ISCHEMIC STROKE / CLASSIFICATION AND ETIOLOGY
MELAS
Mitochondrial encephalopathy, lactic acidosis, and stroke-like episodes
Updated on 14/01/2024, published on 10/05/2023
Definition
- MELAS (mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes) is a mitochondrial multisystem disease primarily affecting the nervous system and muscles
- one of the most common mitochondrial diseases, with an estimated incidence of 1 in 4000
- both genders are equally affected, but only women can pass on the condition to their children
- presents in children or young adults (onset in a wide range of 2 -40 years) as episodes of migraine-like headache, encephalopathy, myopathy, and focal neurological deficits
- several MELAS-associated point mutations have been described
- most common is the 3243A>G mutation in the MTTL1 gene in mitochondrial DNA encoding tRNALeu
- most cases show maternal inheritance
- histopathologic examination of the brain shows spongiform encephalopathy, characterized by necrosis, neuronal loss, gliosis, and microcystic formations (status spongiosus) in the cortex
- calcifications in the basal ganglia are present in almost half of the cases
Clinical presentation
- children with MELAS often have normal early psychomotor development until the onset of symptoms between the ages of 2 and 10
- infant onset is possible with growth retardation and progressive deafness
The presence of at least two of the three additional criteria is required to confirm the diagnosis of MELAS:
The disease usually manifests at the end of the first decade of life (ranging from 2 to 40 years of age) |
Encephalopathy, stroke-like episodes
- the most common and usually initial symptom is a migraine-like headache with vomiting (90%)
- epileptic seizures (85%)
- focal or generalized, with no syndrome-specific semiology or EEG findings
- higher rates of drug-resistant epilepsy are reported
- “stroke-like” episodes are often accompanied by headaches and epileptic seizures
- hemiparesis, aphasia, and cortical visual defects (hemianopsia or cortical blindness); stroke-like episodes result in gradual impairment of neurologic function
- attacks resemble ischemic vascular events, but they do not correspond to typical vascular territories
- encephalopathy with mental retardation occurs in > 50% of cases
- encephalopathy may be exacerbated by valproate, which is used as an antiepileptic drug or for migraine prophylaxis
- sensorineural hearing loss (25%)
Systemic symptoms
- small figure
- retinal pigmentary degeneration – a progressive loss of vision due to damage to the retina
