SUBARACHNOID HEMORRHAGE
Diagnosis of subarachnoid hemorrhage
Updated on 29/04/2024, published on 30/03/2021
- the diagnosis of SAH should be considered in any patient presenting with a severe, sudden-onset, or rapidly worsening headache
- deciding which patients require evaluation for SAH is often challenging in emergency care
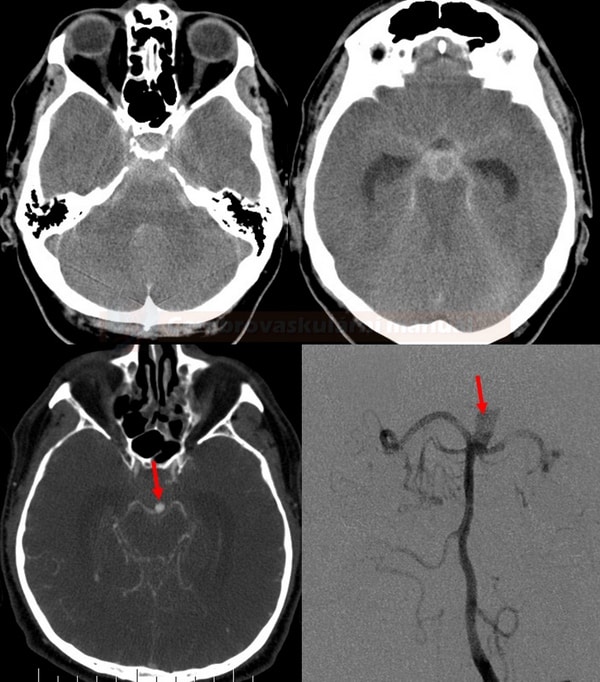
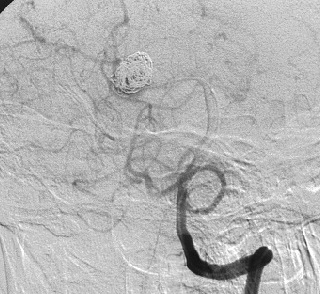
- imaging methods can confirm the diagnosis of subarachnoid hemorrhage (SAH)
- the standard imaging method is computed tomography (CT), followed by CT angiography (CTA) to detect or exclude a source of bleeding
- if CT scan is negative, a lumbar puncture (LP) with proper cerebrospinal fluid (CSF) analysis is performed
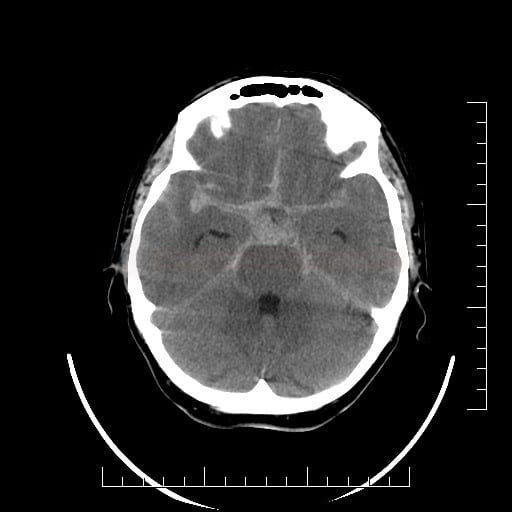
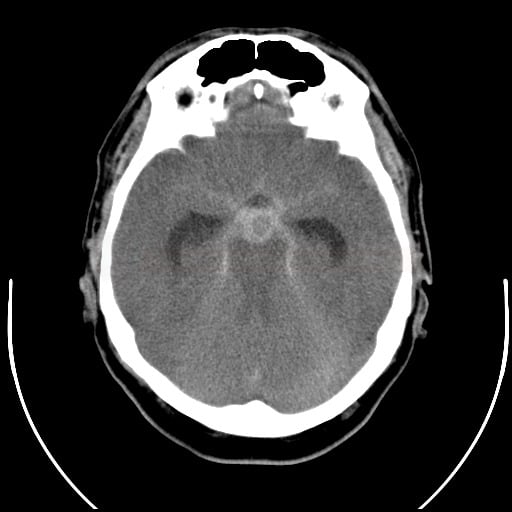
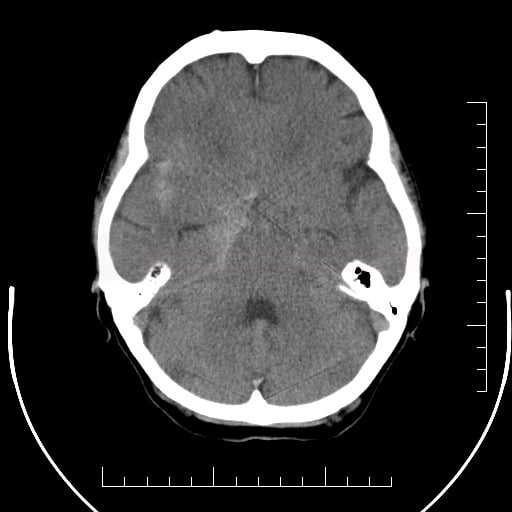
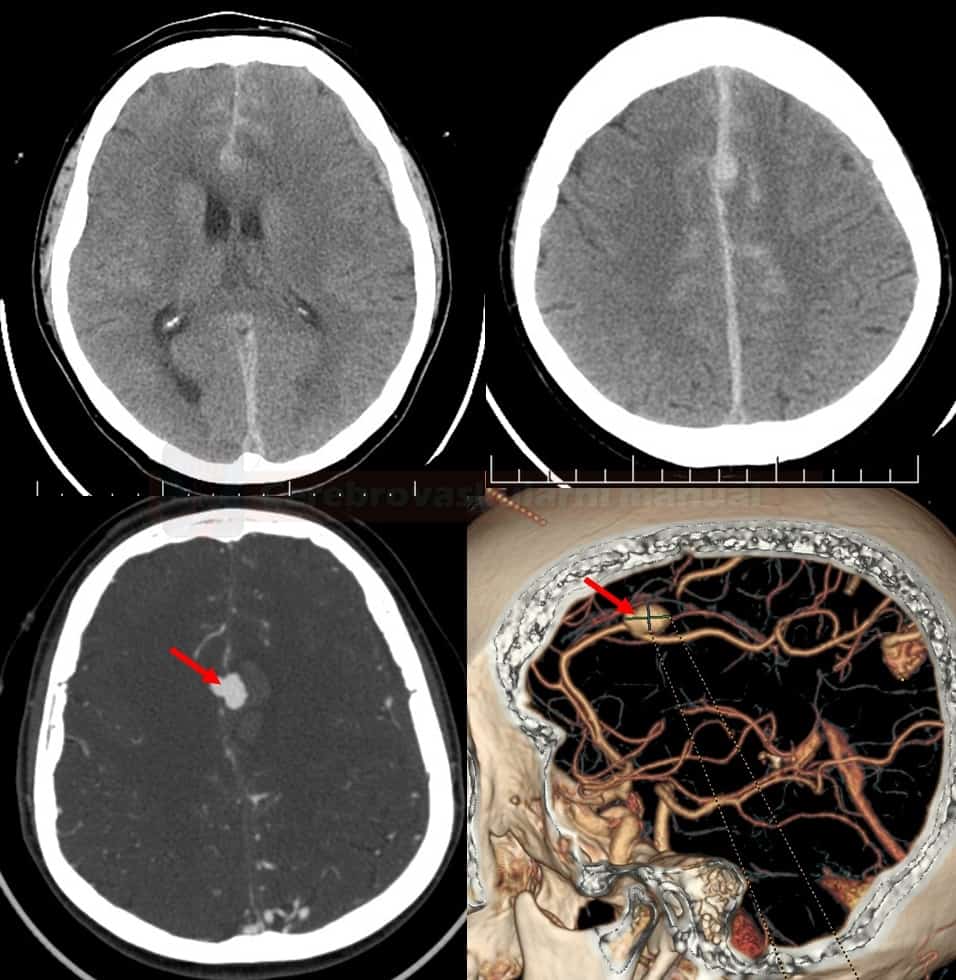
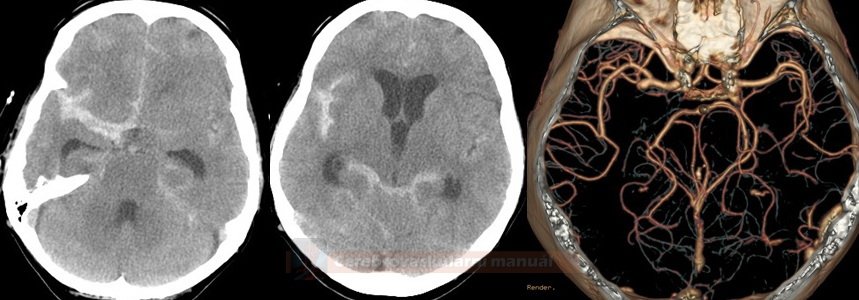
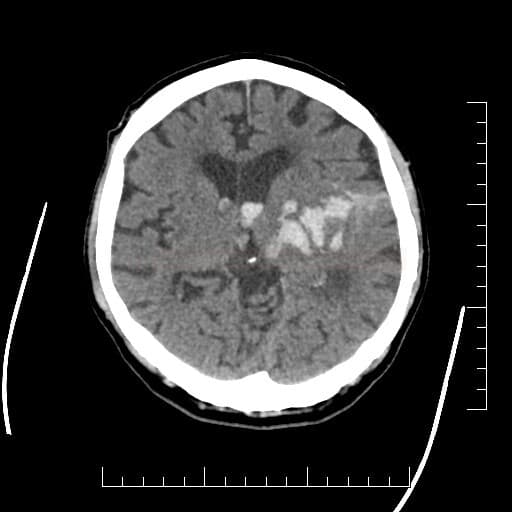
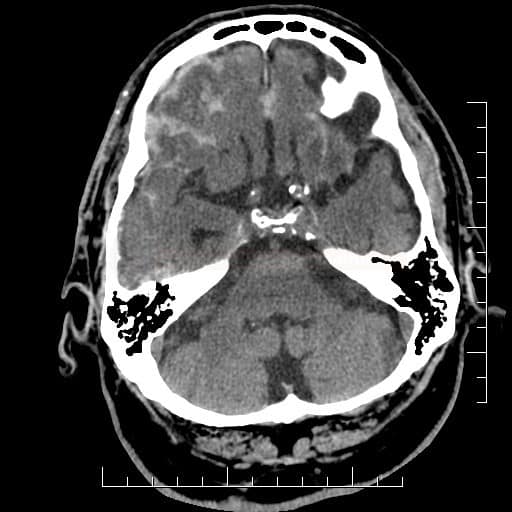
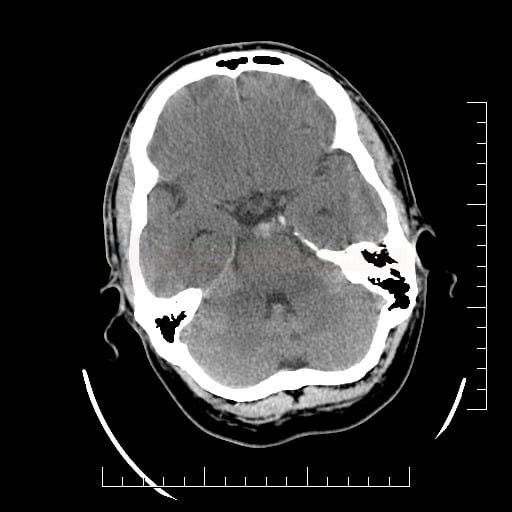
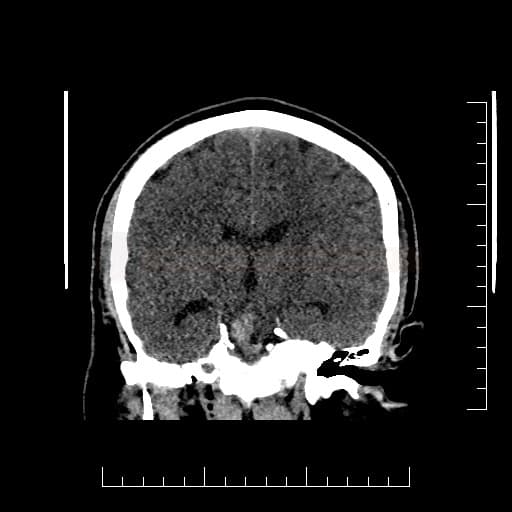
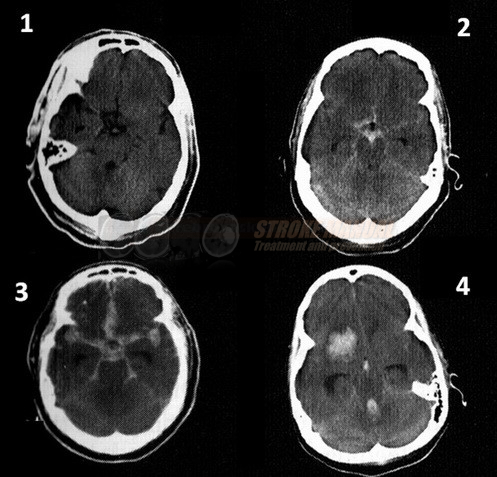
Computed tomography
- SAH is manifested by increased density in the subarachnoid (SA) space → Fisher scale grading
- SAH is found in typical locations (see below) but may be restricted to convexity (hyperdense strips in sulci) → nontraumatic convexal SAH
