CEREBRAL VENOUS SINUS THROMBOSIS
Clinical presentation and etiology of cerebral venous sinus thrombosis
Updated on 12/03/2024, published on 07/04/2021
Introduction
- cerebral venous sinus thrombosis (CVST) refers to the presence of a thrombus in the dural venous sinuses and/or cerebral veins, which are responsible for draining blood from the brain
- CVST accounts for approx. 1-3% of all strokes, with women being affected in 70% of cases (Alet, 2020)
- when diagnosed early and managed adequately, CVST has generally a favorable prognosis
- factors associated with poor prognosis include advanced age, active cancer, decreased level of consciousness, and intracerebral hemorrhage
- the diagnosis of early stages can be challenging, primarily due to the highly variable and non-specific clinical manifestations
- thrombosis results in intracranial hypertension and/or venous infarction (with or without a hemorrhagic component)
- unrecognized venous thrombosis was formerly a common cause of misdiagnosed “pseudotumor cerebri”
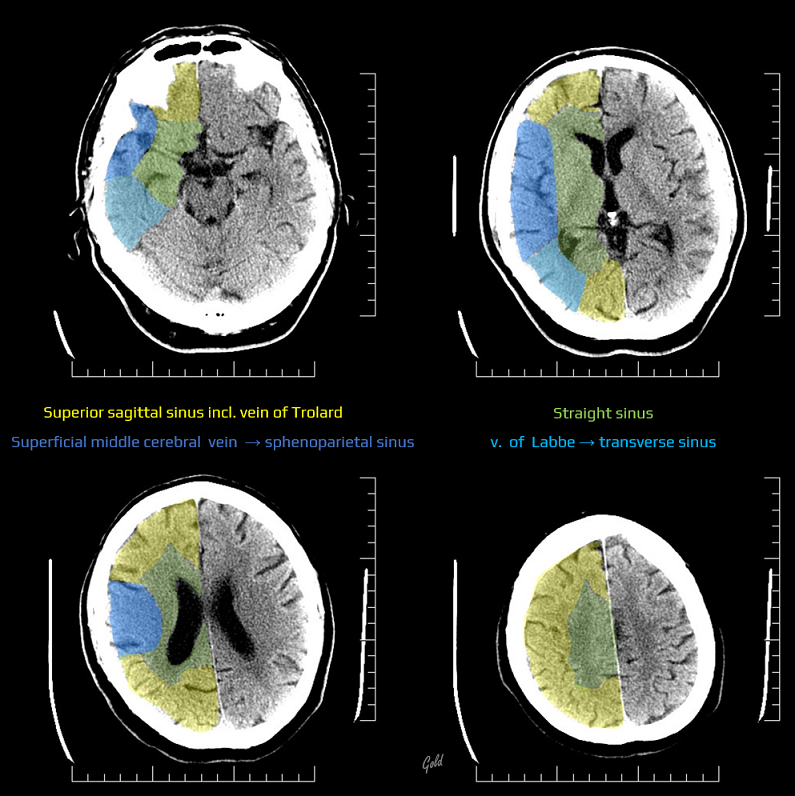
The most common sites of symptomatic thrombosis:
- transverse sinus
- sigmoid sinus
- superior sagittal sinus
- deep venous system
- straight sinus
- cavernous sinus
Etiology
- the most common causes:
- inherited hypercoagulable states (~ 22% of cases)
- pregnancy and the puerperium
- use of oral contraceptives
- malignancy
- combination of multiple factors is commonly observed
- in ~ 10-37% of cases, no obvious risk factor or etiology is identified
Risk factors
| Content available only for logged-in subscribers (registration will be available soon) |
Pathophysiology
- venous thrombosis impairs venous drainage → increased intravenous and intracapillary pressure
- consequences:
- impaired perfusion → cytotoxic edema and the development of venous infarction
- rupture of veins and capillaries → parenchymal hematoma
- blood-brain barrier (BBB) dysfunction → vasogenic edema
- impaired cerebrospinal fluid (CSF) absorption
⇓
intracranial hypertension
- in the absence of focal symptoms and with clinically predominant intracranial hypertension syndrome accompanied by papilledema, the diagnosis of pseudotumor cerebri (benign intracranial hypertension) can only be established after the careful exclusion of cerebral venous thrombosis!
Clinical presentation
- search for the provoking conditions (listed in the table above) in the patient’s personal history
- signs and symptoms of CVST result from intracranial hypertension (causing headache or mental changes) and/or parenchymal lesion (venous infarct +/- hemorrhage), manifesting as focal neurological deficit or seizures
- the most common and usually initial symptom is headache (80-90%), often accompanied by nausea and vomiting
- isolated intracranial hypertension syndrome occurs in 20-40% of cases
- symptoms typically worsen during Valsalva maneuvers (coughing, sneezing, or bending over)
- there is no clear correlation between the location of pain and the site of thrombosis
- the headache in CVST can mimic tension-type or migraine headaches, making diagnosis challenging in the absence of focal symptoms
- papilledema
- transient visual obscurations or vision loss; papilledema carries the risk of permanent vision loss!
