ADD-ONS / OTHER VASCULAR DISORDERS
Transient monocular vision loss
Updated on 01/02/2024, published on 11/07/2023
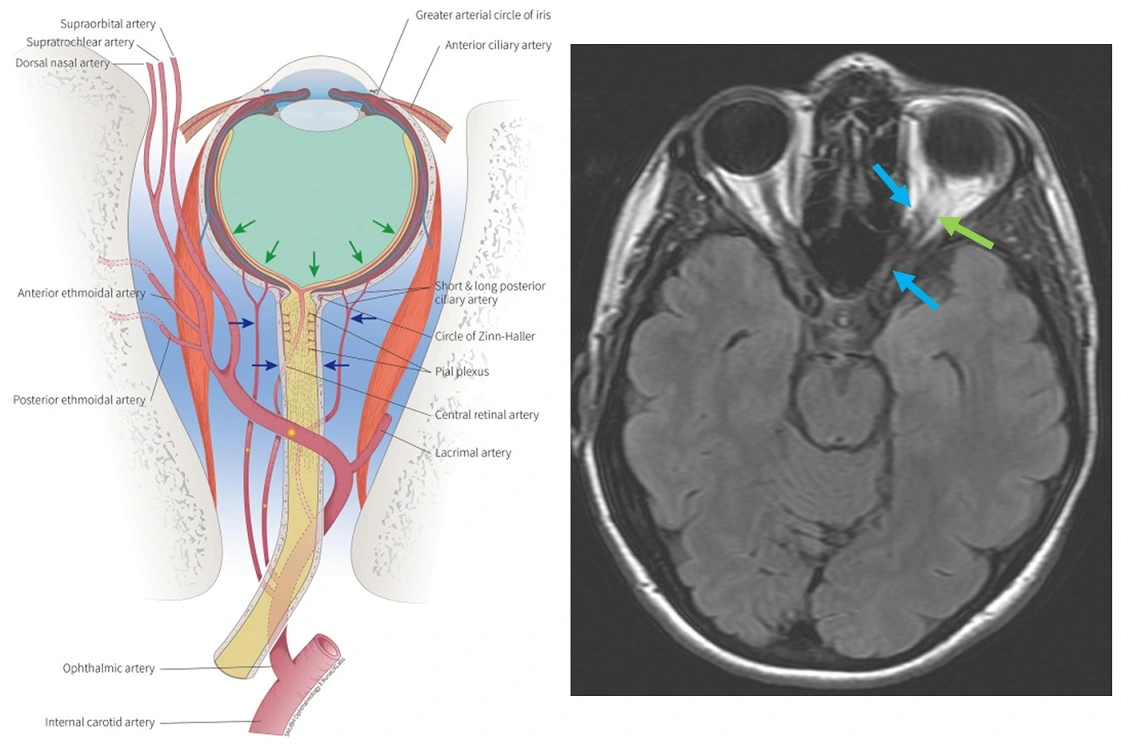
- ophthalmic artery (OA) is the first major branch of the internal carotid artery (ICA), and it usually arises from its supraclinoid segment
- various anomalies of OA origin have been reported (from the cavernous segments of the ICA, MCA, PCoA, or middle meningeal artery)
- OA diameter is ~ 1 mm
- various anomalies of OA origin have been reported (from the cavernous segments of the ICA, MCA, PCoA, or middle meningeal artery)
- OA passes through the dura and enters the orbit via the optic canal, where it runs inferolateral to the optic nerve
- the artery has numerous branches:
- the first branch central retinal artery (CRA) arises just before the ophthalmic artery crosses over the optic nerve; it enters the lower part of the optic nerve and divides into 2 superior and 2 inferior terminal branches
- the OA then crosses over the optic nerve to the medial side and gives off the remaining branches, which may be grouped into those supplying the orbital structures and those supplying the eye; terminal branches are the supratrochlear artery and the dorsal nasal artery
- orbital group
- lacrimal artery (the second and the largest branch)
- supraorbital artery
- posterior ethmoidal artery
- anterior ethmoidal artery
- internal palpebral artery
- supratrochlear artery (frontal artery) and dorsal nasal artery (terminal branches)
- ocular group
- posterior ciliary arteries (including cilioretinal artery) – pass through the sclera and supply the posterior uveal tract
- short posterior ciliary arteries from six to twelve in number
- long posterior ciliary arteries, two for each eye, pierce the posterior part of the sclera a short distance from the optic nerve
- anterior ciliary artery
- muscular branches
- posterior ciliary arteries (including cilioretinal artery) – pass through the sclera and supply the posterior uveal tract
- orbital group
"DR MCLESSI" mnemonic
R = [Central] Retinal Artery
M = Muscular Artery
C = Ciliary Arteries [Long / Short / Anterior]
L = Lacrimal Artery
E = Ethmoidal Arteries [Anterior / Posterior]
S = Supraorbital Artery
S = Supratrochlear Artery [Frontal]
I = Internal Palpebral Artery
- the term transient vision loss is used for episodes of reversible visual disturbances lasting < 24 h; it may be monocular or binocular
- monocular loss (most common) is most commonly caused by lesions anterior to the chiasm, usually due to retinal, choroidal, or optic nerve ischemia.