- SAH is found in typical locations (see below) but may be restricted to convexity (hyperdense strips in sulci) → nontraumatic convexal SAH
- CT scan sensitivity for SAH is 90-95% within the first 24 hours, depending on the amount of blood
- CT scan sensitivity decreases over time – to 70% by day 3 and to < 50% a week later
- presence of a significant amount of blood on a CT scan after one week strongly suggests rebleeding
- CT scan sensitivity decreases over time – to 70% by day 3 and to < 50% a week later
| SAH location |
Aneurysm location |
| Sylvian fossa | MCA |
| interhemispheric fissure |
AComA, ACA |
| suprasellar cistern |
distal ICA |
| perimesencephalic cistern | top basilar artery |
| 4th ventricle | PICA |
Combination of SAH and intraparenchymal bleeding
- SAH may be accompanied by intraparenchymal hematoma (especially in MCA aneurysms) or by intraventricular bleeding
- conversely, a primary ICH from AVM or in basal ganglia can secondarily extend into the subarachnoid space resulting in secondary SAH
Convexial SAH
- traumatic
- bleeding from a dural fistula
- rarely, intracranial venous thrombosis may initially manifest as convexal SAH [Sharma, 2010] [Oppenheim, 2005]
- rupture of a dilated feeding vein due to retrograde intravenous hypertension
- secondary rupture of a hemorrhagic infarction into the subarachnoid space
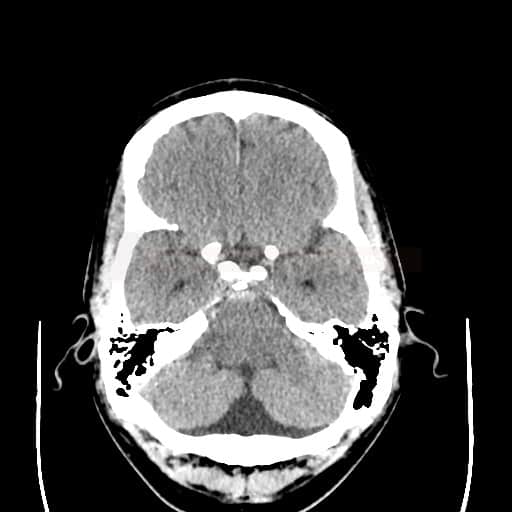
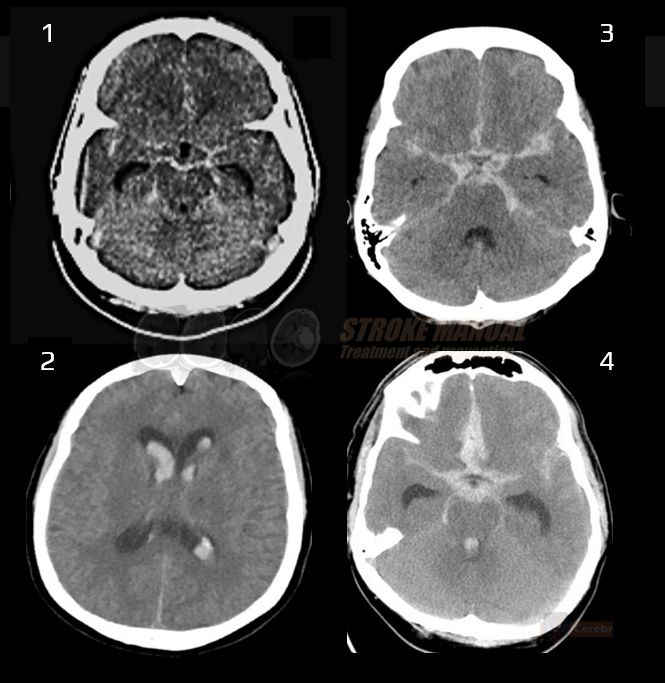
Perimesencephalic SAH (PMSAH)
- blood is present only in the (pre)pontine and interpeduncular subarachnoid cisterns
