coarctation (e.g., hypertension, headache, leg claudication)
- cardiac symptoms
- angina pectoris / myocardial infarction (due to the narrowing of the coronary artery orifice)
- heart failure due to aortic regurgitation
- angina pectoris / myocardial infarction (due to the narrowing of the coronary artery orifice)
- pulmonary hypertension, pulmonary infarcts
Diagnostic evaluation
The diagnosis of Takayasu arteritis is based on:
- typical symptoms and signs (see above)
- typical imaging findings
- evidence of inflammation detected by blood tests
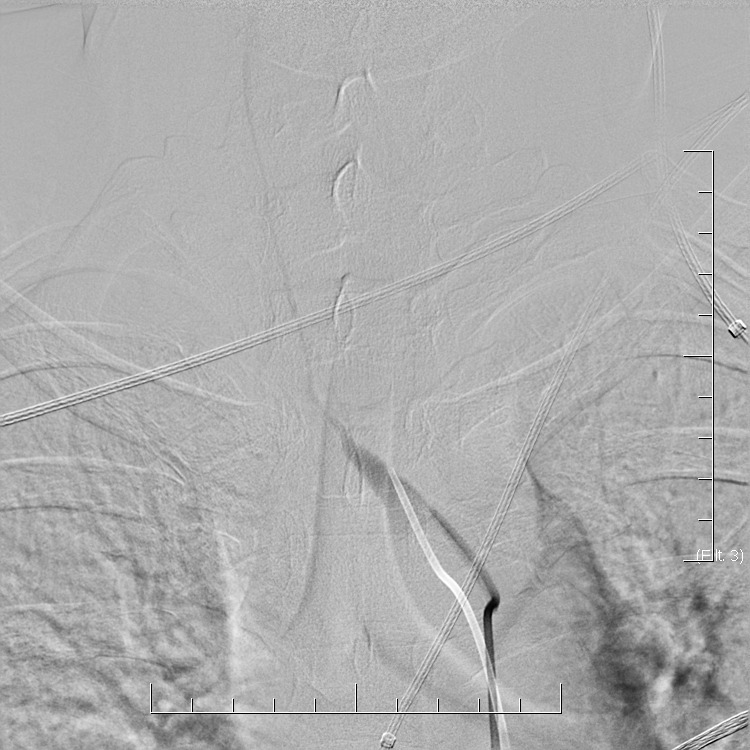
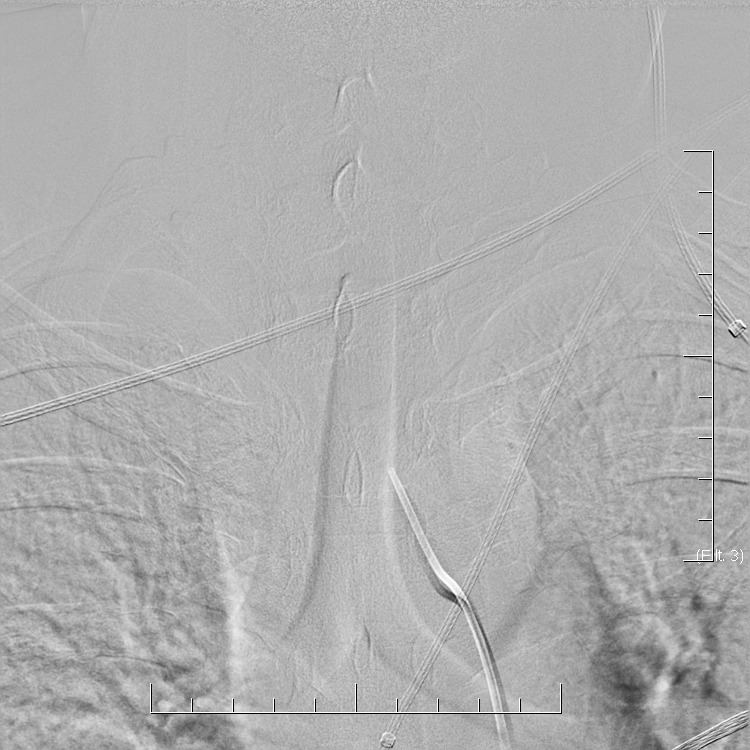
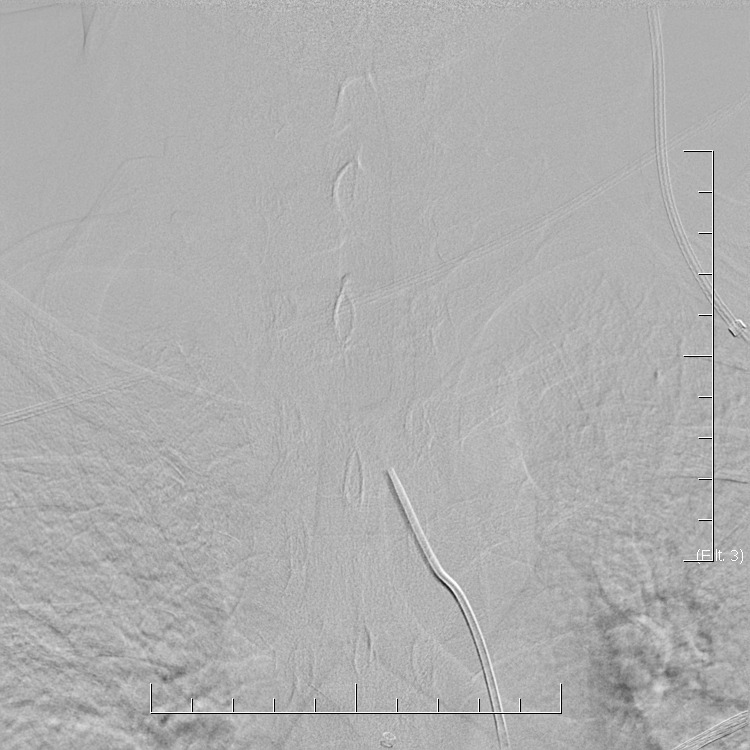
Imaging methods
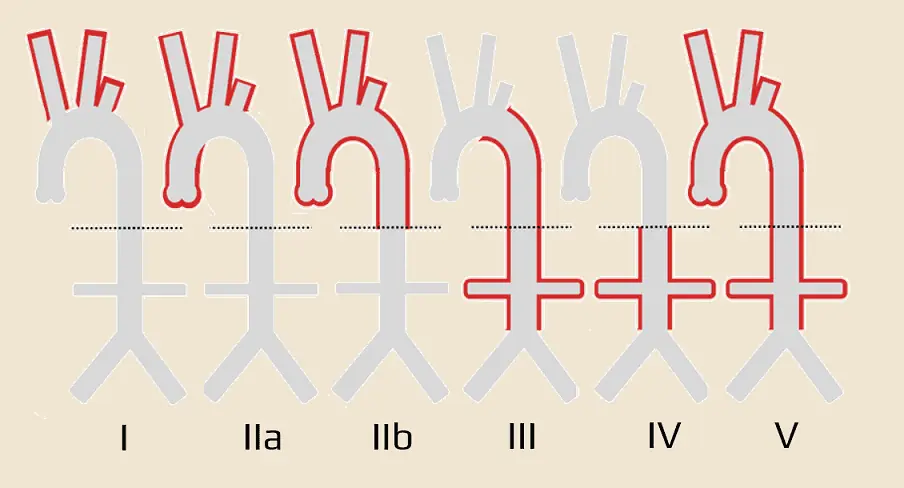
- characteristic findings in the aorta and its branches (always examine the descending aorta and renal arteries):
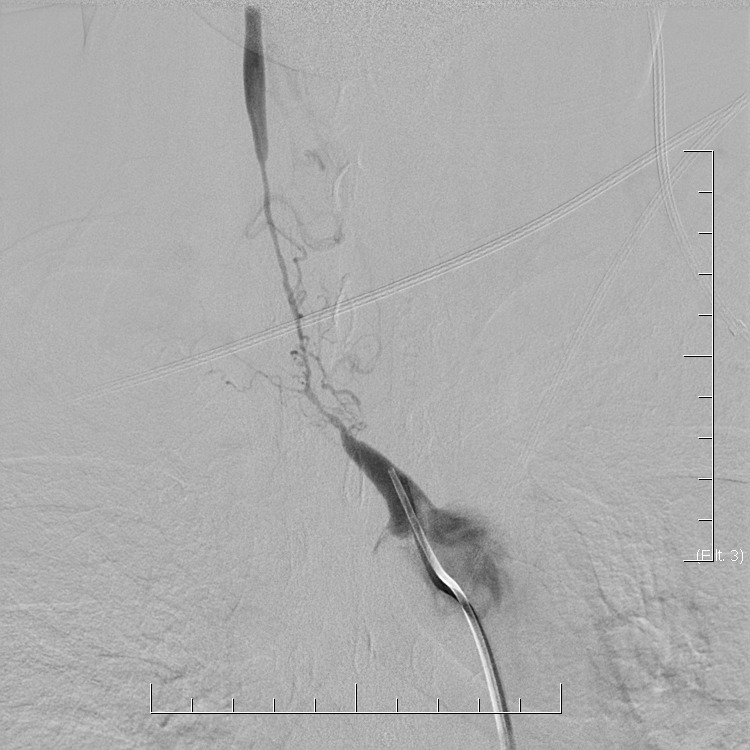
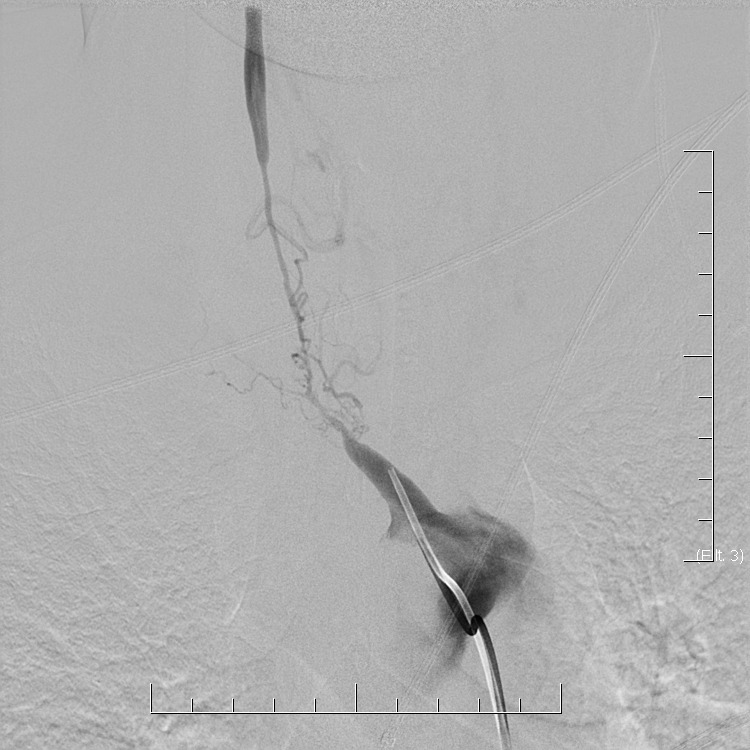
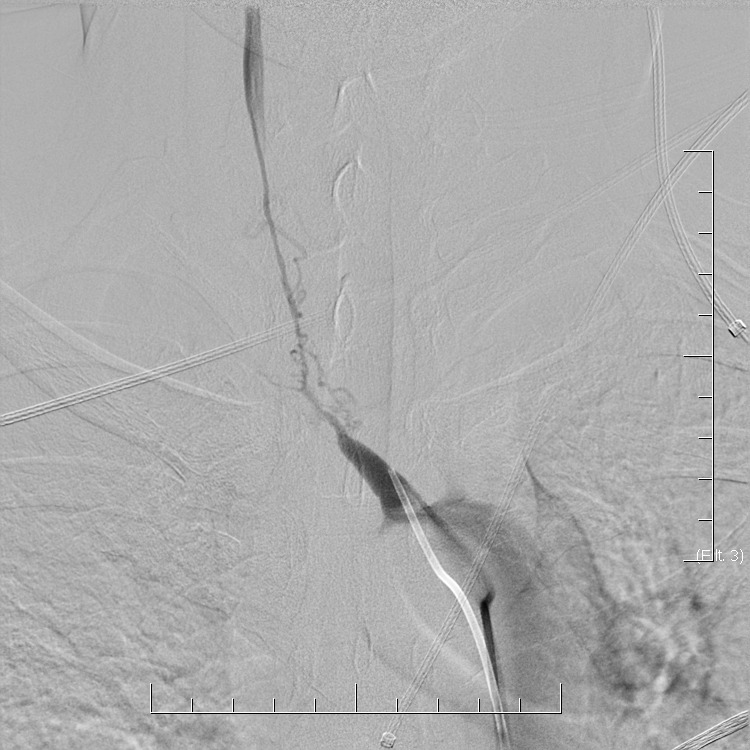
- segmental concentric stenoses/occlusions
- poststenotic dilatation
- collateral arteries as a compensatory response to restricted blood flow
- aneurysms
- aortic aneurysms, in particular, require careful monitoring due to their potential for rupture
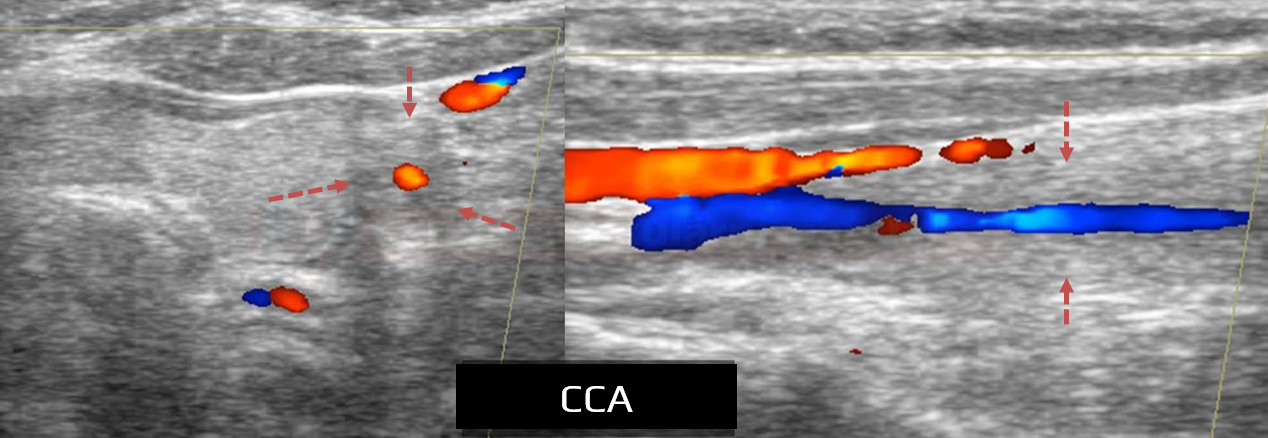
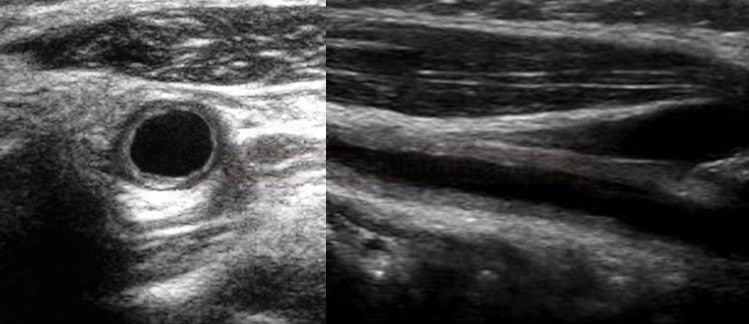
