ADD-ON / MEDICATION / ANTICOAGULANT THERAPY
Neutralization of the anticoagulant effects
Updated on 21/03/2024, published on 04/02/2022
Indications for modification/discontinuation of anticoagulant therapy
- anticoagulation reversal in acute bleeding (including intracranial hemorrhage)
- the annual risk of ICH for VKA is 0.3-0.6% and 0.1-0.2% for DOAC [Schlunk, 2015]
- anticoagulated patients (warfarin > DOAC) are at ↑ risk of prolonged bleeding (in about 30-50% of cases) → spot sign in ICH
- anticoagulation reversal before IV thrombolysis (→ see chapter on recanalization therapy in the anticoagulated patients)
- temporary discontinuation of anticoagulation before a surgical procedure
- emergency surgery
- elective procedure → see separate chapter
- dose adjustment in case of overdose (based on laboratory tests)
Categorization of bleeding complications
- for the management of hemorrhagic complications, it is essential to assess the severity of bleeding
|
Severe bleeding
|
|
|
Life-threatening bleeding
|
|
Low molecular weight heparins (LMWHs)
- protamine only partially neutralizes the anticoagulant effect of LMWH
- ∼ 60–75% of the anti-Xa activity of enoxaparin is neutralized; effectiveness depends on the specific LMWH agent used
- ∼ 60–75% of the anti-Xa activity of enoxaparin is neutralized; effectiveness depends on the specific LMWH agent used
- dosing depends on timing since the last dose of LMWH (see table)
- vial/5mL/50mg/5000IU + 100mL of NS administered by a short IV infusion (over 5-10 minutes
- DO NOT EXCEED 5mg/minute !!
- max dose 50 mg/10 min
- dosing should ideally be guided by anti-Xa levels, if available
- AEs: anaphylaxis, hypotension, bradycardia to arrest, flush
- close monitoring is required, and protamine should be administered in a setting where emergency resuscitation measures are available
|
Protamine (amp = 1ml/10mg/1000IU)
|
||
|
nadroparin
(FRAXIPARIN) 1ml/9500IU |
< 8 h
(since the last dose) |
6 mg/0,6mL for 950UI antiXA of nadroparin (0,1 ml) |
| > 8h | do not use |
|
|
enoxaparin
(CLEXANE, LOVENOX) 1ml/10000IU/100mg
|
< 8 h
|
10mg/1mL for 1000UI anti-Xa of enoxaparin (0,1 mL) 1 mg protamine per 1 mg enoxaparin |
|
8-12 h
|
half dose
|
|
| > 12h | protamin likely not needed |
|
- andexanet alfa is not useful (Lewis, 2021)
Unfractioned heparin (UFH)
| Content available only for logged-in subscribers (registration will be available soon) |
Fondaparinux
- fondaparinux (ARIXTRA) reversal is challenging because there is no specific antidote
- andexanet alfa and protamin seem to be ineffective in neutralizing the anti-Xa effects of fondaparinux (Siddiqui, 2019)
- fondaparinux is not significantly removed by dialysis (due to its large molecular size and strong protein binding)
- in cases of fondaparinux-related hemorrhage, consider coagulation factors supplementation; limited data are available on recombinant factor VIIa and PCC; both drugs may be used as off-label therapy
Warfarin
- significant bleeding → check INR; if in therapeutic range, administer IV vitamin K + start substitution therapy
- asymptomatic overdose → proceed according to current INR
| Warfarin overdose without bleeding |
|
|
slight increase in INR
|
|
|
INR 3 -5
|
|
|
INR 5 – 9
|
Low risk of bleeding
High risk of bleeding
|
|
INR over 9
|
Low risk of bleeding
High risk of bleeding
|
|
any bleeding with a subtherapeutic INR level
|
|
Effectiveness of therapies for the correction of elevated INR
| Content available only for logged-in subscribers (registration will be available soon) |
Direct Oral Anticoagulants (DOACs)
- assess the severity of the bleeding (mild, moderate, severe) and the patient’s general condition, especially blood pressure, pulse, O2 saturation
- secure the source of bleeding, apply local hemostatic measures
- mechanical compression, local hemostatics, endoscopic or surgical hemostasis
- order CBC + coagulation tests (if available, request DOAC-specific tests)
- consider transfusion for severe anemia
- replenish fluids
- start hemodynamic support in cases of major bleeding
- obtain personal medical history:
- medications+doses, time since the last DOAC administration
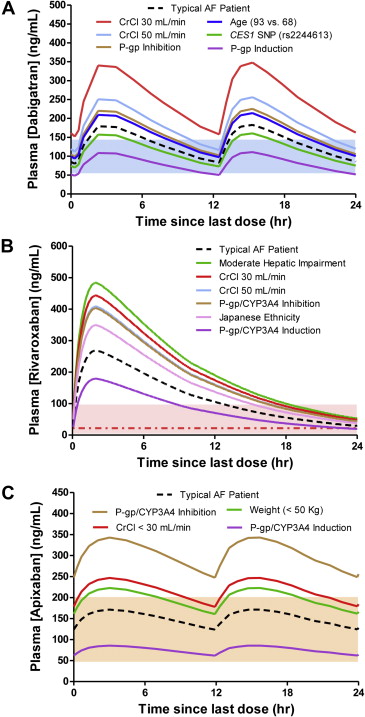
- estimate DOAC elimination time according to ClCr and coagulation test results
- other medications + comorbidities
- antifibrinolytics (tranexamic acid or epsilon-aminocaproic acid) are considered off-label therapy for major DOAC-associated bleeding
| Content available only for logged-in subscribers (registration will be available soon) |
| Planned discontinuation of DOAC with regard to renal function and procedural bleeding risk |
||||||||
| Dabigatran | Rivaroxaban / Apixaban / Edoxaban | |||||||
|
bleeding risk
|
low
|
high
|
low
|
high
|
||||
| CrCl (mL/min) | ||||||||
| ≥ 80 | ≥ 24h | ≥48h | ≥ 24h | ≥48h | ||||
| 50-80 | ≥ 36h | ≥72h | ≥ 24h | ≥48h | ||||
| 30-50 | ≥48h | ≥96h | ≥ 24h | ≥48h | ||||
| 15-30 | KI | KI | ≥ 36h | ≥ 48h | ||||
| <15 | DOAC contraindicated | |||||||
| Mild bleeding |
|
| Moderate bleeding |
|
| Severe, life-threatening bleeding |
|
Follow-up procedures
- recheck coagulation parameters (choose appropriate test according to type of anticoagulant)
- if correction is sufficient, repeat the test in 4-6 hours
- if correction is not sufficient, consult a hematologist
- in the case of overdose, assess the probable cause
- comorbidities, drug interactions, non-compliance
- consider DVT prevention according to the degree of actual thromboembolic risk