- it may extend into the suprasellar cistern or to the medial (not lateral) Sylvian fissure and proximal interhemispheric fissure
- accounts for ~ 5-10% of all SAHs
- mainly low-pressure bleeding, presumably caused by rupture of small perimesencephalic and/or prepontine veins → normal CTA/DSA
- favorable clinical course (HH usually I-II), low recurrence risk (~1%)
- the minority of MPSAHs are caused by vertebrobasilar aneurysms or AVM rupture
- if NCCT criteria are met and CTA is negative, DSA is not required
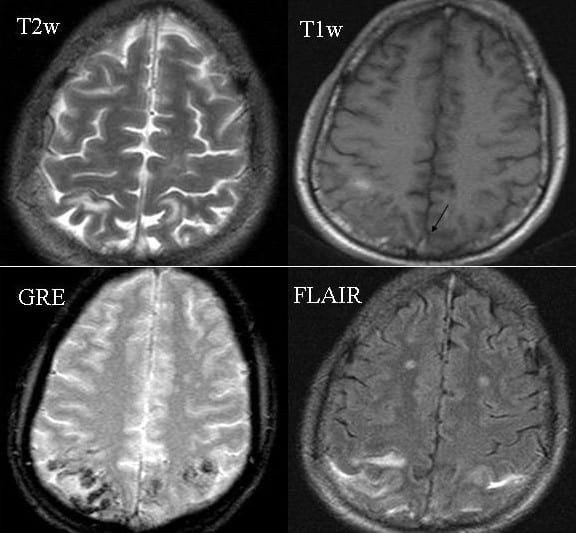
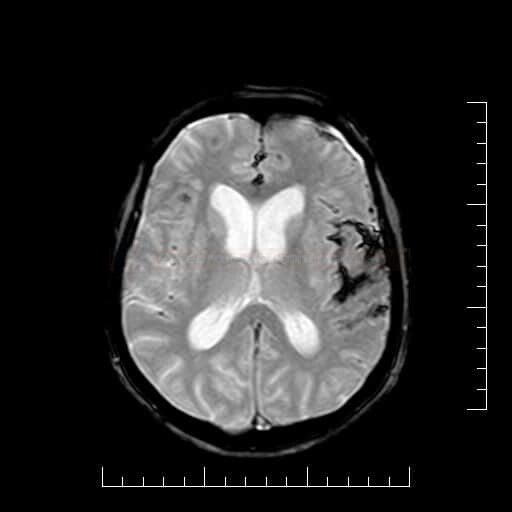
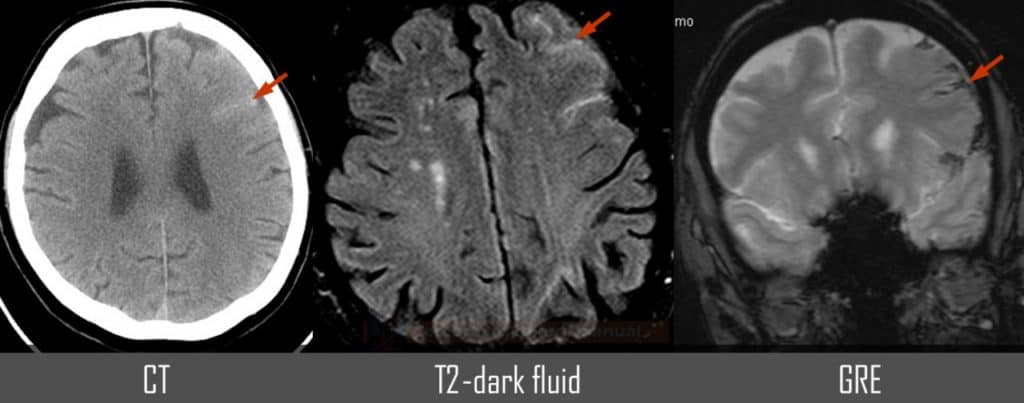
Magnetic resonance imaging (MRI)
- MRI is sensitive to subarachnoid blood and can visualize it within the first 12 hours
- T2, FLAIR – hyperintense
- T1 – isointense to hypointense
- GRE/SWI – hypointense
- supersensitive to blood products
- MRI can also detect thrombosed aneurysms, sometimes not visible on angiography
- MR angiography and MR venography can detect an aneurysm or other sources of bleeding
- DWI may show potential ischemic changes
- both early and delayed (DID associated with vasospasm)
Cerebrospinal fluid analysis
- it is recommended to wait ≥ 12 hours from the onset of presenting symptoms before performing a lumbar puncture (LP) [Beetham, 2003]
- if performed earlier, the CSF can appear “artificially normal”
- rapid analysis of collected CSF is required