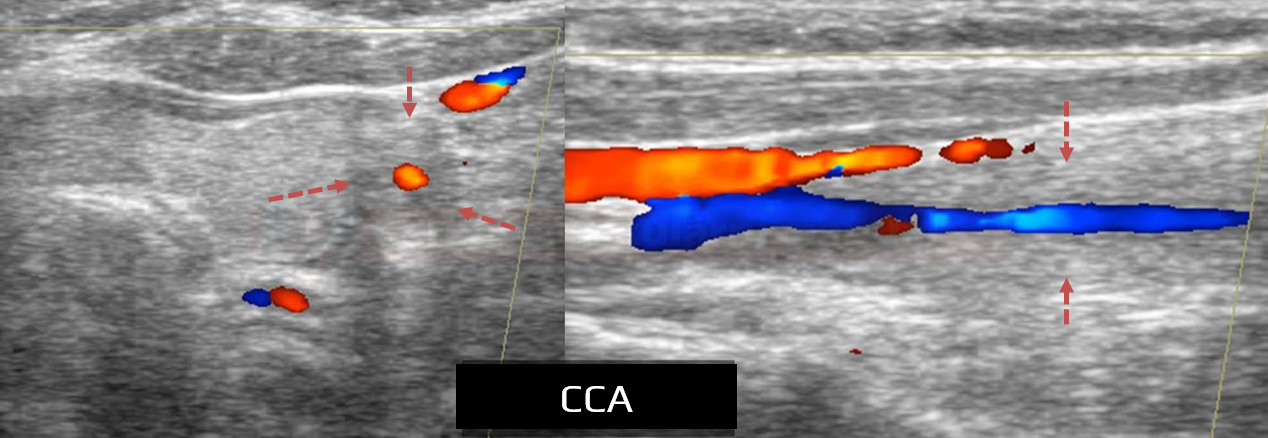
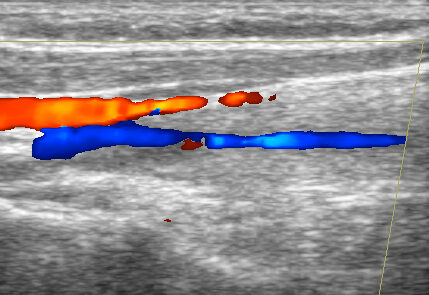
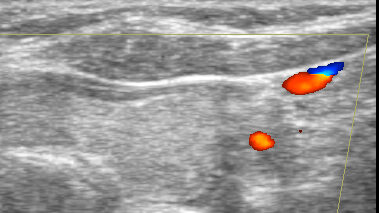
- carotid ultrasound – allow direct visualization of wall thickening, may assess the blood flow in distal segments and collaterals
- magnetic resonance imaging
- CTA
- DSA
- FDG PET/CT
- can demonstrate inflammatory arterial involvement
[Chrapko, 2015]
- may show hypometabolism in certain brain regions [Berlit, 2010]
- can demonstrate inflammatory arterial involvement
- Takayasu arteritis may progress silently even if clinical status and laboratory studies suggest remission ⇒ periodic vascular imaging is required
Blood tests
- tests are nonspecific
- ↑CRP (C-reactive protein), ESR (erythrocyte sedimentation rate) > 40mm (however, normal values do not exclude active disease)
- anemia of chronic disease (usually mild)
- leukocytosis
- elevated platelet count
- ↑ metalloproteinases MMP-2, MMP-3 and MMP-9
Blood pressure measurement
- BP should be measured in all extremities (both arms and both legs) to assess for potential discrepancies
- accurate measurement can be challenging
- if both subclavian arteries are affected, systemic BP can be measured only in the unaffected legs
