INTRACEREBRAL HEMORRHAGE
Intraventricular hemorrhage in adults
Updated on 08/10/2024, published on 22/08/2023
Introduction
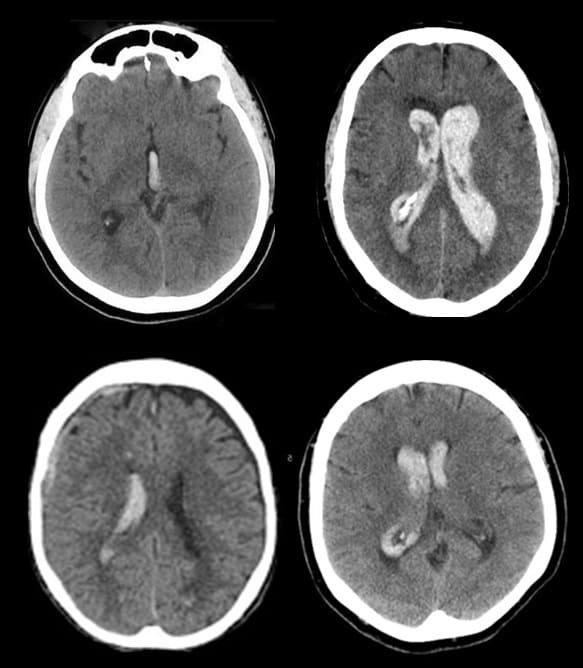
- intraventricular hemorrhage (IVH), also known as hemocephalus, is characterized by the presence of blood in the brain’s ventricles
- initially, IVH is present in one-quarter of patients with intracerebral hemorrhage (ICH) but may occur later as an extension of the ICH
- patients with larger hematomas or hemorrhages in the caudate nuclei or thalamic locations are more likely to bleed into the ventricles
- IVH significantly increases the risk of obstructive hydrocephalus, which in turn increases morbidity and mortality
- the volume of intraventricular hemorrhage is an important determinant of outcome
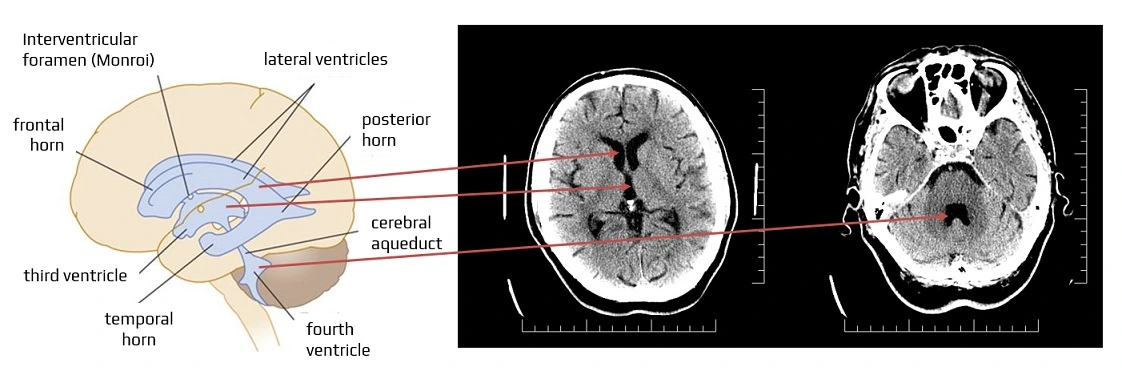
- the cerebral ventricular system consists of four interconnected cavities known as the cerebral ventricles (the lateral ventricles, the third ventricle, and the fourth ventricle)
- each ventricle contains a choroid plexus, which produces cerebrospinal fluid (CSF)
- the ventricular system continues from the fourth ventricle into the central canal of the spinal cord
- ventricles and the central canal are lined with ependymal cells, a specialized epithelium connected by tight junctions; these junctions form the blood-cerebrospinal fluid barrier
Classification and etiology
Primary IVH
Secondary IVH
- more frequent
- a significant extraventricular component (either parenchymal or subarachnoid) is present with secondary expansion to the ventricles
- propagation of intracerebral hematoma
- present in up to 45% of ICH patients [Hallevi, 2008]
- SAH (beware of possible reflux from the spinal SAH)
- trauma (Ravi, 2019)
- propagation of intracerebral hematoma
Clinical presentation
- in primary IVH, symptoms resemble those of SAH (sudden and severe headache and meningeal syndrome) → Clinical presentation of SAH
- in secondary IVH, signs and symptoms arise from the primary parenchymal lesion
- extensive hemorrhages may result in an altered level of consciousness with cardiorespiratory compromise
Diagnostic evaluation
MRI
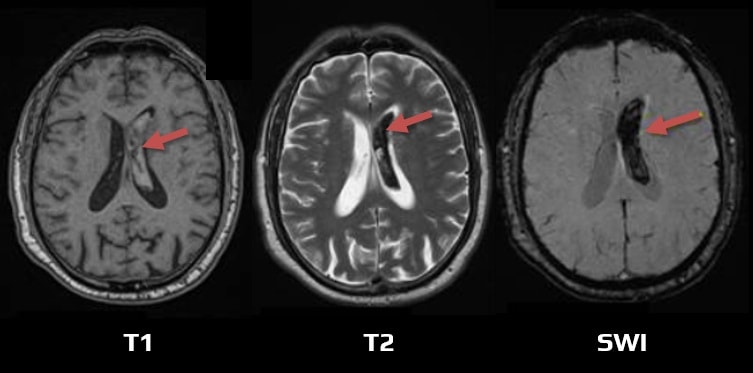
- MRI is sensitive to small amounts of blood, especially in the posterior fossa (CT may be inconclusive due to artifacts)