- bedside multiple-tubes test is useful
- if there is bleeding due to the puncture, the CSF should clear when collected in multiple tubes
- xanthochromia is evidence of previous bleeding
- risk of early SAH recurrence as a complication of lumbar puncture is negligible
- NCCT may miss some SAH cases; cerebrospinal fluid (CSF) spectrophotometry should be performed in those patients with negative CT scans or those who present several days after suspected hemorrhage
- spectrophotometry provides information about the presence of hematogenous pigments in the CSF and helps differentiate SAH from artificial bleeding (sample must be delivered and processed immediately and protected from light)
- under physiological conditions, the spectrophotometric curve of CSF is flat or slightly elevated
- CSF xanthochromia (yellowish discoloration) can be caused by oxyhemoglobin or bilirubin
- hemolysis occurs 2 hours after erythrocytes enter the CSF ⇒ oxyhemoglobin – oxyHb-type curve (wavelength 410-418nm) can be detected
- the presence of oxyhemoglobin alone is not proof of SAH; it may be increased because of in vitro hemolysis of red cells introduced into the CSF during lumbar puncture
- bilirubin can be detected after ~9-15 hours (wavelength 450-460nm) [Beetham, 2003]
- the presence of bilirubin in CSF is macroscopically manifested by a distinctly yellow or at least yellowish color (xanthochromia)
- bilirubin is formed only in vivo and rules out a bloody tap
