NEUROIMAGING / NEUROSONOLOGY
TCD/TCCD bubble test
Updated on 06/05/2024, published on 13/01/2023
Indications
- the TCD/TCCD bubble test (bubble study) is designed for the detection of right-to-left shunts, particularly Patent Foramen Ovale (PFO)
- a cost-effective, safe, and non-invasive imaging modality ideal for screening purposes
Bubble study procedure
- the test simulates a paradoxical embolism
- an embolus (thrombus, gas, fat) passes through an intracardiac defect (or any other A-V shunt) and enters the systemic circulation, incl. the brain
- an embolus (thrombus, gas, fat) passes through an intracardiac defect (or any other A-V shunt) and enters the systemic circulation, incl. the brain
- with the patient in the supine position, a blue cannula (22G) is inserted into the cubital vein and connected to a 3-way stopcock via a flexible tube
- two 20 mL syringes are connected: one containing 8 mL of saline solution + 1 mL of blood and the other containing 1 mL of air (final mixture = 8:1:1) (Zetola, 2019)
- this air dose is safe; in animal models, a threatening air dose is a bolus of > 20 mL or 11 mL/min [Tsivgoulis, 2010]
- some authors mix NS with blood immediately, while others mix NS + air first and then draw 1 mL of blood to stabilize the mixed suspension
- mix the contents of both syringes (perform at least 10 exchanges between syringes)
- inject the bolus of agitated solution (10 mL) while monitoring the flow in the MCA (ideally in both MCA and ACA)
- in cases of an impenetrable temporal window, the terminal ICA may be examined transorbitally, or HITS may be detected in the extracranial portion of the CCA/ICA
- bilateral monitoring with a fixation frame increases sensitivity
- the suspension is applied twice, first during normal breathing and then during the Valsalva maneuver (which increases the pressure in the right atrium and thus the functionality of the shunt)
- the quality of the Valsalva maneuver should be checked beforehand (verify ↓ PSV in MCA > 30% during the maneuver)
- initiate the Valsalva maneuver approx. 5s after administration of the suspension
- repeated testing increases sensitivity

Definition of HITS
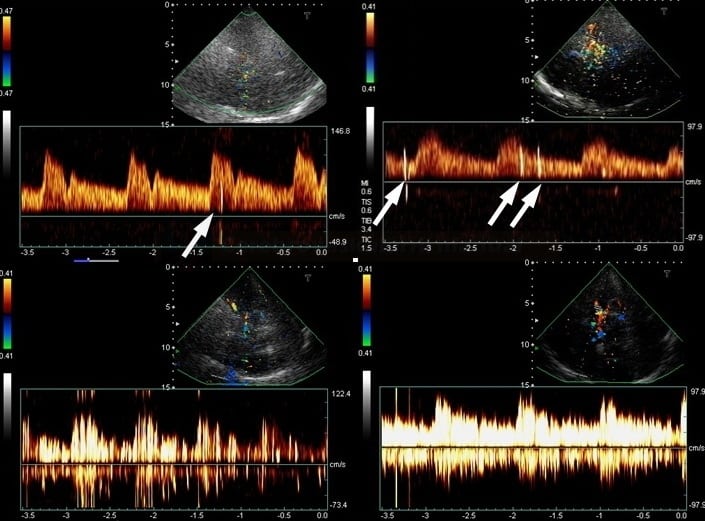
- if bubbles pass from the right atrium into the left atrium via the PFO (or other shunts) and then enter the monitored cerebral artery, they manifest as High-Intensity Transient Signals (HITS) on the TCD/TCCD due to the reflection of the ultrasound signal
- characteristics of HITS:
- unidirectional
- accompanied by a typical audible sound
- duration < 300 milliseconds (usually 2-100ms)
- amplitude >3 dB above the background (3-60 dB)
- when insonated simultaneously at different depths, the HITS shift in time (as the bubbles travel through the artery)
- always record the timing of the first HITS
- HITS recorded in the first 30 seconds of monitoring indicate the presence of a right-to-left shunt
- PFO: usually < 12s
- extracardiac shunts: >15-20s
Test evaluation
|
Assessment of the right-to-left shunt severity
|
||
|
grade
|
number of HITS
|
evaluation |
|
I
|
0
|
negative test |
|
II
|
1-10
|
low-grade shunt |
|
III
|
> 10
|
medium-grade shunt |
|
IV
|
“shower” or “curtain”
|
high-grade shunt |
|
permanent
latent – shunt is present only during and after the Valsalva maneuver
|
||
Specificity and sensitivity
- the sensitivity and specificity of both TCD and TCCD are reported to be > 90%
- repeated/bilateral testing increases both sensitivity and specificity
- repeated/bilateral testing increases both sensitivity and specificity
- false-positive results:
- the test is not PFO specific; it can be positive in the presence of any right-to-left communication (intraventricular septal defects, intrapulmonary AV shunt, etc.).
- false-positive results may be obtained if the monitoring duration is too long (some bubbles may be detected after passing through the pulmonary circulation) → see the timing of the HITS above
- certain modifications of the bubble test can increase the sensitivity, such as mixing the air suspension with blood to stabilize the microbubbles, as previously described)