- if both subclavian arteries are affected, and the patient has also coarctation of the descending aorta, and/or involvement of both iliac/femoral arteries, accurate noninvasive BP measurement is impossible ⇒ central arterial pressure measurement via angiography may be required to detect occult hypertension
- additional indicators of occult hypertension are:
- hypertensive retinopathy
- echocardiographic evidence of concentric left ventricular hypertrophy
- severe hypertension may cause complications that may be mistaken for symptoms of vasculitis ⇒ a comprehensive evaluation and accurate diagnosis are essential
Diagnostic criteria and classification
|
Diagnostic criteria of Takayasu arteritis
( American College of Rheumatology, 2022) |
|
|
Absolute requirements
|
|
Additional clinical criteria
|
|
Additional imaging criteria
|
|
| A score of ≥ 5 points is needed to classify as Takayasu arteritis |
|
Diagnostic crieteria of Takayasu arteritis
( American College of Rheumatology, 1990) |
|
|
Typical clinical complaints lasting > 1 month
|
major |
|
minor |
|
minor minor minor |
Proof of arterial involvement
|
major
major
minor
minor minor
minor
minor
minor
minor
|
High probability of Takayasu arteritis
|
|
Differential diagnosis
- atherosclerosis
- age > 40 years
- more common in men
- lesions in typical locations
- fibromuscular dysplasia (FMD)