long bilirubin (460 nm) – SAH, hemolytic anemia - short bilirubin (430 nm) – SAH, obstructive icterus
- the presence of bilirubin in CSF is macroscopically manifested by a distinctly yellow or at least yellowish color (xanthochromia)
- initially, the oxyHb peak dominates (oxyHb-type curve), bilirubin gradually increases (oxyHb-Bi type curve), and later bilirubin dominates (Bi-type curve)
- the CSF may contain bilirubin for up to 2 weeks – in a patient with a severe headache of several days’ duration and no blood on a CT scan, the detection of xanthochromia/bilirubin is significant
- it is important to rule out passive transfer of bilirubin from the plasma
- therefore, a serum/plasma sample from the patient is also required
- therefore, a serum/plasma sample from the patient is also required
- cytology is useful only when monocyte activation and erythrocyte phagocytosis have begun
- aseptic meningitis is usually present at later stages of SAH
- cytology helps to distinguish repeated bleeding
- this is indicated by a disruption in the sequence of erythrocytes phagocytosis and the gradual appearance of hematogenous pigments in macrophages
- simultaneous phagocytosis of intact erythrocytes with hemosiderin granules or simultaneous appearance of hematoid crystals with erythrocyte digestion may be observed
Erythrocyte phagocytosis
recent bleeding, erythrophages appear (≥ 6 h from bleeding)
↓
Digestion of phagocytosed erythrocytes
