INTRACEREBRAL HEMORRHAGE / VASCULAR MALFORMATIONS
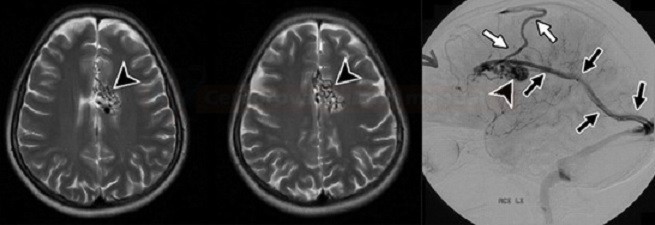
Cerebral arteriovenous malformation (AVM)
Updated on 29/02/2024, published on 23/04/2021
- brain AVMs are congenital developmental defects (present in about 1.4-4% of the population); they are likely to grow over time ( AVMs are diagnosed at a mean age of 31 years)
- there is an AD form of hereditary hemorrhagic telangiectasia (HHT)/Osler-Weber-Rendu (with a combination of AVM + telangiectasia)
- there is an AD form of hereditary hemorrhagic telangiectasia (HHT)/Osler-Weber-Rendu (with a combination of AVM + telangiectasia)
- AVM consists of an abnormally enlarged feeding artery and draining veins, between which lies a conglomerate of A-V junctions closely associated with the brain parenchyma (nidus)
- feeding arteries (one or more) are enlarged and tortuous; in 10-20% of cases, an aneurysm develops, which is often the source of bleeding/rebleeding
- in the nidus, there are abnormal arteries and veins without capillaries (arteries are directly connected to veins)
- intranidal aneurysm is frequent (up to 50%)
- draining veins (one or more) are tortuous, dilated, may cause mass effect, venous aneurysms (venous pouches) may also be seen
- if the transition between the feeding artery and the draining vein is direct (without nidus), it is called arteriovenous fistula (another type of cerebral vascular pathology)!
- localization of AVM
- supratentorial: ~85% (2/3 superficial, 1/3 deep)
- infratentorial: ~15%
- AVMs are solitary in most cases (multiple in < 5% of cases)
- multiple AVMs are present in hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu syndrome) or Wyburn-Mason syndrome (craniofacial arteriovenous metameric syndrome)
- AVMs are often discovered incidentally on CT/MRI scans performed for other reasons
- parts of the AVM have a histologically abnormal structure, gliosis or calcification are found around the lesion
- a clinical manifestation usually occurs between 20-40 years of age (in contrast to DAVF, which occurs between 40-70 years of age)
- considering treatment options, it is essential to determine
- number of feeding arteries
- size of the nest
- type of drainage (superficial or deep vein system)
Classification
- nidus composition
- compact (or glomerular) nidus: abnormal vessels without the interposition of normal brain tissue
- diffuse (or proliferative) nidus: no well-formed nidus is present; brain tissue is interspersed within the anomalous vessels
- The Spetzler-Martin arteriovenous malformation (AVM) grading system assigns points for various angiographic features to predict the risk of surgery
|
Spetzler-Martin AVM grading scale (grade I-V)
|
||
|
score
|
||
|
Nidus size – largest nidus diameter on angiography
|
1
2
3
|
|
|
The eloquence of the adjacent brain
|
0
1 |
|
|
Venous drainage → Anatomy of veins and sinuses
|
0
1
|
|
| Content available only for logged-in subscribers (registration will be available soon) |
Clinical presentation
- incidental finding in asymptomatic patients (~ 15%)
- intracerebral, intraventricular, and subarachnoid hemorrhage (40-65%)
- risk of bleeding 1-4%/year, risk of rebleeding about 20% in the first year
- risk factors:
- previous bleeding
- deep location and drainage
- concomitant aneurysm in the nidus or feeding arteries
- mortality is approx. 10% for the first bleeding and 20% for the third bleeding
- epileptic seizures (20-25%)
- headache (15%)
- focal neurologic deficits
- a consequence of bleeding, mass effect, or steal syndrome
- pulsatile tinnitus
Diagnostic evaluation
| Content available only for logged-in subscribers (registration will be available soon) |
Differential diagnosis
- other cerebral vascular malformations
- cerebral proliferative angiopathy (CPA)
- absence of early, extensive venous drainage
- involvement of an entire lobe or hemisphere as a diffuse network with normal neural tissue intermingled with the abnormal vessels
-
more common in females (2:1) and presents at a mean age of 20 years
- the risk of neurologic deficits after the surgical or endovascular treatment is substantial
- craniofacial arteriovenous metameric syndrome (CAMS)
- developmental venous anomaly (DVA)
- dural arteriovenous fistula (DAVF)
- cerebral proliferative angiopathy (CPA)
- malignant tumor
Management
- higher Spetzler-Martin grade ⇒ higher surgical risk
- grades 1 and 2: surgery is safe (good outcome in 95-100% of patients)
- grade 3 requires individual assessment
- grades 4 and 5 are associated with a high perioperative risk due to potential damage to the draining venous system that may serve both the AVM and surrounding healthy tissue. The alternative here is conservative management (good outcome in ~35%)
- other factors increasing the risk of bleeding:
- aneurysm in the feeding arteries or nidus
- venous stasis
Conservative therapy
| Content available only for logged-in subscribers (registration will be available soon) |
Surgery/endovascular treatment
| Content available only for logged-in subscribers (registration will be available soon) |