- cardiomyopathy and cardiac conduction disorders
- diabetes mellitus
- hirsutism
- nephropathy
- chronic fatigue
Diagnostic evaluation
Laboratory tests
- elevated resting lactate in serum and CSF with a dramatic increase after exercise
- increased CSF protein
- genetic testing
- screening for mtDNA mutations can be performed from blood leukocytes or muscle tissue
- genetic evaluation from blood should be done first to eliminate the need for muscle biopsy in most cases
- muscle biopsy
- histochemical examination of muscle shows typical “ragged red” fibers on SDH and trichrome staining
- in contrast to KSS and MERRF, only a minimum of fibers are COX-negative
- the specific histochemical feature of MELAS is evidence of SDH-positive vessels due to the mitochondrial proliferation
- ultrastructural examination confirms mitochondrial proliferation and mitochondrial morphological abnormalities
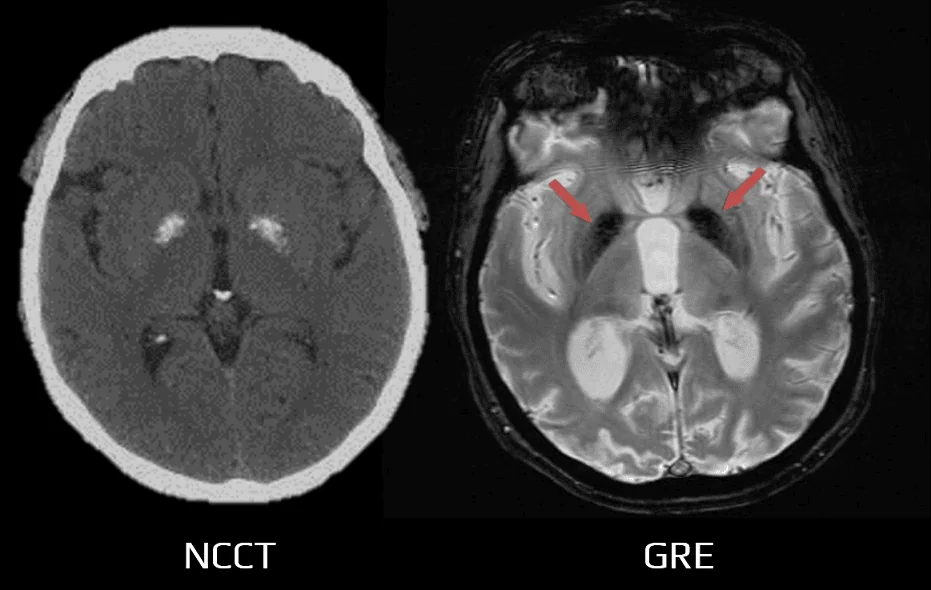
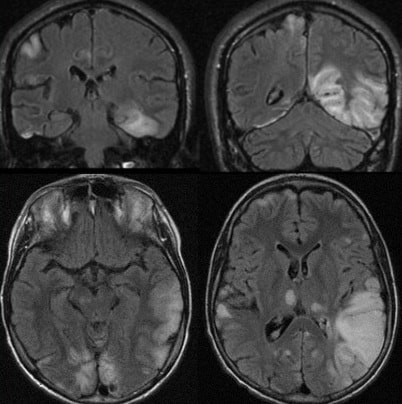
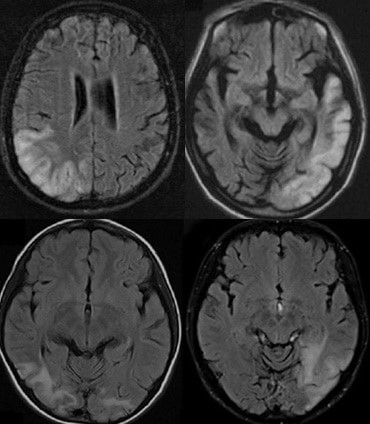
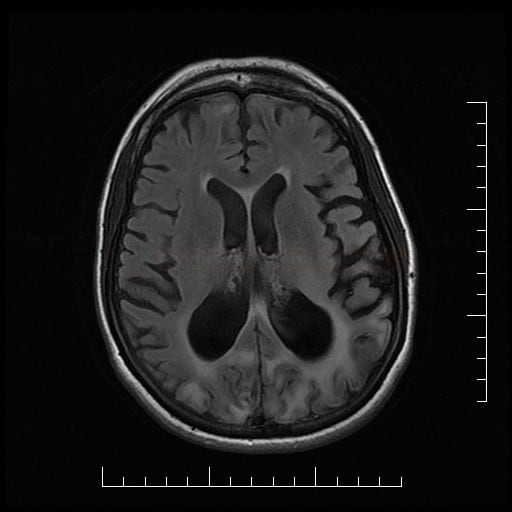
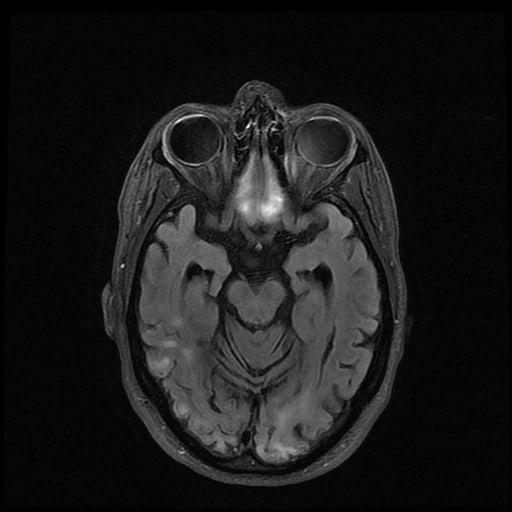
Neuroimaging
- brain CT/MRI
- multifocal infarct-like cortical lesions with disrespect to known vascular territories and initial preference for the posterior brain regions (occipital or parietal lobes)
- cerebellum, basal ganglia, and thalamus may also be involved
- MRI findings may fluctuate or resolve more quickly than typical stroke, and the ADC is not always decreased and may instead be increased or show mixed signal
- cerebral atrophy
- calcifications in the basal ganglia, mainly in elderly patients (50%)
- multifocal infarct-like cortical lesions with disrespect to known vascular territories and initial preference for the posterior brain regions (occipital or parietal lobes)
- MR spectroscopy – elevated lactate peak in affected and even unaffected brain areas
Other methods
- ECG – possible signs of preexcitation or partial block
- much less common and less pronounced than in KSS
- much less common and less pronounced than in KSS
- EMG – myopathic pattern
Differential diagnostics
- other causes of stroke in young persons under age 40
- other mitochondrial disorders:
- MERFF (Myoclonus epilepsy associated with ragged red fibers)
- hearing loss
- visual disturbance secondary to optic atrophy
- characteristic myoclonic seizures
- Kearn-Sayre
-
chronic progressive external ophthalmoplegia
-
atypical retinitis pigmentosa
-
retinal pigmentary degeneration
- more pronounced cardiac manifestation