erythrocytes decolorization and disintegration, optically empty vacuoles are present
↓
Hemosiderin
iron-containing hematogenous pigment, present in siderophages (from day 4-5)
↓
Hematoidin crystals
hematogenic pigment forming rhomboid crystals in macrophages
may be present extracellularly (after macrophage death) (~ from day 13)
FAQs
- the diagnosis usually involves a CT scan of the head, which is effective in detecting blood in the subarachnoid space
- if the CT scan is inconclusive, a lumbar puncture (spinal tap) may be performed to look for blood in the cerebrospinal fluid
- a CT scan should be performed as soon as possible, ideally within the first few hours after symptom onset, for the highest sensitivity in detecting a subarachnoid hemorrhage
- MRI, particularly fluid-attenuated inversion recovery (FLAIR) and gradient echo (GRE) sequences, can be used to diagnose SAH
- MRI is typically more sensitive than CT for subacute or chronic hemorrhage
- a lumbar puncture is particularly useful when the CT scan is negative but clinical suspicion remains high. It can detect blood in the cerebrospinal fluid that might not be visible on a CT scan, especially in cases of minor hemorrhages.
- yes, SAH can be misdiagnosed, especially if symptoms are mild or atypical. Misdiagnosis can occur in emergency settings if the symptoms are attributed to less serious conditions like migraine or tension headache
- blood tests are not available to diagnose subarachnoid hemorrhage