ISCHEMIC STROKE / CLASSIFICATION AND ETIOPATHOGENESIS
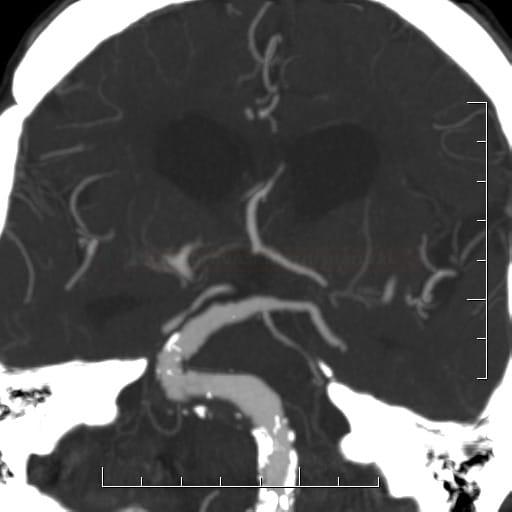
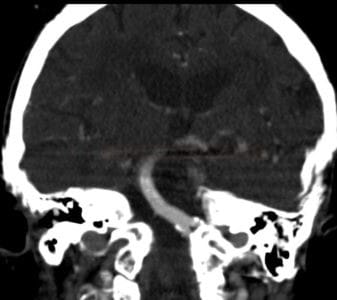
Dolichoectasia
Updated on 07/11/2023, published on 16/12/2021
What is dolichoectasia?
- a progressive disease characterized by elongation, dilation and tortuosity of the arteries, sometimes called dilated arteriopathy
- the vertebrobasilar arteries are most commonly affected (also known as vertebrobasilar dolichoectasia or megadolichobasilar artery)
- (pseudo)aneurysm, on the other hand, is characterized by a focal dilation, creating a weakened area prone to rupture
- incidence 0.06-6% [Brutto, 2021]
- associated with increased risk of stroke recurrence (up to 19%/2 years) [Chen, 2019]
- likely cause of a fraction of strokes initially classified as cryptogenic [Brutto, 2021]
- the following characteristics also apply to large fusiform aneurysms
Pathophysiology
dolichoectasia may lead to:
- ischemic stroke through
- thrombus formation (due to slowed flow)
- occlusion of perforators
- distal embolization
- atherosclerotic plaques with stenosis or occlusion of penetrating (perforating) arteries
- possible combination with thrombosis
- distortion of the origin of the penetrating artery due to tortuosity
- thrombus formation (due to slowed flow)
- intracranial hemorrhage (ICH) or subarachnoid hemorrhage (SAH)
- due to rupture of the fragile wall l (risk 20 times higher than in the general population)
- risk factors: hypertension, antiplatelets/anticoagulants, the extent of lateral artery displacement
- compression syndrome may affect the brainstem and/or cranial nerves
Etiology
- atherosclerosis (atherosclerotic dolichoectasia)
- affects both intra- and extracranial arteries
- usually occurs in individuals aged > 40 years
- the combined effect of increased age, chronic hypertension with arterial wall remodeling, and chronic inflammation that may weaken the arterial wall; typical vascular risk factors are present
- congenital disorders (non-atherosclerotic dolichoectasia)
- individuals aged < 40 years; more common in women
- distal branches of the posterior circulation are typically affected
- Marfan syndrome, Ehlers-Danlos, Fabry disease
- can develop as a complication of arterial dissection
Clinical presentation
- ischemic stroke/TIA (30% risk over 5 years)
- intracranial bleeding, subarachnoid hemorrhage
- compressive phenomena
- brainstem compression (associated with basilar dolichoectasia)
- hydrocephalus
- neurovascular compression syndrome (NVCS)
- compression of the optic nerve near the optic chiasma (ICA)
- impairment of one or more cranial nerves is associated with a tortuous and elongated BA (CN VII, VIII, VI)
- factors influencing clinical outcome:
- severity of arterial dilation and the extent of lateral shift
- signs and symptoms at the time of diagnosis
- presence of intraluminal mural thrombus
- progression of ectasia on follow-up imaging
Management
- due to the potential for significant morbidity, a multidisciplinary approach involving neurologists, vascular surgeons, and radiologists is often recommended for comprehensive management and prognostic assessment
- there is no universally accepted treatment with proven benefit
- serial imaging to monitor disease progression is suggested
- patients with previous stroke/TIA may receive antiplatelet therapy or anticoagulation (AHA/ASA 2021 2a/L-CD)
- in primary prevention, the benefit of antiplatelet/anticoagulant therapy is uncertain
- intervention/surgery is reserved for symptomatic cases; the benefit is uncertain (better results in the anterior circulation)
- bypass
- resection with anastomosis
- transposition
- endovascular flow diverter/stent placement with or without additional coiling
- lifestyle modifications + management of vascular risk factors, especially hypertension
- intravenous thrombolysis or mechanical thrombectomy are not contraindicated in acute stroke
Prognosis
- variable nature of the disease with asymptomatic to malignant course
- progression more common in younger patients with anterior circulation ectasia
- relatively high risk of stroke recurrence (up to 60% over 11 years)