- binocular loss may be of chiasmal or retrochiasmal origin (incl. bioccipital lesions, etc.), or it may be due to the bilateral involvement of the eyes or optic nerve
- monocular transient vision loss is also called amaurosis fugax
- this term is usually used when a vascular etiology is suspected
- such disorder is also classified as a transient ischemic attack (TIA)
- it usually lasts from seconds to minutes, followed by a full recovery of vision
- transient vision loss may be a harbinger of impending stroke ⇒ proper and urgent evaluation is mandatory to find the underlying cause and treat it appropriately
Etiopathogenesis
- monocular loss of vision can be caused by several etiologies that can be classified as:
- vascular (the unifying mechanism is hypoperfusion of the retina/optic nerve)
- most commonly, an embolus transiently occludes the central or branch retinal arteries or the ophthalmic artery
- if the ischemia targets the optic nerve, it is usually due to decreased perfusion of one or more posterior ciliary arteries
- nonvascular
- vascular (the unifying mechanism is hypoperfusion of the retina/optic nerve)
- different mechanisms may combine (e.g., significant carotid stenosis + hypotension, etc.)
→ differential diagnosis of visual disorders see here |
Clinical presentation
- usually negative visual symptoms, typically lasting from seconds to minutes (even longer episodes have been reported)
- positive visual symptoms (although typical for migraines) do not rule out an ischemic etiology
Diagnostic evaluation
Medical history
- check the patient´s medical history
- search for provoking factors and associated symptoms
- transient visual loss induced by gaze may suggest an orbital lesion
- hemiparesis is suggestive of a source proximal to the OA (most commonly carotid stenosis or cardioembolism)
- multiple infarcts or posterior circulation stroke may suggest cardioembolism
- headaches, jaw claudication, scalp tenderness, fever, polymyalgia rheumatic, etc., point to temporal arteritis
- verify that the vision loss is truly monocular
- determine the nature of the visual impairment
- complete blindness (often OA or CRA occlusion)
- partial (quadrant, central, paracentral, or altitudinal defect); constriction of the peripheral visual field is usually due to nonvascular etiology
- the curtain sensation (ascending, descending)
- positive phenomena at the onset? (migraine)
- duration of visual loss
- very short attack (e.g., acute decompensation of papilledema)
- 1-10 minutes (temporal arteritis or embolization to OA or CRA) → CRA occlusion
- 5-20 minutes (often retinal migraine; usually with some initial positive visual phenomena)
- recurrent retinal claudication (exclude carotid stenosis)
Imaging, physical examination, laboratory studies
Differential diagnosis
| Content available only for logged-in subscribers (registration will be available soon) |
Management
- management is directed to the underlying cause
- some causes of cardioembolism (e.g., AFib) are treated with anticoagulants
- ICA stenosis may be managed with antiplatelet therapy + risk factors treatment; significant stenoses should be treated with carotid endarterectomy or carotid stenting
- temporal (giant cell) arteritis is managed with corticosteroids
- retinal vasospasms could be treated with aspirin or calcium channel blockers
- a retinal migraine is controlled with conventional migraine treatments
- angle-closure glaucoma is also treated with standard therapies for this condition