OTHER VASCULAR DISORDERS / OCULAR VASCULAR DISORDERS
Retinal vein occlusion (RVO)
Updated on 26/02/2024, published on 29/04/2022
| Ocular vascular disorders |
| Ischemic optic neuropathy (ION) |
|
|
Central retinal vein occlusion (CRVO) → more |
|
|
Hemi-central retinal vein occlusion (HCRVO) |
|
|
Branch retinal vein occlusion (BRVO) |
|
|
Central retinal artery occlusion (CRAO) |
|
|
Branch retinal artery occlusion (BRAO) |
|
|
Cilioretinal artery occlusion |
- retinal vein occlusion (RVO) is the second most common retinal vascular disease after diabetic retinopathy
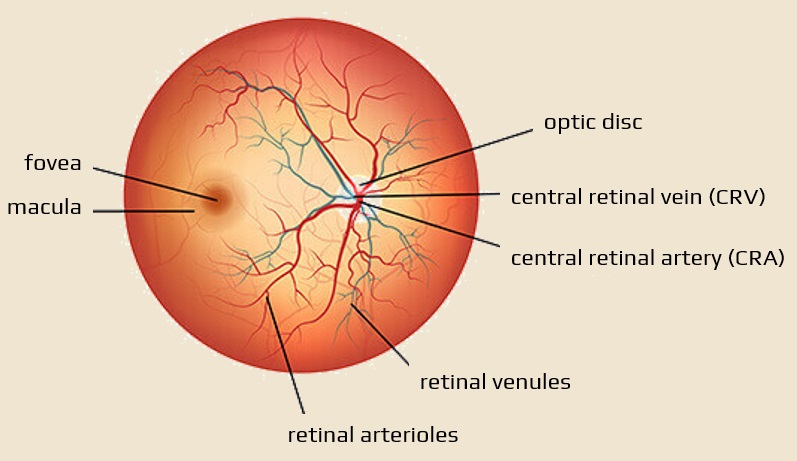
- it may affect the central retinal vein (CRVO) or its branches (HCRVO, BRVO)
- the most common clinical presentation is unilateral and painless loss of vision, usually caused by macular edema (with or without concurrent macular ischemia)
- branch RVO may present with peripheral visual field defects or may be asymptomatic
- the speed of vision loss varies depending on the extent and location of the occlusion and the presence of associated complications; commonly over a period of hours
- prognosis depends on the extent of the initial visual defect
- better for branch RVO than for central RVO
- late complications may occur: vitreous hemorrhage, retinal detachment, or glaucoma
- risk of recurrence is significant (in the same or the fellow eye)
Etiology and pathophysiology
The three main factors contribute to retinal vein thrombosis:
- reduced venous outflow with venous stasis
- increased intraocular pressure in glaucoma may compromise retinal venous outflow
- atherosclerotic retinal artery may compress the vein
- endothelial damage
- hypercoagulable states
Common risk factors:
- age (usually patients older than 50 years
- arterial hypertension
- open-angle glaucoma
- diabetes mellitus
- hyperlipidemia
Other associated conditions:
- smoking
- optic disc drusen or edema
- hypercoagulable state
- polycythemia, multiple myeloma, cryoglobulinemia, Waldenstrom macroglobulinemia, antiphospholipid syndrome, Leiden factor V, APC resistance, hyperhomocysteinemia, protein C and S deficiency, antithrombin III mutation, prothrombin mutation
- infection
- syphilis
- HIV infection
- sarcoidosis
- sickle cell disease
- vasculitis
- drugs (oral contraceptives, diuretics)
- abnormal platelet function
- orbital diseases
- vein thrombosis provokes increased production of vascular endothelial growth factor (VEGF)
- this leads to swelling and neovascularization with bleeding
- treatment involves intravitreal injections of an anti-VEGF drug to reduce the new blood vessel growth and swelling
Clinical presentation
| Content available only for logged-in subscribers (registration will be available soon) |
Diagnostic evaluation
- extensive laboratory workup is needed to determine the cause
- standard laboratory tests include:
- complete blood count (CBC)
- erythrocyte sedimentation rate (ESR), C-reactive protein (CRP)
- blood glucose
- total cholesterol, LDL, and HDL
- plasma protein electrophoresis (to exclude multiple myeloma)
- BUN and creatinine
- electrolytes
- thyroid function tests
- extended laboratory tests (patients < 50 years of age, those with bilateral retinal vein occlusion, history of the previous thrombosis, or a family history of thrombosis)
- chest x-ray
- thrombophilia screening
- autoantibodies (rheumatoid factor, antinuclear antibodies, anti-DNA antibodies)
- serum angiotensin-converting enzyme (ACE) level
- plasma homocysteine level
-
ECG (left ventricular hypertrophy secondary to hypertension)
- check blood pressure
- Duplex carotid ultrasound (exclusion of ocular ischemic syndrome)
Differential diagnosis
-
arterial ischemic syndrome
-
proliferative diabetic retinopathy
-
hyperviscosity retinopathy → hyperviscosity syndrome
Management
Ophthalmologic therapy
- no fully effective medical treatment is available to prevent or treat central retinal vein occlusion
- medical treatments (with varying efficiency):
- antithrombotic therapy
- antiplatelet therapy (aspirin)
- anticoagulant therapy
-
anti-inflammatory agents
-
isovolemic hemodilution
-
plasmapheresis
-
fibrinolytic agents
-
systemic corticosteroids
-
intravitreal injection of
-
alteplase
-
ranibizumab
-
triamcinolone
-
bevacizumab
-
- antithrombotic therapy
-
surgical interventions:
-
laser photocoagulation
-
chorioretinal vein anastomosis
-
radial optic neurotomy
-
pars plana vitrectomy
-
Antithrombotic and thrombolytic therapy
| Content available only for logged-in subscribers (registration will be available soon) |
Prognosis
- prognosis correlates with the initial degree of visual impairment
- in visual acuity < 20/200, improvement is unlikely
- if visual acuity is > 20/60, it is likely to remain unchanged
- chronic macular edema and macular ischemia are the main causes of poor vision
- better prognosis can be expected in younger patients and those without ischemia
- 1/3 of older patients improve without treatment, 1/3 stay the same, and 1/3 get worse
- complications:
- iris neovascularization (~ 60% of cases) ⇒ neovascular glaucoma
- retinal neovascularization
- vitreous hemorrhage