-
- Leigh syndrome
- primarily affects infants and young children ( 3 months to 2 years; rarely, it can occur in teenagers and adults
- generalized weakness, lack of muscle tone
- episodes of lactic acidosis, which can lead to impairment of respiratory and kidney function
- MERFF (Myoclonus epilepsy associated with ragged red fibers)
- vasculitis
- CADASIL (subcortical lesions, external capsule, and temporal poles)
- CADASIL is caused by mutations in the NOTCH3 gene, which encodes a protein involved in the development of blood vessels
| Content available only for logged-in subscribers (registration will be available soon) |
Management
- effective causal treatment to stop disease progression is not known; supportive measures (social worker assistance, physical and occupational therapy) are essential to improve the quality of life
- a partial effect of coenzyme Q10, riboflavin, has been described
- L-arginine shows promising results [Koga, 2006]
- IV administration reduces the severity of symptoms when used in acute attacks (e.g., status epilepticus); dosage is adjusted according to arginine levels (ref. interval 45-130 umol/L) – ARDEAELYTOSOL 21% + 500mg Glu 5% 20 mL/h [Toribe, 2007] (Coga, 2018)
- oral L-arginine 4x1g per day prolongs the interval between stroke-like attacks (Lekoubou, 2011) (AHA/ASA 2021)
- IV administration reduces the severity of symptoms when used in acute attacks (e.g., status epilepticus); dosage is adjusted according to arginine levels (ref. interval 45-130 umol/L) – ARDEAELYTOSOL 21% + 500mg Glu 5% 20 mL/h [Toribe, 2007] (Coga, 2018)
- idebenone
- a synthetic analog of coenzyme Q10 that acts as an antioxidant and has the potential to improve mitochondrial oxidative metabolism
- further investigation through clinical studies is required
- epileptic seizures respond favorably to antiepileptic drugs (beware of valproate encephalopathy)
Prognosis
- MELAS is a progressive disease that tends to worsen following each “stroke-like” episode
- these episodes cause cumulative damage to the brain over time
- while the severity and frequency of episodes can vary among individuals, MELAS typically follows a progressive course
- the prognosis varies depending on the severity of symptoms and age of onset; death may occur in the first decades of life, especially in early clinical manifestations
- death is usually caused by cardiopulmonary failure or a malignant course of status epilepticus
- the average lifespan for people with MELAS is reduced, but many people with MELAS live into their 40s or 50s