- rarely affects the subclavian artery; almost never the aorta
- temporal arteritis (does not affect CCA and subclavian artery)
- vascular infections
- syphilitic aortitis (with typical aortic calcifications)
- tuberculous, fungal aortitis
- neurofibromatosis type I
- idiopathic inflammatory conditions (e.g., ankylosing spondylitis with aortitis, Behçet syndrome, sarcoidosis)
Stroke prevention
- antiplatelet therapy [Souza, 2010]
- treatment of hypertension (problem with BP assessment in cases of subclavian artery stenosis/occlusion)
- low sodium diet
- stenting or bypass surgery in cervical artery lesion
- procedures performed during remission have better outcome
- procedures performed during remission have better outcome
Immunosuppressive therapy
- start with PREDNISONE 1 mg/kg, then gradually taper over several weeks; target maintenance dose should be individualized (based on inflammatory markers and clinical status)
- after remission is achieved (decrease in ESR and CRP, correction of anemia), maintain dose at 5-10 mg/day for 1-2 years
- rapid tapering may lead to relapse
- prevention of osteoporosis is necessary during long-term corticosteroid treatment – e.g., by administering Caltrate PLUS twice daily or Kombi-Kalz 1000/880 once daily
- whenever possible, combine corticosteroids with immunosuppressants or immunomodulators to enhance treatment efficacy
Immunosuppressants – cytostatics
- approximately 50-70% of patients require adjunctive treatment with immunosuppressive drugs
- for less aggressive forms, consider the following:
- azathioprine (IMURAN) 1-2 mg/kg/day
- mycophenolate (CELLCEPT)
- methotrexate is administered once weekly (due to its potential for toxicity)
- starting dose: 7.5-15 mg once weekly
- the dose may be gradually increased as needed and tolerated, with a usual maximum of ~ 20-25 mg per week
- may help improve disease control and reduce corticosteroid dose
- monitor patients for potential side effects, including hepatotoxicity, bone marrow suppression, and pulmonary toxicity
- supplementation with folic acid is standard to mitigate some of the side effects
- cyclophosphamide
- typical dose 1-2 mg/kg per day
- intravenous pulse of 500-1000 mg/m² body surface area, administered once a month
New immunosuppressive agents [Mekinian, 2015]
- biologically targeted treatments
- IL-6 receptor monoclonal antibody – tocilizumab (ROACTEMRA)
- used in the treatment of various autoimmune and inflammatory conditions
- it has been investigated as an alternative or adjunctive therapy for Takayasu arteritis, especially in cases resistant to conventional treatment
- results are promising but more research is needed to establish its long-term safety and efficacy
- TNF-alpha blockers – reserved for conditions resistant to standard therapies
Reconstructive procedures
- vascular procedures for organ-threatening ischemia, such as stenting or bypass surgery (indicated not only for cervical artery involvement but also for limb, mesenteric, and renal artery disease)
Follow up
Laboratory tests
- CRP unreliable
- ESR – decline during remission present in ∼ 60% of cases ⇒ unreliable marker [Matsuyama,2003]
- metalloproteinases [Matsuyama,2003]
- MMP-2 diagnostic > 800 ng/mL
- relapse – MMP-3 > 100 ng/mL and MMP-9 > 75 ng/mL
Imaging methods
- vascular lesions may progress even if clinical and laboratory findings suggest remission
- periodic vascular imaging to monitor stenosis grade and wall width/enhancement is essential
- MRI of the neck (with black blood sequences) + MRA
- neurosonology for non-invasive flow dynamics evaluation
- CT angiography
Prognosis
- the clinical course is usually relapsing-remitting or chronic/progressive
- despite therapy, the prognosis is uncertain and disease progression is frequently observed
- despite combined immunosuppressive therapy, restenosis of intervened arterial segments is common