- most pronounced in thrombosis involving the sagittal and/or cavernous sinuses
- altered level of consciousness or encephalopathy
- rapid deterioration of consciousness indicates either decompensated intracranial hypertension or extension of thrombosis into the deep venous system; herniation syndromes may occur
- disturbances of consciousness in the initial stages are usually due to deep venous involvement (with typical bithalamic involvement)
- always consider the possibility of nonconvulsive status epilepticus (NCSE)
- rapid deterioration of consciousness indicates either decompensated intracranial hypertension or extension of thrombosis into the deep venous system; herniation syndromes may occur
- focal neurological deficits occur in ~ 50% of patients (in more advanced stages when ischemia or hemorrhage has developed) – a sudden worsening is probably caused by hemorrhagic transformation of ischemia
- cranial neuropathies
- visual field disturbances (in cases involving the Labbe vein)
- epileptic seizures (~ 20-40%, often accompanied by Todd’s hemiparesis)
- common in cortical vein involvement
- sinus thrombosis rarely presents initially as a subarachnoid hemorrhage
[Sharma, 2010] [Oppenheim, 2005]
- rupture of dilated feeding veins due to retrograde intravenous hypertension
- secondary rupture of the hemorrhagic venous infarct into the subarachnoid space
- ⇒ in a small SAH with no detectable aneurysm, it is helpful to include MRV in the diagnostic workup
- obstructive hydrocephalus
- a rare complication
- usually caused by an intraventricular extension of a thalamic hematoma caused by the thrombosis of internal veins
- focal motors seizures, sometimes generalized
- focal hemispheric symptoms (neglect, impaired symbolic functions, hemiparesis)
- impaired consciousness in cases of extensive thrombosis (due to intracranial hypertension)
- increased risk of temporal herniation (with ipsilateral mydriasis, contralateral hemiparesis)
- middle ear affections or mastoiditis are the most common cause of transverse and sigmoid sinus thrombosis, especially in patients with fever
- epileptic seizures
- aphasia in cases of dominant hemisphere involvement
- cranial nerves palsies
- retrobulbar and eye pain due to:
- edema and congestion
- trigeminal nerve irritation
- exophthalmos
- massive conjunctival injection and swelling
- papilledema and fundus hemorrhage
- visual disturbance (including blindness)
- aseptic cavernous sinus thrombosis is rare; it most often occurs secondary to orbital, paranasal sinus, or facial inflammation
- in DDx, exclude carotid-cavernous fistula!
- qualitative/quantitative alteration of the level of consciousness (LOC)
- prognosis is serious due to potential bithalamic involvement
- edema of the structures around the tentorium may lead to brain herniation
- focal epileptic seizures
- motor/sensory deficits
Late complications
- chronic headaches
- stroke-related seizures
- recurrence of CVST
- visual loss
- dural arteriovenous fistula (DAVF)
- the consequence of persisting sinus occlusion with increased venous pressure
- preexisting DAVF can be the cause of CVST
- long-term cognitive impairment (rare)
Prognosis
- cerebral venous thrombosis generally has a more favorable prognosis than arterial stroke, particularly when diagnosed and treated promptly
- various factors influence outcome:
- extent of the thrombosis
- cause
- timely and appropriate therapy
- presence of complicating factors such as hemorrhagic conversion or elevated intracranial pressure
- according to the ISCVT study (International Study on Cerebral Vein and Dural Sinus Thrombosis)
- 57.1% of patients were symptom-free (mRS=0), 22% had minor residual symptoms (mRS=1)
- 7.5% had mild impairments (mRS=2), 5.1% were moderately or severely impaired (mRS=3-5)
- 8.3% had died (mRS=6)
- seizures ~ 10.6% of patients
- risk of recurrence ~ 2.2%
- mortality in the acute phase is 0.4-13% according to various studies
- risk of deterioration in the first week after admission ~ 23%
- recanalization: 84% at 3 months and 85% at 12 months (De Sousa, 2018)
- positive predictors of recanalization are the female sex and thrombosis of the superior sagittal sinus
- for a list of adverse prognostic factors, refer to the table and CVT risk score below)
| Unfavorable prognostic factors | |||
|
Demographic data
|
Clinical presentation and course
|
Imaging methods
|
Other risk factors
|
|
male sex
age > 37 y
|
initial coma (GCS) severe neurological deficit encephalopathy seizures rapid progression |
intracerebral hemorrhage extensive thrombosis involving multiple sinuses or deep venous systems venous infarction with hemorrhagic component |
malignancy CNS infection coagulopathy sepsis systemic inflammation |