- FLAIR – signal intensity is time-dependent. Blood appears hyperintense in the first 48 hours; after that, the signal becomes more variable (exclude flow artifacts)
- GRE, or preferably SWI – detects even small amounts of blood in the occipital horns (characterized by a hypointense rim)
Vascular imaging (CTA, MRA, DSA)
- rule out vascular malformations, moyamoya, etc.
Management
- the recommended treatment is the same as the therapy used for intracerebral hemorrhage
- treat the underlying cause of bleeding
- detect and treat possible obstructive hydrocephalus (serial neurological status examinations and repeated CT scans are required for the diagnosis)
- external ventricular drainage (EVD) may reduce mortality, especially in patients with large ICH/IVH and impaired level of consciousness (LOC) (AHA/ASA 2022 1/B-NR)
- for patients with a GCS score >3 and primary IVH or secondary IVH (with supratentorial ICH of <30-mL volume) requiring EVD, minimally invasive IVH evacuation with EVD plus thrombolytics is safe and reasonable compared with EVD alone to reduce mortality (AHA/ASA 2022 2a/B-NR)
- for patients with a GCS score >3 and primary IVH or secondary IVH (with supratentorial ICH of <30-mL volume) requiring EVD, the effectiveness of minimally invasive IVH evacuation with EVD plus the use of thrombolytics to improve functional outcomes is uncertain
- for patients with large ICH/IVH and impaired LOC, the efficacy of EVD to improve functional outcome is not well-established
- intraventricular application of tPA may facilitate the thrombus evacuation from the ventricles; it appears safe, but clinical efficacy is unclear
- CLEAR-IVH study – systemic bleeding 4%, ventriculitis 2%
- CLEAR III trial – no substantial improvement in functional outcome at mRS 3 cutoff compared to saline irrigation; mortality reduced by 10%
- intraventricular tPA protocol – 1 mg of alteplase, 8h apart; up to 12 doses
- alternative procedures: endoscopic evacuation of the hematoma with ventriculostomy, VP shunt, or lumbar drainage – benefit is unclear (AHA/ASA 2022 2b/C-LD)
- external ventricular drainage (EVD) may reduce mortality, especially in patients with large ICH/IVH and impaired level of consciousness (LOC) (AHA/ASA 2022 1/B-NR)